Transcription
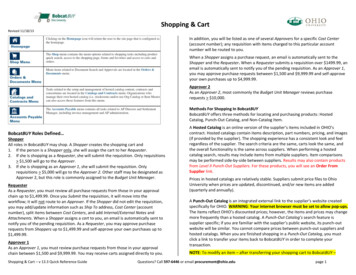
2021DESK REFERENCEoptum360coding.comFind product details and features —including item number, ISBN number andavailability date — quickly and easily.Intuitive product organizationStreamlined checkoutOptum360 coding products areorganized by category so you can findwhat you need quickly and easily.View and edit your cart, ship to multiplerecipients, add payment information,assign a PO number and complete yourpurchase — all on one page.Sign in to check outSigning in prior to checkout ensuresyour online and offline transactions areseamlessly linked to the same account foryour convenience. Don’t have an onlineaccount? It’s easy to create one — visitoptum360coding.com/register.Visit optum360coding.comView all your accountinformationGet immediate access to your order andinvoice history, track shipments, renew aproduct, create a wish list or update yourcontact information. 2020 Optum360, LLC. All rights reserved.WF2305592 04/20PLEEffortlessly view our new website onany device — desktop, tablet orsmartphone — optum360coding.comis with you wherever you go.Product information atyour fingertipsAnswers to your toughest CPT coding questionsMDevice-friendly shoppingCoders DeskReference forProceduresSAThe redesigned optum360coding.com offers new conveniences and the same greatcoding resources you’ve always trusted for a convenient, seamless shopping experience.Coders Desk Referencefor ProceduresSeamless shopping starts here.CDR21/CDR Made in the USA2 0 22optum360coding.comCDR CDR21 CVR Final.indd 110/21/2020 9:43:50 PM
ContentsReimbursement Terms .35Clinical Abbreviations, Prefixes, Suffixes,and Acronyms .57Procedural Eponyms .101Surgical Terms .119PLEIntroduction .1Format .1Using CPT Codes .1Using CPT Modifiers .1Using E/M Codes .1Reimbursement Terms .1Clinical Abbreviations, Prefixes, Suffixes,and Acronyms .1Procedural Eponyms .1Surgical Terms .2Anatomical Illustrations .2CPT Lay Descriptions .2MUsing CPT Codes .3History of CPT .3The CPT Book Conventions .3Format .4Resequencing of CPT Codes .4Symbols and Appendix B . 10Modifiers . 11Glossary of Terms . 11Using CPT Modifiers . 15SAUsing E/M Codes . 23Types of E/M Services . 23Levels of E/M Services . 24Documentation Guidelines forEvaluation and ManagementServices . 24 2021 Optum360, LLCAnatomical Illustrations .133CPT Lay Descriptions .167Integumentary .167Musculoskeletal .190Respiratory .337Cardiovascular .371Hemic/Lymphatic .453Mediastinum and Diaphragm .459Digestive .460Urinary .539Male/Female .572Maternity Care and Delivery .614Endocrine .621Nervous .624Eye and Ocular Adnexa .665Auditory .692Radiology .702Pathology and Laboratory .757Medicine .886Evaluation and Management .962Category III .975i
Coding is a complicated business. It’s not enough tohave a current copy of a CPT book. Medical codersalso need dictionaries and specialty texts if they are toaccurately translate physicians’ operative reports orpatient charts into CPT codes.Using CPT ModifiersModifiers augment CPT codes to the satisfaction ofprivate and government payers. Optum360 codingexperts interpret CPT modifiers and identify theiradvantage in reimbursement.Using E/M CodesAlthough some of the most commonly used codes byphysicians of all specialties, evaluation andmanagement (E/M) codes are amongst the leastunderstood. These codes, introduced in the 1992 CPTbook, were designed to increase accuracy andconsistency in the reporting of non-proceduralencounters. This section contains new 2021guidelines and a summary of E/M services andguidelines, along with information from the 1995 and1997 documentation guidelines.PLEThat’s why Optum360 originally developed Coders’Desk Reference—now known as Coders’ Desk Referencefor Procedures—to provide a resource with answers toCPT coding questions. We polled the medicalreimbursement community and our technical staff todetermine the issues causing bottlenecks in a coder’sworkload.IntroductionIntroductionWe know that experienced coders are frustrated bylimited definitions accompanying many CPT codes.Beginning coders need guidelines on the use of CPTcodes and basic information about medical andreimbursement issues. Everyone requires up-to-dateinformation about the anticipated changes inprocedural coding.MCoders’ Desk Reference for Procedures (CDR) answersthe questions of both experienced and novice medicalcoders. Coders, physicians, registered nurses,physician assistants, and physical therapistscontributed to the technical information contained inCDR. The result is a compendium of answers to a widevariety of CPT coding questions.SASince the first release of CDR in 1995, coders’corrections, suggestions, and tips have beenincorporated into every printing, making this book asinformative and useful as possible. Changes reflectingthe dynamic world of coding are ongoing, andOptum360 encourages input for inclusion in futureeditions of the book. Information in CDR has beenupdated to reflect 2021 CPT codes.FormatCDR is divided into convenient sections for easy use,with each section organized in alphabetic or numericorder. Simply access the section by thumbing throughthe convenient tabbing system to find the specificitem of interest.Using CPT CodesFor the new coder, and even for the veteran, thischapter provides an overview of the CPT book: what itis and how best to use this coding system foridentifying procedures. 