Transcription
Ministry of Health Viet NamNational Expanded Program on ImmunizationComprehensive Multi-Year PlancMYP for Extended Program on Immunization 2016-2020Ha Noi, August 2015
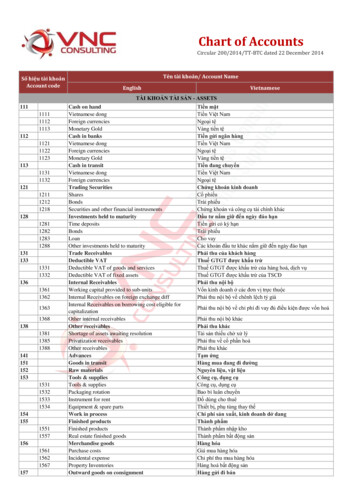
ContentsAcronyms . 1Executive Summary . 21.Situational Analysis . 41.1.Country Profile . 41.2.National EPI Program . 51.2.1.Management and Financing . 61.2.1Immunization Service Delivery . 81.2.2Coverage and Reporting of Vaccine Preventable Diseases . 111.2.3Cold Chain and Vaccine Management . 131.2.4Immunization safety and AEFI. 131.3.2.3.Achievements in 2011-2015 . 15Comprehensive Multi-Year Plan for EPI: 2016-2020 . 162.1.National Objectives, Strategies and Key Activities 2016-2020 . 162.2.Key Activities . 21Financial Sustainability of the cMYP 2016-2020. 233.1.Cost and financing of the Viet Nam National cMYP . 233.1.1.Background . 233.1.2.Summary of key findings on financing of the NEPI . 243.1.3.Key assumptions . 253.1.4.Findings on Baseline Expenditures . 263.1.5.Future resource requirements . 293.1.6.Future financing and funding gap analysis . 343.1.7.Future Financial Sustainability . 35Annexes . 37
AcronymsAEFIAdverse Events Following ImmunizationAD syringesAuto-Disabled SyringesBCGBacille-Calmette Guerine Vaccinec-VDPVCirculating-Vaccine derived polio virusCBAWWomen in Child-bearing age groupDTPDiphtheria -tetanus-pertussis vaccineDTP3Third dose of DTP vaccineEPIExpanded Program on ImmunizationHepB3Third dose of hepatitis B vaccineHPVHuman PapillomavirusHWHealth WorkersGAVI AllianceGlobal Alliance for Vaccines and ImmunizationGIVSGlobal Immunization Vision and StrategyHCWsHealth community workersICCInteragency Coordination CommitteeIECInformation Education CommunicationIPVInactivated polio vaccineJEJapanese EncephalitisJICAJapan International Cooperation AgencyMNTEMaternal and Neonatal TetanusMSV1Measles vaccine first doseMSV22nd dose of measles vaccineMRMeasles-Rubella combination vaccineNRANational Regulatory AuthorityNEPINational Expanded Program on ImmunizationOPVOral Polio VaccineOPV3Third dose of OPV vaccinePATHProgram for Appropriate technologies in Health, an international NGOPCVPneumococcal Conjugate VaccineSIASupplementary Immunization ActivitySNIDSub-national Immunization DaysVPDVaccine Preventable DiseasesVHWsVillage Health WorkersUNICEFUnited Nations Children FundWHOWorld Health Organization1
Executive SummaryIMMUNIZATION SITUATIONALImmunization AchievementsImmunization Coverage1. DPT coverage - 95%2. Coverage of fully immunized children 75.6%3. DPT1 – DPT3 drop out 7.7%4. 94% of districts with above 80% of DPT3coverage5. Polio coverage – 96%6. Service delivery strategy is developed7. Recurrent budget for EPI staff salaries8. Functional AFP surveillance system979595952014201559201120122013Immunization System AnalysisHealth System Constraints1. Immunization services are available at alllevels and functioning through wellestablished provider network2. Coverage is not uniformly high amongsome population groups3. Outreach services targeting hard-to-reachpopulations stopped in some districts4. Existence of non-EPI immunizationsystem with different immunizationschedule1. Overall investment on EPI is insufficient at alllevels2. Limited outreach and mobile activities3. High staff turnover and new staff4. Multiple tasked staff beyond EPI and lack oftime for regular supervision aditional burdenof health staff5. Inequitable distribution of vaccinatorsBaseline Costing ProfileIndicators2014Total Immunization Expenditures ( ) 60,905,828Campaigns ( ) 33,796,428Routine Immunization only ( ) 27,109,400per capita ( )per DTP3 child ( ) 0.30 16% Vaccines and supplies80.8%% Government funding61.1%% Total health expenditures0.3%% Gov. health expenditures0.6%% GDPTotal Shared Costs ( )% Shared health systems costTOTALBaseline Financing PPLIES13% 17,804,60122.6%UNDERUSEDVACCINES49% 78,710,4292
