Transcription
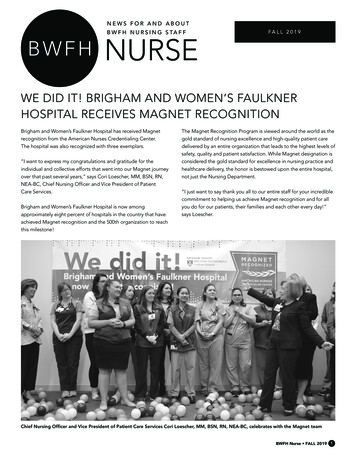
SUMMER 2011N E W S F O R A N D A B O U T FA U L K N E RH O S P I TA L N U R S I N G S TA F FFAULKNERINP3:NURSETHIS ISSUENURSING PAIN MANAGEMENTCOMMITTEE: PAIN AS THE FIFTHVITAL SIGN Jane Shufro, RN, BSN, CPAN6 South and patient satisfactionP4-5: Nursing AwardsP6:Are you a culturallycompetent nurse?P8:Endoscopy proficiency workshopP11: Recommendations for verbaleducationMembers of Faulkner Hospital’s Nursing Pain Management Committee from left, Mary PatCunniffe, Kitty Rafferty, Barbara Peary, Helene Bowen Brady, Jane Shufro, Jeanne Hutchinsand Lauren Morrisssey.Faulkner Hospital’s Nursing Painof the nursing staff in the area of painManagement Committee is dedicatedassessments, reassessments and protocols,to meeting the pain management andcreating an environment that is conduciveeducation needs of our patients and theirto excellence in nursing practice andfamilies. In the past, Faulkner has hadpatient care.an interdisciplinary pain managementteam that addressed the issues of painThe Committee is comprised of registeredassessment, sedation risks, and identifiersnurses representing each of the inpatientfor safe medication administration withinand specialty areas, staff development,the hospital.nurse practitioners and nurse directors,as well as an Associate Chief Nurse. TheOver two years ago the need for a specificCommittee Co-chairs oversee the planningNursing Pain Management Committeeof monthly meetings and any workshops,was identified to look at nursing practicesone of which was a “retreat day” whererelated to pain management. Since then,the committee met for an entire workdaythe committee has continued to further theto refine the QI pain audit tools toeducation and professional developmentmore accurately reflect the type of paincontinued on P2Faulkner Nurse SUMMER 2011 1
DEAR NURSING COLLEAGUESFirst let me say thank you and95th percentile or achieving best practicecongratulations for another successfulnationally for care of CHF patient.celebration of our Nursing Professionas we closed out the month of May withThis high quality care is the expectationNurses’ Week, a week that continues toof our patients and staff and we need tohighlight the best of our practices here atprovide this care in the most affordableFaulkner Hospital.fashion to meet the demands on us as ahealthcare institution. I know as we workThis year we had a Nursing Awardstogether on this we will reach solutionsCeremony attended by not only staff andthat not only maintain the excellence intheir families but the families that continueto support our Nursing Awards. It was soenriching to be able to hear of the greatpractice of all the award winners picturedin this edition of Faulkner Nurse. Afterreading this edition of Faulkner Nurse youwill see exactly what makes our nurses thebest! They are often seen as mentors,patient educators, life long learners andnurses that our patients and families havecome to count on for their care.Judy Hayes, RN, MSN, CNOThe poster session during Nurses’ Weekallowed us to highlight the many diverseareas of practice that we have here atFaulkner Hospital. Our next few monthspatient care but also assure that the careis accessible for all patients. Enjoy yoursummer.Sincerely,will be challenging ones as we all examineour ability to provide care that continuesto meet all the quality and satisfactionmetrics that we have attained - whether itis our Press Ganey inpatient satisfactionJudy Hayes RN, MSN, CNOVice President of Nursingscores reaching an all time high of theNursing Pain Management Committee: pain as the fifth vital sign, continued from P1assessments for their own practice areas.they are providing,” according to HeleneEducation to meet the learning needs ofPrior to this, all units used the same toolBowen-Brady from staff development.nursing staff was another focus this pastto assess pain which did not accuratelyWorking with IS to refine Meditech soyear and a guide to pain reassessmentportray the best practice. They also collectthat RN’s can document “real time”documentation, “The Road to Excellenceand collate the monthly pain QI dataassessments and using the Vocera/in Pain Management” was posted onthat demonstrates how staff documentSignet integration to monitor responseNursing Practice Boards for unit discussion.pain assessments and re-assessments.to patient’s requests for medicationThe committee members will be looking atAlthough many of the staff nurses haveare a few of the accomplishments thatthe development of educational programsbeen introduced to their unit pain tool,the committee has brought to currentfor patients, family and staff about painthey may not necessarily have informationnursing practice. By reviewing themanagement, as well