2021 Optum360, LLCReimbursement TermsIn order to get reimbursed in a timely manner, it isimportant to have a clear understanding of theterminology used by major insurers and the federalgovernment. This section includes up-to-dateterminology that will help coders have a betterunderstanding of the complex reimbursementclimate.Clinical Abbreviations, Prefixes,Suffixes, and AcronymsThe medical profession has its own shorthand fordocumentation. Here, acronyms, abbreviations, andsymbols commonly seen on operative reports ormedical charts are listed for easy reference.The uniquely efficient language of medicine is basedon prefixes and suffixes attached to root words tomodify the meaning. Medical prefixes and suffixesevolved from the Greek and Latin used by pioneeringphysicians.Procedural EponymsWhat is the Mitrofanoff operation? What is the Binettest? Eponyms honor the developer of a procedure ortest, but do little to clarify what the procedure is.Subject matter experts have researched theprocedural eponyms found in the index of the CPTbook or used by surgeons and other medicalpersonnel in medical reports, and provide simplifiedexplanations of what the procedures are, along withapplicable CPT codes.CPT 2021 American Medical Association. All Rights Reserved.1
Using CPT ModifiersModifiers allow coders to indicate that a service wasaltered in some way from the stated CPT descriptionwithout actually changing the basic definition of theservice. Modifiers are considered an essentialcomponent of accurate coding. Some modifiersimpact reimbursement and others identify specialcircumstances. Modifiers can indicate the following: A service or procedure was performed by morethan one physician Only part of a service was performed An adjunctive service was performed A bilateral procedure was performed A service or procedure was provided more thanonce Unusual events occurred A procedure or service was more difficult or tooklonger or was less involved or required less timePLEA service or procedure represents only aprofessional or technical componentModifier 22 often produces an automatic review oraudit by payers. If the operative report attached to theclaim does not indicate appropriate use of themodifier, the increase in payment will be denied.Periodic training for all involved in the coding processis important from both a legal and reimbursementperspective.Because modifier 22 is often used when complicationsare encountered during surgical procedures, medicalnecessity is substantiated by additional diagnosticcodes that identify the complication. These diagnosticcodes should reflect the operative condition and thecomplication(s) encountered during the surgery.23Unusual Anesthesia2224MPhysical status modifiers, P1-P6, specifically used foranesthesia services, are not discussed in this chapter.HCPCS modifiers, beginning with an alpha character,may be appended to CPT codes in specificcircumstances and are also not discussed in thischapter.This modifier is used by anesthesiologists to indicatethat this procedure is normally performed under localanesthesia or regional block but due to unusualcircumstances, general anesthesia is needed. Thismodifier is not appropriate for use with codes thatinclude the term “without anesthesia” in thedescriptor, or for procedures normally performedunder general anesthesia.Increased Procedural ServicesSAModifier 22 is not appropriate for CPT codes with theterm “simple” as part of the code description, norshould it be appended to a code for an E/M service.Rather, modifier 22 is used to indicate that aprocedure was complicated, complex, difficult, or tooksignificantly more time than usually required by theprovider to complete the procedure. Documentation,including notations to the amount of time involved,should be provided with the billing and kept in themedical record when this modifier is used. Timenotations in the documentation should include startand stop times, as well as the total amount ofadditional time required to complete the procedure.The provider should clearly state specifically, and indetail, what issues made the procedure more complexrather than simply using vague statements such as,“The patient had a lot of adhesions.” When modifier22 is used, an operative report should always beattached to the claim.The fee reported for modifier 22 should be the usualand customary amount for the procedure plus anadditional amount for the unusual circumstances. If 2021 Optum360, LLCUnrelated Evaluation and Management Serviceby the Same Physician or Other QualifiedHealth Care Professional During aPostoperative PeriodThis modifier reports that an unrelated E/M servicewas provided by the surgeon within the global period.Use of this modifier