Transcription
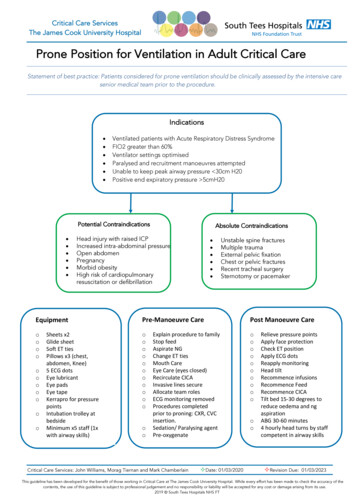
Prone Position for Ventilation in Adult Critical CareStatement of best practice: Patients considered for prone ventilation should be clinically assessed by the intensive caresenior medical team prior to the procedure.Indications Ventilated patients with Acute Respiratory Distress SyndromeFIO2 greater than 60%Ventilator settings optimisedParalysed and recruitment manoeuvres attemptedUnable to keep peak airway pressure 30cm H20Positive end expiratory pressure 5cmH20Potential ContraindicationsAbsolute Contraindications Headinjury with raised ICPPotentialContraindications Increased intra-abdominal pressure Open abdomen Pregnancy Morbid obesity High risk of cardiopulmonaryresuscitation or defibrillationEquipmentoooooooooooSheets x2Glide sheetSoft ET tiesPillows x3 (chest,abdomen, Knee)5 ECG dotsEye lubricantEye padsEye tapeKerrapro for pressurepointsIntubation trolley atbedsideMinimum x5 staff (1xwith airway skills) Unstable spine fracturesMultiple traumaExternal pelvic fixationChest or pelvic fracturesRecent tracheal surgerySternotomy or pacemakerPre-Manoeuvre CareoooooooooooooExplain procedure to familyStop feedAspirate NGChange ET tiesMouth CareEye Care (eyes closed)Recirculate CICAInvasive lines secureAllocate team rolesECG monitoring removedProcedures completedprior to proning: CXR, CVCinsertion.Sedation/ Paralysing agentPre-oxygenateCritical Care Services: John Williams, Morag Tiernan and Mark Chamberlain²Date: 01/03/2020Post Manoeuvre CareooooooooooooRelieve pressure pointsApply face protectionCheck ET positionApply ECG dotsReapply monitoringHead tiltRecommence infusionsRecommence FeedRecommence CICATilt bed 15-30 degrees toreduce oedema and ngaspirationABG 30-60 minutes4 hourly head turns by staffcompetent in airway skills²Revision Due:01/03/2023This guideline has been developed for the benefit of those working in Critical Care at The James Cook University Hospital. While every effort has been made to check the accuracy of thecontents, the use of this guideline is subject to professional judgement and no responsibility or liability will be accepted for any cost or damage arising from its use.2019 South Tees Hospitals NHS FT
'Cornish Pasty' .18.19.20.21.22.Identify turn leader / coordinator.Identify person to manage airway during the procedure.2x staff each side of the bed.Patient’s limbs to have lines protected with towel/pad.Pre-oxygenatePlace spo2 probe onto the limb.Remove all other monitoring.Remove pillow.Insert slide sheet using concertina technique.Place 1 sheet on top of the patient.Roll sheets together on each side of the patient.Slide patients to the side of the bed (ideally away from the ventilator).Turn patient onto side by pulling patient up towards you, then away from you in a 'C'shape.Rotate patient onto new sheet until in the prone position.Check head position- deflate top cells if needed.Check ETT, lines etc.Position into the 'swimmers' position.Put pillows under the flank.Place pillows/repose under shins (to keep toes off the bed).Reattach monitoring.Reattach cables and infusions.Tilt bed at 15-30 degree angle.Critical Care Services: John Williams, Morag Tiernan and Mark Chamberlain²Date: 01/03/2020²Revision Due:01/03/2023This guideline has been developed for the benefit of those working in Critical Care at The James Cook University Hospital. While every effort has been made to check the accuracy of thecontents, the use of this guideline is subject to professional judgement and no responsibility or liability will be accepted for any cost or damage arising from its use.2019 South Tees Hospitals NHS FT
Critical Care Services: John Williams, Morag Tiernan and Mark Chamberlain²Date: 01/03/2020²Revision Due:01/03/2023This guideline has been developed for the benefit of those working in Critical Care at The James Cook University Hospital. While every effort has been made to check the accuracy of thecontents, the use of this guideline is subject to professional judgement and no responsibility or liability will be accepted for any cost or damage arising from its use.2019 South Tees Hospitals NHS FT
