Transcription
Expanding Multidisciplinary Carein Community Cancer CentersAn MDC assessment tool developed by the NCCCPby Patricia L. Swanson, RN, BSN; Patricia Strusowski, RN, MS; Thomas Asfeldt, RN, BAN, MBA;Judy De Groot, RN, MSN, AOCN ; Patricia D. Hegedus, RN, OCN , MBA; Mark Krasna, MD;and Deb White, RN, BSN, CCM, OCN In BriefBy 2009 “expansion of integrated multi-specialtycancer care through new or expanded approaches toimprove coordination” was a program deliverable forall NCCCP sites. Accordingly, an NCCCP Qualityof Care Subcommittee was established and taskedwith identifying a means to evaluate and implement multidisciplinary cancer care (MDC) at eachNCCCP site.The end result was the creation of a MDCdevelopment assessment tool composed of seven keyindicators—with five levels, ranging from “evolvingMDC” to “achieving excellence”—to measure thelevel of MDC implementation at each site. NCCCPsites incorporated each of the key assessment areasinto their programs; however, the levels for each areavaried from site to site, depending on geographicfactors and availability of resources. For example, anNCCCP site in an urban area may easily have a faceto-face MDC model, whereas a rural site may need toimplement a virtual MDC model due to the distancebetween specialists and patients.Three years into the MDC project, all NCCCPsites showed measured improvement in the level ofmultidisciplinary cancer care delivered at their community cancer centers. Sites agreed that the mostimportant factor in the establishment of a MDCmodel is effective physician leadership throughout theprocess. A number of challenges to the implementation of MDC were identified, including limited support staff and insufficient amounts of time.Community cancer centers may find this MDCassessment tool and the experience of the NCCCPsites helpful in their efforts to create and/or expandmultidisciplinary care at their own centers.Assessment Tool DevelopmentA small working group was formed within the Quality ofCare Subcommittee to establish a framework for a MDCmodel that allowed NCCCP sites to assess their currentprograms and/or further develop their capabilities to delivercomprehensive and integrated services. The working groupagreed that a common definition of multidisciplinary cancer care includes: Prospective and/or concurrent review of patient care Multidisciplinary physician specialists Development and review of treatment plans based onevidence-based guidelines Efficient communication among physiciansOncology Issues January/February 2011Written treatment plans that are updated as necessaryand reviewed with the MDC team.Based on the collective experience of the working groupmembers (patient caregivers and hospital administrators),seven key assessment areas of MDC were identified. In noparticular hierarchy, these areas were:1. Case planning2. Physician engagement3. Coordination of care4. Infrastructure5. Financial6. Clinical trials7. Medical records.These assessment areas were put into a matrix, each withfive levels of increasing accomplishment (e.g., from Level 1 –“evolving MDC” to Level 5 – “achieving excellence”). Afterthe NCCCP Executive Subcommittee (comprised of thePrincipal Investigators at each site) approved the completedtool, it was provided to the NCCCP sites to evaluate theirexisting capacity to deliver multidisciplinary cancer care.Now, community cancer centers across the countrycan use the MDC assessment tool to evaluate their programs and guide growth opportunities in the delivery ofMDC. This tool can be found on pages 34 and 35.During their efforts to improve and expand the delivery of multidisciplinary care at their own cancer centers,NCCCP sites utilized the assessment tool, applied severalMDC models to develop their MDC infrastructure, andshared lessons learned.MDC ModelsNCCCP sites used the tool to assess how best to deliverMDC to meet patient needs, while taking into consideration facility space, logistical realities, and the cancer centerenvironment. The results showed multidisciplinary cancercare at each site was at different points along the assessmentscale; the spectrum ranged from minimal collaboration toface-to-face multidisciplinary clinics. Some NCCCP siteswere able to use the tool to assess their programs, yet wereunable to advance to a higher level due to local contributing factors. Here are three of the MDC models used by theNCCCP sites:Tumor Board. Several sites changed the format oftheir weekly retrospective disease-specific tumor boardsfrom educational case presentations to evidence-based andguideline-driven prospective case reviews. In this restructured format, the MDC model presents a patient’s case to theMDC team prior to the start of treatment. A treatment plancontinued on page 3633
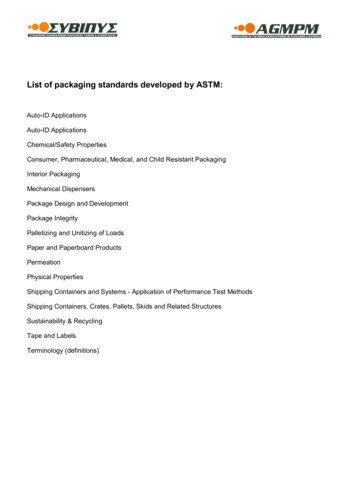