needs to be correlated to adiagnosis code that is unrelated to the surgicaldiagnosis code.25Significant, Separately IdentifiableEvaluation and Management Service by theSame Physician or Other Qualified Health CareProfessional on the Same Day of the Procedureor Other ServiceThis modifier indicates that on the same day aprocedure or service identified by a CPT code isperformed, the patient’s condition required asignificant, separately identifiable E/M code beyondthe usual level of service required for the procedure. Inaddition, the modifier denotes that the patient’scondition required services that were over and aboveCPT 2021 American Medical Association. All Rights Reserved.15Using CPT Modifiers modifier 22 is appended to a code that is not theprimary code, and modifier 51 has been appended,modifier 22 should be paid in addition to the cutcontract rate paid for the code.
Using E/M Codesguidelines. The professionals within this definition areseparate from “clinical staff" and are able to practiceindependently. CPT defines clinical staff as “a personwho works under the supervision of a physician orother qualified health care professional and who isallowed, by law, regulation, and facility policy toperform or assist in the performance of a specifiedprofessional service, but who does not individuallyreport that professional service.” Keep in mind thatthere may be other policies or guidance that canaffect who may report a specific service.PLEThis section provides an overview of evaluation andmanagement (E/M) services, tables that identify thedocumentation elements associated with each code,and the federal documentation guidelines withemphasis on the 1997 exam guidelines. This set ofguidelines represents the most complete discussionof the elements of the currently accepted versions.The 1997 version identifies both general multi-systemphysical examinations and single-systemexaminations, but providers may also use the original1995 version of the E/M guidelines; both are currentlysupported by the Centers for Medicare and MedicaidServices (CMS) for audit purposes.The levels of E/M services define the wide variations inskill, effort, and time and are required for preventingand/or diagnosing and treating illness or injury, andpromoting optimal health. These codes are intendedto represent physician work, and because much of thiswork involves the amount of training, experience,expertise, and knowledge that a provider may employwhen treating a given patient, the true indications ofthe level of this work may be difficult to recognizewithout some explanation.MAt first glance, selecting an E/M code may appear tobe difficult, but the system of coding clinical visits maybe mastered once the requirements for code selectionare learned and used.ProvidersSAThe use of the phrase “physician or other qualifiedhealth care professional” (OQHCP) was adopted toidentify a health care provider other than a physician.This type of provider is further described in CPT as anindividual “qualified by education, training,licensure/regulation (when applicable), and facilityprivileging (when applicable).” State licensureguidelines determine the scope of practice and aqualified health care professional must practice withinthese guidelines, even if more restrictive than the CPTguidelines. The qualified health care professional mayreport services independently or under incident-to 2021 Optum360, LLCWhen approaching E/M, the first choice that aprovider must make is what type of code to use. Thefollowing tables outline the E/M codes for differentlevels of care for: Office or other outpatient services—new patientOffice or other outpatient services—establishedpatientHospital observation services—initial care,subsequent, and dischargeHospital inpatient services—initial care,subsequent, and dischargeObservation or inpatient care (includingadmission and discharge services)Consultations—office or other outpatientConsultations—inpatientEmergency department servicesCritical careNursing facility—initial servicesNursing facility—subsequent servicesNursing facility—discharge and annualassessmentDomiciliary, rest home, or custodial care—newpatientDomiciliary, rest home, or custodialcare—established patientHome services—new patientHome services—established patientProlonged services—with direct patient contactProlonged services—without direct patientcontactProlonged clinical staff services with physician orother qualified health care professionalsupervisionStandby servicesCPT 2021 American Medical Association. All Rights Reserved.23Using E/M CodesThe AMA advises coders that while a particular serviceor procedure may be assigned to a specific section,the service or procedure itself is not limited to useonly by that specialty group (see paragraphs 2 and 3under “Instructions for Use of the CPT Codebook” onpage xiii of the CPT Book). Additionally, theprocedures and services listed throughout the bookare for use by any qualified physician or otherqualified health care professional or entity (e.g.,hospitals, laboratories, or home health agencies).Types of E/M Services