as collaborate toabout where that data is used – or that it’squality indicators monthly, the committeerevise policies and procedures related todesigned to enhance strategies that couldmembers are able to identify strongpain management.improve how nurses document.nursing practices that can then beshared with other units in an effort toIn the near future, we will be conducting“We feel that nurses do know where theirimprove nursing practices related to paina staff Knowledge and Attitude surveypatient’s pain level is but the challengemanagement.which will be used to apply evidence-is ensuring that nurses are consistentlybased interventions for more effective paindocumenting the excellent nursing caremanagement in our nursing practice.2 Faulkner Nurse SUMMER 2011
6 SOUTH’S EFFORT TO IMPROVE PATIENT SATISFACTIONLast September, the staff of 6 SouthThey educate the patient on theirwas asked to participate in a Leanroom and how to use the callquality improvement initiative.light. The nurse and the nursingThe Lean program is a philosophyassistant update the patient whitethat helps drive efficiency throughboard every shift in the room withemployee empowerment andtheir name and titles.changes at the grass roots level.In-patient satisfaction surveysLean principles include gainingwere completed both before andrespect from individuals for theirafter this intervention. Below areideas which fosters the most impacttwo graphs of the Press Ganeyon results.results showing the improvementSarah Sawyer, left and Kathy Codair.in the two questions. The firstAfter reviewing the Press Ganeyreport from last summer it was clear thata change needed to be initiated. July of2010’s press Ganey report showed thatpatients were scoring nursing staff at alower percentage than previously. KathyCodair, Nursing Director, solicited SarahSawyer, staff nurse, to research the issuesand problems.Together Kathy and Sarah, coached byCori Loescher, attended a Partner’s wideLean training program which met monthlyfor five months. Sarah and Kathy met withthe staff to define sources of waste andgraph shows the delay in meetingData was collected in these two areas overa period of time. The researchers foundthe patient’s needs and the second graphshows the staff’s attitude toward requests.that call lights were being answered in atimely manner, however the patient’s needwas not always being met, such as whena patient requested pain medication butthere may not have been a doctor’s orderfor the pain medication.Kathy and Sarah warn that change takestime and having staff input was the keyto the success that they have seen. Thehardest thing now will be sustaining thesuccess.Sarah and Kathy initiated education to thenursing assistants regarding the importance of quality communication with patients. A script was designed by the nursing assistants to outline key information.delays in meeting people’s needs. Theyanalyzed the results of two Press Ganeyquestions: delay in meeting the patientneeds and staff’s attitude toward requests.The nursing assistant introduces themselves by name to their patient and familyand explains the purpose of their visit.Published by Marketingand Public Affairs(617) 983-7588djgoldberg@partners.orgWe welcome your feedback andsuggestions for future issues.Faulkner Nurse SUMMER 2011 3
NOTES ON NURSES’ WEEK AWARDSCONGRATULATIONS TO ALL OF THE 2011 AWARD WINNERS!THE ELAINE HAZELTONMEMORIAL SCHOLARSHIPwas presented to Margaret McNulty, RN, Dana-Farber/Brighamwas established by Elaine’s family and is given to a nurse whoand Women’s Cancer Center at Faulkner Hospital. The McAlarneydemonstrates a dedication to Faulkner Hospital and the practiceAward was established in 2003 to be given to a member of theand advance of nursing along with continuing their education.Nursing Department in recognition of excellence in patientThis year’s winner was Kimberly Tierney, RN, 6N.teaching.Kimberly Tierney, RNFrom left, Judy Hayes and Margaret McNulty.THE MAL AND LOIS LEWIS EXCELLENCE INNURSING PRACTICE SCHOLARSHIP AWARDwas established in 2010 to be given to a nurse that meetsthe following criteria 1. a nurse working in cardiology thatdemonstrates compassion in a family centered context, 2. a nursethat advocates for the patients using evidence-based researchand 3. a nurse who is recognized by her/his peers for their uniquecontribution. The 2011 winner was Tammy McNeil, RN, 6N.From left, Judy Hayes, Tammy McNeil andAnnie Lewis-O’Connor, PhD.4 Faulkner Nurse SUMMER 2011THE ANGELA MCALARNEY AWARD