MDC Assessment ToolAssessment AreaEvolving MDCDeveloping MDCMDC(Level 1)(Level 2)(Level 3)34Case PlanningCare planning isasynchronous withpatient presenting tomultiple physician officeswithout a shared medicalrecord.Care planning isasynchronous withpatient presenting tomultiple physician officeswith a shared medicalrecord.Most care planningis asynchronous, butsome patient careplans are discussedin multidisciplinaryconferences, which occuron a weekly basis.PhysicianEngagementDiagnostic and treatmentphysician belong tomultiple independentgroups, with littleinteraction, and arepresentative from somegroups is engaged withthe cancer center.Diagnostic and treatmentphysician belong to multiple independent groups,with little interaction, andat least one representative from each group isactively engaged with thecancer center.The MDC has aphysician agreementof participation, andphysicians are activelyengaged in developingtreatment standards.Coordination of CarePatient care is episodic.Patient has to presentto multiple locationson multiple days fortreatment and ordiagnostic modalities.Information is stored inmultiple locations, anddifficult to coalesce.Patient care is episodic,but some treatment anddiagnostic modalities arecoordinated. Informationis coordinated and isreadily available tophysicians and staff.MDC has some dedicateddiagnostic and treatmentabilities to meet patient’scare needs. Informationis readily available tophysician and staff.InfrastructureLimited physicalinfrastructure withlimited informationsystem support. Hospital,physician office model.Limited physicalinfrastructure withintegrated clinicaland administrativeinformation systemsused by all.Some dedicated physicalfacilities, which donot cover the fullspectrum of care, withindependent clinicaland administrativeinformation systems.FinancialBilling is episodic, basedon encounter with facilityor physician. No facilityfee is applied.N/APhysicians bill separately.Introduction of facilityfee for MDC. Communication between MDC andphysician offices.ClinicalTrialsPatient not reviewed foreligibility for clinicaltrials. No literature givento patient on clinicaltrials.Some patients reviewedfor eligibility. No formalprocess to review patientsfor clinical trials. Clinicaltrial literature given topatient.2% of patientsparticipating in clinicaltrials. There is a formalaccrual and recruitmentplan. Clinical trialliterature given to allpatients.Medical RecordsPaper chart plus someEMR with isolatedpockets.Mainly for documentation reasons only. Medicalinformation is not integrated. Little to no sharing. Mixture of paper andelectronic.Mixture of paper andEMR. Starting to sharelabs, radiology, medicalhistory, treatment plans,and medications.Oncology Issues January/February 2011
Case PlanningPhysician EngagementMoving towardsExcellence(Level 4)All patient care planningis done through amultidisciplinaryconference, which occurson at least a weekly basis.Achieving Excellence(Level 5)Coordination of CareInfrastructureFinancialAll patient care planningis done through amultidisciplinaryconference, whichoccurs while the patientencounters care.Same as prior, with theaddition of engagementin quality improvementinitiatives and strategicdirection.Same as prior, with theaddition of physicianshave operational andfinancial authority forthe MDC.MDC is fully integratedwith treatment anddiagnostic modalities,and all information isavailable from a singlesource.Same as prior, with theaddition of ancillaryservices such aseducation, supportgroups, and wellnessprograms for patients andfamilies.Some dedicated physicalfacilities, which donot cover the fullspectrum of care, withintegrated clinicaland administrativeinformation systems.Dedicated center withability to provide fullservice to patients withintegrated informationsystems.N/AGlobal bill for MDCbilling, inclusive offacility fee.4% of patientsparticipating in clinicaltrials. There is a formalaccrual and recruitmentplan. Clinical trialliterature given to allpatients.6% of patientsparticipating in clinicaltrials. There is a formalaccrual and recruitmentplan. Clinical trialliterature given to allpatients.75% of hospital systemand physician offices isintegrated electronicallyacross the continuum.Fully integratedelectronic record acrossthe continuum withaccess to information.Oncology Issues January/February 2011ClinicalTrialsMedical RecordsTotal ScoreLevel 1—Evolving MDC ProgramThis level describes organizations that meet regulatoryrequirements and Association of Community CancerCenters (ACCC) guidelines. There are a few performanceimprovement initiatives underway, and some centers ofexcellence. The leadership vision for quality is unclear.The organization lacks sufficient personnel and financialresources to administer a fundamental program thatsupports conducting MDC initiatives designed to attainimprovements in patient care, quality, safety, andefficiency.Level 2—Moving Towards MDC ProgramOrganizations at this level have some of the fundamentalstructures and processes for achieving MDC initiatives.The leadership vision for quality is under development.Some personnel and financial resources are available tosupport the organization attain some improvements inpatient care, quality, safety, and efficiency, but they areinsufficient for a