Coders’ Desk Reference for Proceduresurgent admission. Admission in which the patientrequires immediate attention for treatment of aphysical or psychiatric problem.USP. United States pharmacopoeia.USPHS. United States Public Health Service.USPSTF. U.S. Preventive Services Task Force.utilization review. Formal assessment of the medicalnecessity, efficiency, and/or appropriateness of healthcare services and treatment plans on a prospective,concurrent, or retrospective basis.utilization review nurse. Nurse who evaluates casesfor appropriateness of care and length of service andcan plan discharge and services needed afterdischarge.PLEto improve the health of all U.S. citizens by makingevidence-based recommendations about clinicalpreventive services such as screenings, counselingservices, and preventive medications. Task Forcerecommendations are published on the organization’swebsite and/or in a peer-reviewed journal. Membersinclude experts in various fields such as preventivemedicine and primary care, including internalmedicine, family medicine, pediatrics, behavioralhealth, obstetrics and gynecology, and nursing. All ofthe expert recommendations go through rigorousreviews of existing peer-reviewed evidence with thegoal and objective of assisting primary care cliniciansand patients in determining whether a preventiveservice is right for the patient’s needs.Recommendations from the organization receive aletter grade (e.g., A, B, C, or D) or an I statement that isassigned on the strength of the evidence and thebalance of benefits and harms of a preventive service.The Task Force does not factor in costs whendetermining a recommendation grade. All Task Forcerecommendations are applicable only to patients whopresent without signs or symptoms of the specificdisease or condition under evaluation, and therecommendations address only services offered in theprimary care setting or services referred by a primarycare clinician.Reimbursement TermsUB-04. Uniform institutional claim form developed bythe NUBC that was implemented in May 2007.MUCR. Usual, customary, and reasonable. Fees chargedfor medical services that are considered normal,common, and in line with the prevailing fees in agiven geographical area. May also be referred to ascustomary, prevailing, and reasonable charges.SAunbundling. Separately packaging costs or servicesthat might otherwise be billed together includingbilling separately for health care services that shouldbe combined according to the industry standards orcommonly accepted coding practices.underwriting. Evaluating and determining thefinancial risk a member or member group has on aninsurer.unlisted procedure. Procedural descriptions usedwhen the overall procedure and outcome of theprocedure are not adequately described by anexisting procedure code. Such codes are used as a lastresort and only when there is not a more appropriateprocedure code.upcoding. Practice of billing a code that represents ahigher reimbursement than the code for theprocedure actually performed.URAC. Utilization Review Accreditation Commission.Accrediting body of case management. 2021 Optum360, LLCverification of eligibility. Process by which the payeror provider determines that the beneficiary iscurrently enrolled in a plan and that the requestedservices are covered by the plan.violation. Disregard or abuse of the laws, rules, orguidelines, knowingly or unknowingly resulting inreceipt of inappropriate reimbursement.waived test. Laboratory test defined by CLIAstandards that can be conducted in a minimallaboratory setting with minimal chance of error.waiver of liability. Provision established by Medicareto protect beneficiaries and physicians from liabilitywhen services are denied as inappropriate ormedically unnecessary. Under the provision, if theMedicare beneficiary knew or should have known thatthe services billed for were not covered, thebeneficiary is liable for paying for the services. Ifneither the beneficiary nor the hospital knew orreasonably could have been expected to know thatthe services were not covered, Medicare is liable forpaying the claim. If the provider should have knownand the beneficiary is protected from liability, thenliability falls with the provider, and the hospitalcannot bill the beneficiary for services other thandeductibles and coinsurance amounts, even thoughno Medicare payment has been made. Beneficiarieswho do not know that services were noncovered areprotected from liability when the services are notreasonable and/or necessary (including adverse levelof care determinations) and when custodial care isinvolved.waste. Spend or use federal funds carelessly.weighting. Assigning more worth to a fee based onthe number of times it is charged, weighting theresource-based relative value fees for an area.55Reimbursement Termsunspecified. Codes for use when documentation isinsufficient to assign a more specific code.value-added network. Vendor of electronic datainterchange data communications and translationservices.
