Transcription
Obsessive Compulsive Disorder:Evidenced-Based Strategies thatWork!Dr. Robin Zasio, Psy.D., LCSWThe Anxiety Treatment Center ofSacramento, Roseville, and El DoradoHills
Scaredy Guy
Anxiety Disorders (DSM IV) Obsessive Compulsive DisorderSocial PhobiaPanic Disorder with or without agoraphobiaPosttraumatic Stress DisorderGeneralized Anxiety DisorderSpecific Phobia
Anxiety Related Conditionsl Body Dysmorphic Disorder (Somotoform)l Hoarding (No category)l Trichotillomania (Impulse Control)l Skin Picking (No Category)
DSM VObsessive Compulsive and Related Disordersl Obsessive Compulsive Disorderl Body Dysmorphic Disorderl Hoarding Disorderl Trichotillomanial Excoriation
DSM VAnxiety Disordersl Separation Anxiety Disorderl Selective Mutisml Specific Phobial Social Anxiety Disorderl Panic Disorderl Agoraphobial Generalized Anxiety Disorder
DSM VTrauma and Stress Related Disordersl Reactive Attachment Disorderl Disinhibited Social Engagement Disorderl Posttraumatic Stress Disorderl Acute Stress Disorderl Adjustment Disorders
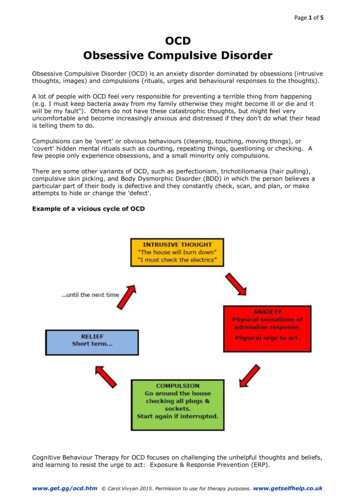
Obsessive Compulsive DisorderllllllObsessions: Thoughts, images or impulses that a personexperiences as unwanted, distressing, irrational and often timesof a bizarre nature. They are repetitive thoughts that are difficultto stop or control.The thoughts are not excessive worries about real-life problems.Compulsions: Behaviors that a person develops to neutralize theunwanted thoughts in an effort to obtain relief. Can be mental orphysical.The thoughts/behaviors cause marked distress.Take up more than one hour per day.Interfere with some aspect of daily routine.
Obsessive Compulsive DisorderContinuedlllWith good or fair insight: Recognizes that the beliefs aredefinitely or probably not true.With poor insight: The individual thinks their beliefs areprobably true.With absent insight/delusional beliefs: The individual iscompletely convinced the beliefs are true.
Body Dysmorphic DisorderllllPreoccupation with one or more perceived defects orflaws in physical appearance that are not observable orappear slight to others.At some point in the disorder, the person has peformedrepetitive behaviors.Preoccupation causes clinically significant distress orimpairment.The appearance preoccupation is not better explainedby concerns with body fat or weight whose symptomsmeet diagnostic criteria for an eating disorder.
Hoarding DisorderllllPersistent difficulty discarding or parting withpossessions, regardless of their actual value.The difficulty is due to a perceived need to save theitems and to distress associated with discarding them.The difficulty discarding the possessions results in theaccumulation of possessions that congest and clutteractive living areas significantly compromising theirintended purpose or use.Causes clinically significant distress or impairment.
TrichotillomaniallllRecurrent pulling out of one’s hair, resulting in hair loss.Repeated attempts to decrease or stop hair pulling.Causes significant distress or impairment.Hair pulling or hair loss is not due to another medicalcondition.
Excoriation DisorderlllllRecurrent skin picking resulting in skin lesions.Repeated attempts to decrease or stop skin picking.Causes clinically significant distress.Not attributable to the physiological effects of asubstance or other medical condition.Not attributable to another mental disorder (e.g.delusions, or tactile hallucinations).
What Can OCD Look Like?llllllllFear of harming self or othersFear of blood/HIV/AIDS/herpesFear of pregnancyFear of not doing things perfectlyFear of becoming a child molester/pedophileFear of urine/feces (contaminating self or others)Fear of homosexualityFear of being punished by a religious figure(Scrupulosity)
What can OCD Look Like?l Fearof illness (health related/somaticobsessions)l Fear of sexual thoughtsl Reading and rewritingl Perfectionisml Counting compulsions
What is the Goal in OCD?llllllCertaintyRelief of doubtConfirmationCompulsionsLoved ones/familyAnything to support the cause
What is Pure Obsessions?l Whenone only has obsessions but nocompulsionsl No such thingl An obsession is a compulsion
Brain Chemistry
llllllCycle of anxiety in generalAmygdalaSympathetic and parasympathetic nervous systemFight or flight responseThe experience of the amygdala misfiring and a senseof real dangerPerceived threat is always greater than the actual threat
Cognitive Behavior TherapyVs.Exposure and Response Prevention
Cognitive Behavioral TherapyllllLooks at how distortions in thinking, impacts/affects howone feels, and then translates into behavior.Distortions include: All or none thinking;Catastrophizing; Mind reading; “Should” statements;Fortune Telling; All or none thinking; Catastrophizing.Logic Based approach.Poking holes in negative thinking patterns to disprovestatements.