comprehensive program.Level 3—MDC ProgramOrganizations at this level have many of the fundamentalstructures and processes for running MDC initiatives.Leadership’s vision for quality is known to many in theorganization. Personnel and financial resources are available to support the organization in attaining a numberof changes in the improvement of patient care quality,safety, and efficiency, and changes largely are driven bythe cancer center staff.Level 4—Moving Towards MDC ExcellenceOrganizations at this level have many significant structures and processes for deploying MDC initiatives. Personnel and financial resources are available to support theorganization in attaining many important changes andimprovements in patient care, quality, safety, and efficiency. Some staff outside the cancer center play lead rolesin fostering initiatives.Level 5—Achieving MDC ExcellenceOrganizations at this level have many best of classstructures and processes deploying MDC initiatives.Personnel and financial resources are spread throughoutthe organization and available to support the attainment of many important, leading, and creative changesand improvements in patient care quality, safety, andefficiency. Many staff outside the cancer center play leadroles in fostering initiatives and achieving results. Thislevel also provides organizations with stretch goals.35
is developed and documented for future reference. A nursenavigator, present during the case review, coordinates thetreatment plan and communicates it to the patient.NCCCP sites found the most challenging issue to thisMDC model was the time commitment needed from support staff to handle the bulk of the upfront work. Otherchallenges included: Obtaining physician buy-in Changing the physician mindset from the “status quo” Moving the tumor board lead from the pathologist tothe disease-specific physician Providing resources or benefits to physicians to makeMDC conference attendance possible.Face-to-face MDC (aka MDC Clinic). In this model, allMDC team members meet with the cancer patient in oneroom to discuss treatment options. An important benefitof this model is that the patient is able to leave the MDCclinic with a completed treatment plan. The nurse navigatorensures that the patient understands the treatment plan andassists with the coordination of diagnostic tests, treatments,and follow-up visits.Though multidisciplinary clinics are enhanced byhaving all team members available as needed rather thanrequiring patients to schedule more appointments at otherlocations, this model is often not feasible for many community cancer centers. Barriers to the implementation of thismodel include: Availability of adequate MDC clinic space Coordination of team member schedules to fit theclinic time Physician buy-in (clinic productivity and therefore revenue is decreased under this MDC model) Ability of support staff to assemble all necessaryreports, test results, and imaging scans prior to theface-to-face MDC clinic meeting.Virtual MDC. NCCCP sites that did not have the physical space to hold team meetings or that could not haveface-to-face clinics due to distance between team members implemented virtual MDCs. In this model, membersof the MDC team see the cancer patient at different timesand places within a specified time frame. A treatment planis developed, written, and sent to all team members, as wellas the patient and primary care physician. A nurse navigator assists the patient through the process to ensure that allappointments are met and that all diagnostic and treatmentinformation is communicated to the MDC team.NCCCP sites found two major challenges to the virtual MDC model: How to identify the needs of MDC team members How to identify the gaps in communication and closethose gaps to ensure timely and accurate communication of the treatment plan.During the three-year pilot period, NCCCP sites initiated27 new MDCs, increasing the total number from 47 to 83.At the end of the assessment period, 36 MDCs were functioning in the five most common disease-specific MDCs:breast, lung, colorectal/GI, prostate/GU, and head andneck. NCCCP sites that were able to implement particulardisease-specific MDCs showed significant improvementsin the level of MDC care as measured with metrics, such36as the number of physicians participating and the percentof patients prospectively presented. Though three of theNCCCP sites did not have functioning MDCs at the endof the initial three-year pilot, these sites were able to demonstrate steps taken toward establishing multidisciplinarycare delivery levels.Based on the outcomes of the MDC evaluation andimplementation efforts, NCCCP sites identified two keyroles as crucial to successful MDC development: an effective physician leader and an experienced nurse navigator.Physician LeaderNCCCP sites found that effective physician leadership wasessential to influence movement to higher levels of MDCdevelopment and was a major component of successfulimplementation and maintenance of MDC in a communitycancer center. An