Severe pain.Pain.Denoting an enzyme.Weakness.Closure, occlusion.Incomplete cellular development.Puncture.Relating to the head.Small or little.Having to do with cells.Relating to the fingers or toes.Binding or fusion.Excision, removal.Blood.Produces, causes, or brings about.Drive out or expel.Production, causation,generation.Drawn, written, and recorded.Written or drawn.State of being, , free, reduction of.Destroy, breakdown.Scientific measurement.Indicates pain or discomfort.Indicates likeness orresemblance.Study of.Tumor.Relating to -lytic-metry-odynia-oid-ology-oma-opathy 2021 Optum360, -osis-ostomySurgical fixation.Surgical repair.Suturing.Hemorrhage.Suturing.To examine.Condition, process.Indicates a surgically createdartificial opening.Indicates a cutting.Crushing, destroying.Indicates fixed or joined together.Indicates weakness.Indicates a feeling, diseasedcondition, or therapy.Indicates a deficiency, less thannormal.Fixation.Inordinate love of or craving forsomething.Abnormal fear of or aversion to.Indicates growth, growing.Indicates surgically formed ormolded.Indicates a stroke or paralysis.Relating to breath, breathing.Indicates producing or making.Indicates activity, action,condition, or use.Indicates bleeding or other fluiddischarge.Indicates a suture or seam joiningtwo structures.Indicates an abnormal orexcessive fluid discharge.Splitting or breaking.Malignant tumor of flesh orconnective tissue.Contraction.Arrangement, grouping.Incision.PLEThe acronyms, abbreviations, prefixes, suffixes, andsymbols used by health care providers speedcommunications. The following list includes the mostoften seen acronyms, abbreviations, and symbols. Insome cases, abbreviations have more than onemeaning. Multiple interpretations are separated by aslash (/). Abbreviations of Latin phrases arepunctuated.AbbreviationsClinical Abbreviations,Prefixes, Suffixes, -spasm-taxy-tomy57
Anatomical IllustrationsCoders’ Desk Reference for ProceduresMusclesTemporalis m.Frontalis m.Orbicularis oculi m.Orbicularis oris m.Depressor labii inferioris m.Mentalis m.Sternocleidomastoid m. (clavicular head)Sternocleidomastoid m. (sternal head)Linea albaTriceps m.Brachialis m.Rectus abdominis m.Brachioradialis m.Pronator teres m.Flexor carpi radialis m.Extensor carpi radialislongus m.Extensor carpi radialisbrevis m.Extensor digitorum m.Anteriorsuperioriliac spineMBrachioradialis m.Extensor carpi radialislongus m.Bicipital aponeurosisExternal oblique m.Flexor carpi radialis m.Palmaris longus m.Flexor carpi ulnaris m.Flexor digitorumsuperficialis m.ExtensorretinaculumLatissimus dorsi m.Coracobrachialis m.Serratus anterior m.Biceps brachii m.PLEBiceps brachii m. (short head)Biceps brachii m. (long head)Masseter m.Zygomaticus major m.Splenius m.Omohyoid m.Levator scapulae m.Platysma m.Deltoid m.Pectoralis major m.Extensor digiti minimi m.Extensor retinaculumIliopsoas m.Pectineus m.Adductor longus m.Sartorius m.PubictubercleGracilis m.Tensor fascia latae m.Rectus femoris m.Vastus lateralis m.SAAnatomical IllustrationsVastus medialis m.TibiaSoleus m.Medial malleolus136Tensor fascia latae m.PatellaGastrocnemius m.Tibialis anterior m.Peroneus longus m.Extensor digitorum longus m.Superior extensor retinaculumLateral malleolus 2021 Optum360, LLC