When to Use CBT When Workingwith Someone with OCDllWhen depression is impacting patients abilityto address the OCDWhen negative thinking patterns are a barrierto engaging in ERP
CBT Exerciselllll3 X 5 notecard.Front side: Write name of distortionBack side: One line definition and thenexamples of how that distortion applies tothem.Reminder: Most people have cognitivedistortions. It’s whether they get caught upand stuck in them.Looking at how it impacts their life.
Exposure and Response Preventionl Exposure to feared object, thought, scenario,without doing a compulsion to neutralize thefeared outcome.l Systematic desensitization.l Process of habituation.
Beginning the Exposure ProcessllllllDecide on a theme to start withCreate a fear hierarchyTake an inventory of situations that trigger the fearArrange them from low anxiety to high anxietyAssign SUDS value to each of themCollaboratively select first item with which to startexposure therapy
How Do You Create a Hierarchy?l Wordsl Picturesl Soundsl Videosl Actualobjects/situationsl In vivo versus Imaginal exposures
Starting Exposure TherapyllllllExpose fully and repeatedlyClients to have as much contact with the feared item orsituation as possibleAllow for at least a 50% reduction of anxietyAllow for enough time to support the desensitizationprocessEnsure there are no distractionsWork toward the top of the fear hierarchy
What Occurs During the ExposureProcessllllllAcknowlege the feared outcome.Focus on the doubt and uncertainty about what theindividual fears could happenAbstain from ritualsDevelop Remain in the situation until anxiety decreasesor dissipatesExposure and response prevention scheduleEngage in multiple exposures on a daily basis
Response PreventionlllRefers to one’s ability to focus on the feared outcomewithout engaging in any compulsions or rituals.Avoid engagement in safety behaviorsTrack anxiety
Imaginal ExposurelDevelop scenariosHave client verbalize mental images, thoughts, or impulses indetailRecord these scenariosDecide whether to use the voice of the patient or the voice of thetherapistExpose in a graduated fashionRecord on 1 or 3 minute endless loop tapeExpose to content and meaning of contentlExpose the person to the content of their obsessions and fearsllllll
Interoceptive Exposures/SymptomInduction ExerciseslllllllHead ShakingHead liftingStepping Up/Running in PlaceBreath HoldingSpinningHyperventilatingStraw Breathing
Habit Reversal Trainingl To address repetitive behaviors.l Channel anxiety/urges into competing response.l Awareness training.l Competing response training.l Relaxationtraining.
Assessment
Assessment Toolsl YaleBrown Obsessive CompulsiveSurveyl Yale Brown Obsessive CompulsiveScalel Beck Depression Inventoryl Beck Anxiety Inventoryl Reynolds Adolescent Depression Scalel Fear Survey
Goals in the Initial SessionlllllDiscuss diagnostic impressionsExplain brain chemistry and why they are strugglingReview CBT and ERP as a treatment modality and how it willhelp to address their needs specificallyDiscuss recommended protocol for treatment based on symptomseverity (Individual once per week; Intensive Outpatient;Medications; and so forth)Group therapy is to augment the process
Provide treatment overviewlllllllSome patients fear treatment will make them worse.Some fear that what they “fear” will happen if they facetheir fears.Help patients to anticipate what to feel or expect.Teach clients self-monitoring (5 section notebook,charting).Behavioral homework assignments.Treatment needs to be a commitment.Helpers
Further Assessment /ToolsllllllFamily Accommodation ScaleFreedom from OCD by Jonathon GraysonAbout OCD ArticleReassurance ArticleUnstuckInternational Obsessive CompulsiveFoundation Resources
Be Concrete and Assume NothinglllGet the details of the symptoms, and other relevantinformation to help understand the perceived threat.Some clients are reluctant to express a number ofunacceptable thoughts, images, or impulses for anumber of reasons.Do not assume they are being resistant. They may feelscared.
Embarrassment and ShameContinuedlllThere can be a lot of guilt associated with years ofimpact on the family.Fear that people will think they are “crazy.”Embarrassment over the potentially bizarre nature oftheir thoughts/fears.