effective physician leader has a scope ofauthority and accountability to: Oversee the development and implementation of theMDC program Provide leadership for the vision and strategic plan forthe MDC program Have report relationships and authority within theorganization that enable the physician leader to beaccountable for the MDC program Be an active participant in the MDC program, asappropriate.To be most effective, NCCCP sites believe that the physicianleader should be an active oncology clinician who is skilled atdeveloping peer relationships. An effective physician leaderwill help ensure continued physician participation in MDC.Why? A physician who serves as a champion for MDC willengage private practitioners in a process that respects theirschedules, yet allows for participation in MDC, either inperson or virtually. Interest and involvement by physiciansin the community, as well as cancer-center-employed physicians, offers many benefits, including: Wider participation by physicians overall Broader overall knowledge base Wider range of physician perspectives and greater consensus.Nurse NavigatorThe second influential factor for successful MDC development and implementation is the engagement of an experienced nurse navigator. The standard role of the navigator is to: Help guide the patient and family through the healthcare system Act as the central contact for patients and families Ensure that the patient and family understand the diagnosis and treatment plan Assist patients with scheduling tests and consultations.An experienced nurse navigator can facilitate multidisciplinary care and provide open communication between alldisciplines. A navigator has the process knowledge to coordinate patient schedules, will follow-up on care planning,and will communicate with the patient and the MDC team.When patients are not able to see all disciplines at the sametime, on the same day, or at the same location, the navigatorwill help guide the patient through the process. Even community cancer centers that are able to offer face-to-face MDCOncology Issues January/February 2011
find the support of a nurse navigator important in addressingthe needs of the patients beyond the MDC.sitate additional, time-consuming planning efforts andrequire physician dialogue to gain buy-in.Other StakeholdersIn addition to the physician leader and nurse navigator,NCCCP sites found that expansion of MDC at a cancercenter involved other key stakeholders including: Cancer patients Hospital or cancer center leadership Cancer program director Medical and radiation oncologists Pathologists Surgeons (both oncologic and other specialists) Primary care physicians Cancer registrar and staff Research and clinical trials staff Medical geneticists Legal departments Hospital staff Social workers Dietitians Community outreach staff.Recommendations and ConclusionIn the end, NCCCP sites gained many valuable insightsthrough the process of developing the MDC assessmenttool and expanding multidisciplinary care at their cancercenters. As a group, they offer a stepwise approach with thefollowing recommendations to other community cancercenters interested in establishing or enhancing MDC: Recognize that effective physician leadership is essential for MDC success Gain support of hospital or cancer center leadership toacknowledge the benefits of the physician leader role Utilize a MDC model that will succeed (e.g., implement MDC for a disease site that has a high volume anda willing physician leader) Develop a process that makes it easy for private practice physicians to participate (e.g., provide specific benefits to participating physicians, such as offering CMEcredits or allowing access to specialized equipment andtechnology at the clinic) Accept the need for flexibility as no one model will besuitable for all services Be willing to adapt or make changes to the processimmediately in order to use MDC team members’ timewisely and efficiently Recognize the importance of available support staffto address patient needs—beyond clinical care—thatcould be barriers to completing care Engage an effective nurse navigator with knowledge ofthe process to coordinate patient schedules Understand that not every community cancer center ismeant to reach a level five for all key elements in theMDC assessment tool to measure success.Barriers to MDC ImplementationNCCCP sites found that the most common barrier acrossall types of MDC models was the inability to schedule private practice physician time, resulting in a lack of physicianengagement. The community oncology physician’s scheduleis complicated by decreasing revenues. Today, these physicians have to see more patients to receive the same compensation, and this scenario results in tight schedules that do notaccommodate time for MDC participation
insufficient for a comprehensive program. Level 3—MDC Program Organizations at this level have many of the fundamental structures and processes for running MDC initiatives. Leadership’s vision for quality is known to many in the organization.