This past May, seven members of Faulkner Hospital’s Nursing staffwere presented with awards. The nurses were nominated by their peers.Each award has different criteria but all of the awards link to the profession of nursing.THE MRACHECK AWARD was established in 1995 to be given to three members of the Nursing Department for recognitionof their clinical skills, as well as to support their continuation in the nursing profession. This year’s winners were Bridgid Stevens, RN,6S, Jackie Dejean, RN, 7N and Karen Clougher, RN, 6N.Bridgid StevensThe last award presented was theFrom left, Judy Hayes and Jackie Dejean.From left, Judy Hayes and Karen Clougher.MARY DEVANE AWARD.This award was established in 1999 to be given to any member ofthe Nursing Department in recognition of their commitment todelivering patient care with compassion, kindness and humor.The award was presented to Diane Corgain Hunt RN, OPOU.From left, Judy Hayes and Diane Corgain Hunt.Faulkner Nurse SUMMER 2011 5
AN EYE TOWARDS THE FUTUREBy Brenda Cleary, RNAs we enter the second decade of the newa great job, or the last time you sincerely thanked amillennium, we should take a moment or two tocolleague. I encourage senior nurses to rememberponder some of the changes that have occurred.that they were once new to their chosen field andTechnology continues at a remarkable paceworked hard to gain experience and build their skillbringing with it tremendous advances to people’sset. Faced with individual goals and providing expertlives. Unfortunately this may also come with acare in this fast paced world may make it hard toprice.consider mentoring, but remember we were all oncenew nurses and just as frightened and overwhelmedSociety, more and more has expectations ofas some of our colleagues may be right now.instant gratification. Whether it’s high speedinternet or fast food, we always want better andBrenda Cleary, RNquicker. We are hooked to our cell phones,So as we reflect on the celebration of the recentlypassed Nurses Week, let’s try to remember thatiphones, ipads and computers from the moment we wake untilskilled and expert nursing practice comes with old-fashioned timethe moment we go to bed. It should come as no surprise that thisand mentoring. We should challenge ourselves and pause longway of life has crossed over into our practice as nurses.enough to recognize and support our colleagues. Finally, let’skeep a special eye open for our newer nurses and welcome themAlong with providing expert care to our patients, we also need toto our team.remember to take care of our co-workers and ourselves. Stop andthink of the last time you told someone on your unit that they didARE YOU A CULTURALLY COMPETENT NURSE?By Yuka Hazam, RN, MSN, 6 SouthThe United States is more diverse than evertry’s language. The hospital smells different and is abefore and this will continue to be true. Americanvery unfriendly environment. The doctors prescribenurses require advanced skills to provide culturallysome strange medicines and acupuncture therapycompetent care for the patients. Culturally com-and these medicines are traditional and familiar inpetent care means that nurses and other health-this Asian country but not to you. They say this iscare professionals are able to work in cross culturalwhat you must do. Would you be comfortable ac-situations effectively.cepting these strange therapies? What would youwant to know if you wanted to be treated by them?The first step is to be aware of differences between you and patients. These differences maybe about their thoughts and values about healthNurses have important roles to play in culturallyYuka Hazam, RNcare and their lives. The second step is to providesensitive care. However, our skills and healthcaresystems are not yet advanced enough to provideculturally sensitive care which requires interpersonal and com-culturally competent care for patients who are not familiar withmunication skills. A lack of cultural sensitivity may cause conflictUS healthcare and practices. Some cultures are very complex. Inand unsafe care. A nurse or physician may believe that patientsaddition, family dynamics or religion may create conflict betweenmust follow our advice no matter what their culture is becausehealthcare providers and patients. Nurses must understand theour health care is the best in the world. However, our world classpatients’ comfort level and provide them with adequate infor-medicine could be useless and meaningless if patients do notmation. Nurses must improve interpersonal skills and skills thatunderstand or refuse it because our healthcare providers areestablish a trusting relationship between nurses, patients and theirculturally incompetent.families. This may not solve all cultural problems but it is the mostimportant part of cultural competency. Please share with me anyThink about this situation. You go to an Asian country and havechest pains. You have limited language proficiency in that coun-6 Faulkner Nurse SUMMER 2011of your cultural care experiences.