Assess Impact of Symptoms onClients General Functioning Explore impact on work, school, relationships, homeenvironment, etc.Try to get them to resume chores, activity, etc. as soonas possible.Avoidance of these activities only gives more attentionto the anxiety.Limit the time that the anxiety is talked about inconversations outside of treatment.
Evaluate How Others are Involved in Maintainingthe Symptoms Family Accommodation Do family members carry out activities (chores, care ofchildren, home schooling, etc.) so that they can avoidtheir anxiety?Is the family giving reassurance?****Remember, simply talking about symptoms canserve as a source of reassurance!A “no talk” rule may need to be established at somepoint in the therapy process.
What Do Clients want or fear?l Miraclel Magic pill or medicationl “Just say something to make this go away.”l Did I do something wrong?punished?l Am I a bad person?Am I being
What Doesn’t Work? “I need to find my inner child.”“If I just know why I’m doing what I”m doing then I canstop.”“Hypnosis PLEASE!”Biofeedback“Hold and become the rock.”“Finding what happened in your childhood that iscausing this behavior.”“I was told Cognitive Behavior Therapy not Exposureand Response Prevention Therapy.”
What Doesn’t Work ContinuedllllllPsychotherapyLogicalizingUsing evidence to try to convince them that they don’tneed to be anxiousAsking them to do something that they cannotFloodingModeling exposures
Motivating FactorslllllBy taking a fight response to your anxiety, you reduceyour fear.Change the neurochemistry in your brainWhat’s predictable is what you have been doing. What’sunpredictable is to do something differentReclaim your life and do what you want to do ratherthan what your OCD (anxiety) wants you to do.You can live your Greater Good!!
Important ReminderslllllA client will typically know if you are in tunewith what they are experiencingValidate their concerns and distress.Remember, their fear is real to themBe open with your questions yet gentle toprovide an empathic approachSeek consultation if you are stuckIt’s okay to let a client know that you are notsure how to approach certain stages
The FamilylllllEducate, educate, educate.Eliminate all teasing.Eventually eliminate the compulsions which serve tohave them avoid.Do not try to talk them out of their fears (Helping themto see how silly and ridiculous they are being).Be a part of the therapy process.
More of “Back to the Family”lllllRecognize that doing less will actually do more!Help the family to understand that their loved one is notbeing “selfish.”Remind them this is a fear based disorder.Telling them to “just stop it” will not work, and serves tobe invalidating.Anxiety is not about trying to control others.
Motivational InterviewingllDesigned to help the client identify reasons why makinga change would be a benefit to them, their family, andother aspects of their life.Helps to acknowledge that while there is a cost tochange, the benefits of change will serve them and theiroverall happiness in the long run.
What Motivates People to Change?lllIdentification of the importance of the problem.Having the confidence in the ability to change.Internal desire- It cannot be imposed by others.
How to Address AmbivalencellllExpect it, even if they recognize that there is a problem.Encourage them to express their ambivalence andfears.Facilitate resolution of ambivalence with gentleencouragement.Remind them you are in partnership to get the problemresolved in the least distressing manner possible.
Factors Influencing MotivationlllllSocial supportHome visitsDepressionAnxietyAbility to tolerate discomfort
Talk About the GoalslllllDecreased anxiety and fearImprove general functioningIncreased social contact with othersImproved relationships with familyIncreased time to do other activities
Dealing with ResistancelllllllValidate their feelings and distressAcknowledge that their strugglesActively listenExpress your concern using non-judgmental languageMake it clear that you are there to help and offersupportAcknowledge that you are their to work collaborativelyto get them through their anxietyAnger and depression may be a component to address
Other Important Aspects of treatmentIncrease activityü Regular activity in the outside worldü No avoidance of normal expectancies in the houseü Increase pleasurable/social activitiesFood Considerationsü Be aware of excessive amounts of sugar and carbohydratesü Do not overeat, especially prior to bedtimeü Limit caffeine intake, especially in afternoon/evening
Case Examplel Sarahl 28year old Sherriffl Married with a dogl Fear of contaminationl Individual therapyl Intensive Outpatient Program
ResourcesüThe International Obsessive CompulsiveFoundation www.iocdf.orgüOCD Sacramento www.ocdsacramento.org
Final Outcome for Your Client
The Anxiety Treatment CenterSacramento, CAwww.anxietytreatmentexperts.comEmail: drrobin@atcsac.netPhone: 916.366.0647
Obsessive Compulsive Disorder lObsessions: Thoughts, images or impulses that a person experiences as unwanted, distressing, irrational and often times of a bizarr