'Routine' prone 18.19.20.21.Identify turn leader / coordinatorIdentify person to manage airway during the procedure2x staff each side of the bed.Patients arm to have lines protected with towel/padPre-oxygenatePlace spo2 probe onto the limbRemove other monitoringRemove pillowInsert slide sheet using the concertina technique.Slide patients to one side of the bed (ideally away from the ventilator).Place new sheet onto the bed.Turn patient onto side by pulling patient up towards you, then away from you in a 'C'shape.Rotate patient on to the front, onto new sheet until in the prone position.Check head position- deflate top cells if neededCheck ETT, lines etc.Position into the 'swimmers' position.Put pillows under the flank.Place pillows under shins (to keep toes off the bed).Reattach monitoring.Reattach cables and infusions.Tilt bed at 15-30 degree angle.Critical Care Services: John Williams, Morag Tiernan and Mark Chamberlain²Date: 01/03/2020²Revision Due:01/03/2023This guideline has been developed for the benefit of those working in Critical Care at The James Cook University Hospital. While every effort has been made to check the accuracy of thecontents, the use of this guideline is subject to professional judgement and no responsibility or liability will be accepted for any cost or damage arising from its use.2019 South Tees Hospitals NHS FT
The delivery of CPR in prone position ICU patients in cardiac arrest.Cardio pulmonary arrest is a very time sensitive situation. Once cardiac arrest isconfirmed all guidance for the adult resuscitation states commencing effective CPRimmediately to maintain brain perfusion increasing the chance neurological recoveryshould a Return of Spontaneous Circulation (ROSC) occur. However for the ICU patientthat is in the prone position a significant amount of time maybe lost turning the patientsupine especially when tubes and invasive devises are present. This also required asignificant number of people to achieve.There is a growing body of evidence suggesting the commencement of CPR whilst thepatient is in the prone position is an effective immediate response especially in theintubated patient. Some studies suggest CPR in the prone position can be moreeffective in generating effective perfusion than in the supine position. There appears tobe no specific evidence to suggest that a different level of hand position, depth or rateof CPR will be of greater benefit than what is currently recommended in the supineposition. To aid in the retention of skills it also make since to try to achieve the currentrate and depth of compression only in the opposing position between the thoracic andcervical spine.1.2.3.4.5.6.7.Call for helpConfirm cardiac arrestIf air mattress deflate / use CPR feature on bed frame tolower to a reasonable height to perform CPR.Deliver CPR in the centre of the upper spine at a rate of100-120 / min aiming for 5-6 cm of compression (standardrecommendation).If arterial blood pressure monitoring present and ETCO2observe monitor for perfusion wave form generation.If no effective perfusion suspected or airway managementineffective when sufficient help and skills present, considerrapidly tuning the patient supine and recommencingstandard approach to CPR.Defibrillator pad placement in corresponding positionsover the right scapula and left mid axilla. Also, anterior /posterior or right and left mid axilla can be used in theprone positionCritical Care Services: John Williams, Morag Tiernan and Mark Chamberlain²Date: 01/03/2020²Revision Due:01/03/2023This guideline has been developed for the benefit of those working in Critical Care at The James Cook University Hospital. While every effort has been made to check the accuracy of thecontents, the use of this guideline is subject to professional judgement and no responsibility or liability will be accepted for any cost or damage arising from its use.2019 South Tees Hospitals NHS FT
PROCEDURE CHECKLISTNameAimTo ensure patient safety is maintainedand best procedural practice is attainedwith the intention of minimising theoccurrence of adverse effects.WhenThroughout the procedure.WRITE OR ATTACH ADDRESSOGRAPHSurnameForenamesDOB dd / mm / yyyyAgeHospital numberBy whom All healthcare professionals responsiblefor the procedure.BNHS numberSIGN INywh All members of the team introduced themselves Feed stopped and O/NGT aspiratedom Consultant/Senior nurse aware. If NO, explain Non-essential monitoring & infusions discontinued:reason Adequate length on remaining lines going either up orAlAny contraindications NO YES. If YES,down bed checkedlexplain Chest drains below patient and clamped (only if safe to hedo so)a Skin integrity assessed and documentedlt Eyes taped and lubricated Anti-pressure dressings to bony prominences andh ETT taped/tied (ETT anchor devices removed)cnipplesa Re-intubation equipment available Daily hygiene completed (i.e., mouthcare, washing,re Other equipment available as per guidelinedressings, etc.)prAre there any concerns about this procedure for the patient? NO YES - If YES, orestartofprocedureTIME OUTsi Minimum of 5 people plus 1 for chest drains Team members familiar with procedureon All team members aware of role Adequate sedation (i.e., RASS -5)al Appropriate ventilator settings Adequate muscle relaxation – consider need for bolussr Cardiovascular stability Pillows positioned