ANALYSIS SUMMARYcMYP SUMMARY 2016 – 2020Immunization Priorities1.2.3.4.5.6.7.8.Immunization Goals and ObjectivesPolio eradicationMeasles and Rubella eliminationHepatitis B accelerated controlAccelerated control of JapaneseEncephalitisMeeting regional vaccination coverageratesImmunization of populations in hard toreach areasImprove cold chain equipmentIntroduce IPV and RotaIndicatorMonitoring Framework2012 2018Cases of measles per millionpopulation (#)Cases of polio (#)Neonatal deaths per 100,000newborns (#)DPT3 coverage (%)% pregnant women have TT2% Children fully immunized% District with 80% DPT3 coverage% dropout between DPT1 – DPT3PCV3 coverage aintain polio free statusControl diphtheria and pertussisEliminate measles and rubellaControl Hepatitis BReaching over 90% coverage of three doses ofJE6. Maintain more than 95% coverage rates forall antigens at national level and DTP3coverage of 90% in all districts7. Reach over 90% coverage of fully immunizedchildrenPriority Immunization Program Strategies1. Reaching over 90% coverage of FIC forchildren under 1 years of age2. Reaching over 90% coverage for JE3 among2-5 year old children3. Measles elimination by 20174. Accelerated control of Hepatitis B5. Control of diphtheria and pertussis6. Vaccination of children in high-risk areaswith cholera and typhoid vaccine7. Implementation of JE SIA in the high riskareas8. Elaborate specific urban EPI communicationstrategySustainability Strategy1. Planning and implementation of resourcemobilization strategy2. Development of effective communicationplan3. Development and implementation ofprogram advocacy plan4. Revision of some targets as plannedHealth and Development Impacts1. Contribution in achievement of MDG Goal 5through improved child survival2. Reduced disability in the communityassociated with vaccine preventable diseaseCost and Financing Projections (US )201420152016Total resources required (US million) 64.3 85.3 71.62017 71.62018 72.0Cost per capita (in US ) 0.47 0.68 0.54 0.53 0.53Total secure financing (US million) 47.4 60.1 59.8 57.9 58.3Funding Gap (with secure) (US million) 16.9 24.7 11.8 13.6 13.7Total probable financing (US million) 16.10 27.00 22.70 19.70 19.50 16.9326% 64.3 0.47 24.729% 85.3 0.68 11.816% 71.6 0.54 13.619% 71.6 0.53 13.719% 72.0 0.53Funding Gap (with secured funds only) (US million)Per centage of funding gapTotal resources required (US million)Cost per capita (in US )
1. Situational Analysis1.1. COUNTRY PROFILEViet Nam (population 91.6 million) in recent years has experienced steady rates of economic growth andsocial development.The country is divided into 6 major geographical zones, including the Red River Delta, Northern midlandsand mountain areas, the North Central and Central Coastal areas, Central Highlands, South East and theMekong River Delta. The rapidly growing urban centers of Hanoi in the north (population 7.3 million),and Ho Chi Minh City in the south (population 7.9 million) could be considered as an additional highlyurbanized ecological zone.The country is divided administratively into 4 regions, 63 Provinces, 704 Districts, and 11,138 Communes.The health sector structure conforms to the administrative structures with a network of NationalHospitals, Provincial and District Preventive centers, and Commune Health centers, which are furthernetworked by a system of village health workers.Table 1 Basic Demographic Indicators Viet NamTotal population (2013)91,680,000Population Under 1523%Population Urbanised32%Gross national income per capita (PPP international , 2013)5,030Life expectancy at birth m/f (years, 2013)71/80Total expenditure on health per capita (Intl , 2013)308Total expenditure on health as % of GDP (2013)6.0Total Fertility rate1.7Under-five mortality rate (per 1000 live births)24Maternal mortality ratio (per 100 000 live births)49Viet Nam adopted a state funded health sector, with a recent administrative decree establishing freehealth care services for all children in Viet Nam under the age of six. 92% of deliveries take place infacilities.1 The country is also in the formative period of development of a nationwide health insurancesystem. In 2011 there were 13,506 health service facilities in the country. Viet Nam’s health system ishighly decentralized, with 93.9% of all facilities under the authority and management of local healthauthorities.21WHO Global Health Observatory Data 2013Dr Socorro Escalante - Health Systems Team Leader WHO Excerpt from: ‘WHO and Viet Nam – Health for All: now and into thefuture’ prepared for MOPAN by WHO24