21600Coders' Desk Reference for Procedures21600The physician removes part of one rib. With the patientunder anesthesia, the physician makes an incision inthe skin of the chest overlying the rib. The tissues aredissected deep to the rib itself. The rib is identified.The physician removes the desired part of the rib usinga saw and other instruments. The remaining pieces ofthe rib and the wound itself are irrigated and debrided.The incision is sutured in layers.21602-2160321620The physician removes a portion of the sternum fromthe chest. With the patient under anesthesia, thephysician makes an incision in the skin overlying thesternum. This is carried deep through thesubcutaneous tissues to the bone. The sternum isidentified and the attached soft tissues are dissectedfrom the bone. The physician marks the portion of thesternum to be removed. The bone is cut in theappropriate places using a saw and other surgicalinstruments. The remaining portion of the bone isirrigated and smoothed as needed. The wound isclosed in layers and a dressing is applied.PLEThe physician excises a chest wall tumor, includingribs. An incision in the skin of the chest overlying thesite of the tumor is made. The tumor and surroundingtissue are excised. The tissue removed includes at leastone adjacent rib above or below the tumor site andany associated intercostal muscles. It may also includerib cage resection and/or an en bloc resection ofmuscles, including the pectoralis minor or major, theserratus anterior, or the latissimus dorsi. The physicianligates or cauterizes bleeding vessels. A chest tubemay be placed to re-expand the lung. The incision isrepaired with layered closure and a pressure dressingis applied to the wound.21627The physician performs a debridement of the sternum.With the patient under anesthesia, the physician makesan incision in the skin overlying the sternum. Theincision is carried deep to the bone. The sternum isdebrided as warranted using any of a variety of handor powered surgical instruments. Irrigation is used sothat debridement can be completed as extensively asindicated. The wound may be loosely packed and adressing applied or it may be closed in layers and adressing applied.21630-21632The physician removes most or all of the sternum fromthe chest. With the patient under anesthesia, thephysician makes a long incision overlying the sternumand anterior chest. This is carried deep to the bone.Dissection is performed around the sternum. Ribs aredisarticulated as needed and thorough debridementis accomplished. Using saws and other surgicalinstruments, the physician removes the bone. Internalfixation devices (reported separately) are often neededto support the ribs and chest wall. The wound isirrigated and closed in layers. Report 21632 if amediastinal lymphadenectomy is performed duringthe procedure.MThe physician excises a chest wall tumor, involvingribs, with plastic reconstruction. The physician makesan incision in the skin of the chest overlying the tumor.The tumor and surrounding tissue are excised andincludes at least one adjacent rib above and below thetumor site and all intervening intercostal muscles. Itmay also include an en bloc resection of muscles,including the pectoralis minor or major, the serratusanterior, or the latissimus dorsi. In 21603, lymphatictissue lying within the mediastinum is also removed.The physician ligates or cauterizes bleeding vessels. Achest tube may be placed to re-expand the lung. Plasticreconstruction is done and may involve rib graftsand/or a myocutaneous flap. A pressure dressing isapplied to the wound.SAMusculoskeletal21601A dressing is applied. Report 21616 if a sympatheticnerve pathway is cut during the procedure.21610The physician resects the costovertebral joint. Thephysician makes a posterior incision overlying the joint.The tissues are dissected from the joi
Using CPT Codes For the new coder, and even for the veteran, this chapter provides an overview of the CPT book: what it is and how best to use this coding system for identifying procedures. Using CPT Modifiers Modifiers augment CPT codes to the satisfaction of private and government payers. Optum360 coding