correctly – chest, pelvis, kneesesTo be confirmed post procedure before leaving the bed areaSIGN OUTpPressure areas checked: Capnography & monitoring re-establishedon ETT not pressing against lips Ventilator settings reviewedsi No pressure on eyes Lines securedb Ears not bent over Chest drains below patient and unclampedle NG not pressed against nose Slide sheet removedf Penis between legs & urinary catheter secured Reverse Trendelenburg 30 or Lines & tubing not resting against skin NG position confirmedt Pillows positioned correctly Enteral feed resumedhePRINT NAME / SIGN / REG NOinChecklist completed by Date TimeseOther team membersrtLocationionProning Checklist / General Critical Care / 06/02/20201 ,onPreparation prior to proning patientCritical Care Services: John Williams, Morag Tiernan and Mark Chamberlain²Date: 01/03/2020²Revision Due:01/03/2023This guideline has been developed for the benefit of those working in Critical Care at The James Cook University Hospital. While every effort has been made to check the accuracy of thecontents, the use of this guideline is subject to professional judgement and no responsibility or liability will be accepted for any cost or damage arising from its use.2019 South Tees Hospitals NHS FT
PATIENT NAME DOB HOSPITAL NoAREACHECK POINTChecked / InitialsCheck ETT/Tracheostomy is accessible/not kinked (ETT cm at teeth )All connections between ETT and ventilator circuit secureNote ETT/tracheostomy cuff pressureETT positioned in middle of mouth, not compressing lipsDermal gel pads placed between ETT cotton ties and patient’s skinHead/FaceConfirm ears are not bent overPerform ETT/tracheal suctioning immediately post proningEyes taped shutNo direct pressure on the eyesEnsure 30 foot down positioning (Reverse Trendelenburg)Move patient’s head from side to side 2 hourly to relieve pressureNG tube secure and not displaced (cm at nose )NG tube not causing pressure to nostrilNeckVerify that patient’s lower back and neck are not hyper-extendedFront of neck free from compressionCentral line secureChestChest drains patent and on correct suctionBreasts supported and free from pressureAbdomenAbdomen freePelvis support cushion in placeMale genitalia positioned between legsCatheter tubing is free and between legsShoulders not rotatedPelvisNo compression over elbowsWrists in neutral positionHands freeAlternate Swimmers Position 2-4 hourlyNo peripheral IV lines under patientLegsPillows positioned under shins to prevent extensionAll monitoring recommencedAll infusions connected and infusingCheck CRRT lines patentInfusions andMonitoringECG leads not underneath patientEnsure patient is well sedated and pain freeInfusion lines not resting on patient’s skinMattress is in dynamic modeCheck ABG 20-30 mins post prone positioningck Point2Proning Checklist / General Critical Care / 06/02/2020Critical Care Services: John Williams, Morag Tiernan and Mark Chamberlain²Date: 01/03/2020²Revision Due:01/03/2023This guideline has been developed for the benefit of those working in Critical Care at The James Cook University Hospital. While every effort has been made to check the accuracy of thecontents, the use of this guideline is subject to professional judgement and no responsibility or liability will be accepted for any cost or damage arising from its use.2019 South Tees Hospitals NHS FT
Document DetailsTitleProne Position for Ventilation in Adult Critical CareMain points the document coversWho is the document aimed at?All general critical care staffAuthorJohn Williams, Morag Tiernan and Mark ChamberlainApproval processApproved byCritical Care Guidelines and Clinical Governance GCCEffective fromMarch 2020CategoryCritical Care Services JCUHSub-CategoryRespiratoryReview dateMarch 2023Document LinksRequired by CQCICS/FICMRequired by NHSLAOtherExternal references used1.Guidance For: Prone Positioning in Adult Critical Care. Intensive Care Society and Faculty of Intensive careMedicine. November 2019Amendments HistoryNoDateAmendment12345Critical Care Services: John Williams, Morag Tiernan and Mark Chamberlain²Date: 01/03/2020²Revision Due:01/03/2023This guideline has been developed for the benefit of those working in Critical Care at The James Cook University Hospital. While every effort has been made to check the accuracy of thecontents, the use of this guideline is subject to professional judgement and no responsibility or liability will be accepted for any cost or damage arising from its use.2019 South Tees Hospitals NHS FT
Critical Care Services: John Williams, Morag Tiernan and Mark Chamberlain ²Date: 01/03/2020 ²Revision Due: 01/03/2023 This guideline has been developed for the benefit of those working in Critical Care at The James Cook University Hospital. Whil