The current health sector plan 2010-20153 identifies ten tasks for health sector development, seven ofwhich are directly relevant to the immunization program: Consolidating the health care delivery network especially grass-roots level Strengthening preventive medicine Strengthening population - family planning and reproductive health care Developing health human resources Developing health information systems Renovating health service operations and financial mechanisms Strengthening health sector management capacityThe new health sector strategic plan for 2016-2020 is in the stage of development and will be adopted bythe end of the year.1.2. NATIONAL EPI PROGRAMViet Nam has one of the strongest National EPI program in the region that has managed to reach andmaintain high coverage levels for all antigens included in the national immunization schedule. During theprevious cMYP cycle EPI has managed successful implementation of the MR SIA. In terms of the newvaccine introduction, Viet Nam National EPI take pro-active approach for realizing availableopportunities, through the work with the government and international developing partners.Despite of significant progress in the implementation of the National Immunization Program (NIP), therestill are policy and operational challenges, which are highlighted in the recent National EPI review andwhich are taken into account, while identifying national goals, strategies and objectives for the next fiveyear cMYP cycle.4The details on the most challenging areas and key aspects for consideration are represented below: The dual system of EPI public sector vaccines and fee for service non EPI vaccines result incomplexities and inconsistencies in reporting, immunization schedule and quality standards. Urban EPI strategy is becoming significantly more complex, with high rates of mobility andmigration, variable levels of commitment from city governments for operations, and service deliverychallenges associated with providing services in a very dense and mobile population setting. Hepatitis B birth dose coverage and timeliness of administration improved due to the significantimprovements in hospital immunization service providing during the last five year period. The introduction of MCV2 and DTP4 has been successful, through in some provinces morecommunication and social mobilization work will be required to reduce drop out. Scaling up of JE vaccination nationwide requires additional efforts for maintaining EPIachievements during the recent cMYP cycle.34Ministry of Health Vietnam Health Sector Plan http://www.wpro.who.int/health services/VTN 2011-2015.pdfNational EPI Review, August 20155
Chronic disadvantage experienced by specific at risk population groups in some locations, includingremote area residents, ethnic minorities, and mobile and migrant populations in both urban and ruralsettings. Reduction or cancellation of EPI outreach and mobile strategy in some locations, as the result of thepublication of Circular 12 on immunization safety, creating real threat to strategies to reduceinequities in access.1.2.1. MANAGEMENT AND FINANCINGIn terms of legal and regulatory frameworks, a Law on the Prevention and Control of infectious Diseases 5enacted in 2008 details in Article 27 and 28 the principles of use of vaccines and medical products, whichpoints out in particular that vaccines must be used for proper schedule and targets groups, and must alsobe used at qualified establishments. The National Regulatory Authority (NRA) in Viet Nam was recentlycertified by the WHO as having a fully functional regulatory system which will enable Viet Nam to ensurethe safety and efficacy of vaccines used or produced in Viet Nam.6 A decree on immunization is currentlybeing finalized with the Ministry of Health.As illustrated in the Error! Reference source not found., the National Expanded Program onImmunization (NEPI) is managed by the National Institute for Hygiene and Epidemiology. Thereafter,the program management is decentralized to Regional EPI offices (4), Provincial Preventive MedicineCenters (63), and District Preventive