RISK MANAGEMENT CONSIDERATIONS WHEN CARINGFOR THE SUICIDAL PATIENT ON 1:1 OBSERVATIONJoanne Locke, RN, JDThe responsibility of the registered nurselearned about suicide risk assessment asduties and in essence, leaves the patient infor the care of any patient arises from apart of nursing education, hospital policiesthe unsupervised care of a sitter or securitylegal concept known as the “standard ofand procedures, and nursing practiceguard, the nurse has departed fromcare.” The standard of care is definedguidelines, which may be taught as partthe standard of care, and is responsibleas the degree of skill and learning ofof Nursing Case Review, seminars, andfor any injury that may result from suchthe average, qualified member of theworkshops. The average qualified nursenegligence.profession practicing the specialty,would be expected to know the basicHow can a nurse assure that she hastaking into account advances in therequirements of suicidal risk assessment,met the standard of care for monitoringprofession. While this definition maysuch as asking the patient if he is havinga suicidal patient? The nurse mustsound like legalese, the standard of carethoughts of harming himself, and ifbe familiar with hospital policies andis an important concept for nurses toso, whether he has a plan. Once theprocedures for the care of a patient atunderstand when assessing his or her riskassessment confirms that there appearsrisk for suicide, and comply with theof liability for adverse events.to be a risk of suicide, the nurse has apolicy requirements. This policy cannon-delegable duty to use reasonablebe found in Faulkner 411 and the nurseThe standard of care is determined byjudgment to meet the patient’s need forshould review it when a suicidal patientapplying nursing actions (or omissions)safety from self-harm.is under his or her care. Complianceagainst what is required by statute andwith the policy can be demonstratedregulation, policies and procedures,A non-delegable duty is one that only thethrough good documentation of nursingand other evidence of accepted nursingprofessional nurse can perform under theassessment, care, and communication ofpractice. When a nurse departs from theauthority of her professional license; asignificant changes. Documentation onstandard of care in the treatment of his ornon-delegable duty cannot be assigneda communication tool sheet that containsher patient, and the patient is injured asto an unlicensed practitioner. In the casereminders and an observer care plana result of this departure, the nurse canof a patient on 1:1 observation, this meansassures that both the nurse and the sitterbe found negligent, and may be subjectthat although a sitter or security officerunderstand what is required to assureto damages to compensate the patientmay be the person who is assigned to staythat the patient has received adequatefor injuries resulting from the negligence.with the patient and perform the actualmonitoring and care during the shift.Negligence may occur when a nurseobservation, it remains the sole duty ofWhile no nurse is expected to guaranteefails to use adequate clinical judgmentthe nurse to perform ongoing patientthe safety of a suicidal patient, the nursein patient assessment, or when the nurseassessments, to monitor for a changemust provide reasonable care. Followingfails to implement appropriate nursingin condition, to assure that the sitterthese steps can provide the patient withintervention. How does this apply to thehas received clear and comprehensivegood nursing care and demonstrate thatcare of a suicidal patient?instruction about what is expected of himthe nurse has met the standard of care.or her, and to perform adequate handWhen caring for a patient at risk ofoff communications with the doctor, thesuicide, the nurse is responsible for whatsitter, and the next nurse who cares for thethe average qualified nurse would havepatient. If the nurse fails to perform theseFaulkner Nurse SUMMER 2011 7
ENDOSCOPY PROFICIENCY WORKSHOPSeven thousand patients annually undergo endoscopic procedures at Faulkner Hospital’s Gregory Endoscopy Centre. Each ofthese patients depends upon the nursing staff to be thoroughlyskilled in all aspects of endoscopic care. The Joint Commissionrequires that staff be competent to perform their tasks and thatcompetence be assessed and documented at one to three yearintervals.In the technologically advanced endoscopy setting, new modalities and applications are frequently introduced and endoscopystaff must remain current in this changing environment. As endoscopy has moved beyond diagnostic procedures to the therapeuticand interventional, excellence in patient care and technologicalproficiency are closely linked.nursing staff, as experts in a particular modality provide educationTo meet this challenge, the nurses of Gregory Endoscopy Cen-and support to those less experienced. Stations included endo-tre dedicated an entire February afternoon to participating in ascopic band ligation, clipping, electrocautery, balloon dilators,hands-on proficiency workshop. The physician staff demonstratedargon plasma coagulation, sclerotherapy, and ERCP. The nursestheir commitment to this endeavor by freeing the endoscopyare also required to be thoroughly familiar with endoscope repro-schedule for the allotted time period. The workshop familiarizedcessing. Competence in this area is assessed and documentedstaff with lesser-used endoscopic therapies and reviewed day-to-annually.day processes to insure quality and safety based on best practiceguidelines. The nursing staff identified a need for more hands-onProcedural sedation and medication safety in the geriatr
Faulkner Nurse † SUMMER 2011 1 NURSING PAIN MANAGEMENT COMMITTEE: PAIN AS THE FIFTH VITAL SIGN Jane Shufro, RN, BSN, CPAN Faulkner Hospital’s Nursing Pain Management Committee is dedicated to meeting the pain management and education needs of our patients and their families. In the pa