Medicine Centers (704). Immunization services are integrated intothe health service delivery model of the Commune Health centers, where immunization services arenormally provided in sessions for 1 - 3 days per month, supplemented by mobile health strategies forremote areas, and immunization campaigns for disease elimination and control activities.7A fee for service model of immunization for some vaccines also operates through public facilities. Theseservice providers are linked to a communication network of Village Health Workers, whose responsibilityinclude communication with and mobilization of the communities for immunization sessions as well asimplementation of the community based surveillance.5Government of Vietnam Law on Prevention and Control of Infectious Diseases Hanoi 2009WHO National Regulatory Authority of Viet Nam Meets International Standards for ediacentre/releases/2015/nra vietnam certification/en/67The last campaign was conducted in 2014 nationally (measles and rubella)6
Figure 1: NEPI StructureTable 2Table 2 below outlines the immunization schedule in Viet Nam. IPV, MR and Rotavirus vaccinesare under consideration for introductions in 2016 and 2017, suggesting that there are likely to be ongoingrevisions to the national immunization schedule.Table 2. Immunization Schedule and Program Development during the previous cMYP cycleVaccineBirthBCGX2M3M4M5M9MDTP18 MXTTPregnant women and women of childbearing age (High risk areas)HepBXJE2 doses in the first year at 1-2 weeks interval, and another dose in the 2nd yearMeaslesXOPVXXXDTP-HepB-HibXXXTyphoid1 dose for 3-10 years oldCholera2 doses at 1 month interval for 2-5 years old7X
The current comprehensive multi-year plan for immunization (cMYP) 2011-20158 identifies 12 mainstrategies for program development in 2011-2015, which include achieving measles elimination by 2012,improved control of hepatitis B and JE, elimination of invasive Hib disease by 2015, introduction of othernew and under-utilized vaccines including Measles-rubella (MR), pneumococcal conjugate vaccines, HPVand rotavirus and finally continuation of special vaccines (Typhoid and Cholera) in high risk areas. Insupport of global targets for polio eradication, the country was planning to introduce IPV vaccine in 2015,however the introduction was postponed for 2016.The national program is financed nationally through the MoH and increasingly through local governmentat the provincial and district level. Data provided by EPI shows an increasing trend for financing of EPI bythe national Government, as illustrated in Figure 2below. Data provided through the Joint ReportingForm system indicates that the proportion of the national program funded by the government is 44% in2014, up from 39% in 2010.9Figure 2. Government Funding of EPI (billion 41.2.1 IMMUNIZATION SERVICE DELIVERYOverall, the review teams observed a consistent and robust immunization service delivery strategy acrossthe reviewed provinces.There is a high level of demand and social mobilization, as is evident from the fact that most vaccinationsare provided through health facility sessions that take place two to three days every month. Given thepreliminary findings from the immunization coverage survey indicate high DTP3 coverage (90%), thenthis service delivery strategy (in the context of Viet Nam) could be considered both highly effective andvery efficient.However, the EPI review identified a number of service delivery challenges in both the current andupcoming planning cycle.Fee for Service Immunization and Alignment with Policy and Reporting8Ministry of Health EPI Multi-Year Plan for EPI 2011-2015WHO Immunisation Monitoring Data base WHO GVA 2015http://apps.who.int/immunization %5Bcountry%5D%5B%5D VNM&commit OK10 10National EPI Review. Vietnam August 6 201598
The first challenge relates to the operation of the “dual system” of EPI immunization and the “non-EPI”fee for service model that operates simultaneously in health facilities across the country. This strategy,though innovative, presents following major policy and operational questions:-Existing system of double standards of care.There is concern that a system of double standards of care is operating, whereby families who use servicepayments for EPI can access this service any day of the month in contrast to free-of-charge provision ofEPI vaccines, which can be accessed only 2-3 days per month.-Usage of different vaccines by the EPI and non-EPI immunization models.Currently, different vaccines are provided according to a different immunization schedule (e.g. MR andMMR), raising concerns as to the degree to which this may be causing confusion in public health strategyfor control of vaccine preventable diseases.-Different standards for monitoring vaccine management quality.There are concerns with regards to some standards for monitoring quality of vaccine management, whichmay differ between the EPI immunization program and the “non-EPI”, fee for service immunizationmodels.-EPI and non-EPI immunization service providers.Human resources for EPI and non-EPI vaccines are the same, but allocation of time between activitiesrelated to EPI and non-EPI is unclear.-Different reporting, recording and vaccine management in the EPI and non-EPI immunizationservice delivery.There’s a lack of clarity on how fee for service immunization reports to the public health sector, whichraises some doubt as to the real coverage of EPI vaccines on the public routine immunization schedule.Taking into account importance of the aspects reflected above, strengthening of immunization Policy toset a consistent set of guidance and standards for implementation of a nationwide immunization andstrategy calls to particular attention.Immunization Safety and Outreach ServicesThe outreach service provision has stopped after publication of the circular 12, which sets conditions forprovision of safety and quality of immunization. This has resulted in suspension of outreach services inalmost all parts of the country, which has important implications on equity in immunization serviceprovision, as many of the most disadvantaged and poor families reside in remote areas. Flexibility ininterpretation of Circular 12 was highly recommended by the National EPI review11 in order to ensure thatremote area residents in particular have adequate access to mobile or outreach service strategy.Equity Strategy for Routine ImmunizationViet Nam immunization program ensured high coverage rates, however reaching the most disadvantagedpopulation still remains the most significant challenge for EPI. Existence of following different types of11National EPI Review, 20159
disadvantaged population groups who are most at risk of not accessing immunization services suggestsabout the equity problems in the national immunization program of Viet Nam 12:-Migrant populations who move to Provinces or Cities and who may not be registered with localauthorities-Mobile populations who come and go from their place of residence on a periodic basis in search ofemployment in other locations-Remote Area residents cut off from health services by seasonal flooding due to poor road access-Ethnic minority populations who may not always understand Vietnamese language andimmunization messagesReaching these at risk population groups requires flexible interpretation of Circular 12 to ensure mobile oroutreach services to the communities. It also means careful implementation of coverage monitoring,micro-planning to reach every community, tracking of drop outs and securing of operational financing tosupport targeted mobile/outreach strategy implementation.Urban EPI StrategyTracking populations is a major issue in the urban setting, given the high rate of internal migration andmobility of the population. In the most cases, the temporary residence place for internal migrants is notnecessarily the place where they try to access immunization services. The coverage data is furthercomplicated by the high level of immunizations provided through the non-EPI service provision model.Given the very large population base, operation finances are critical in order to provide the adequateimmunization sessions. Financial commitments of local governments varies significantly that raiseslegitimate questions regarding standards for operational financing in urban context.In terms of Circular 12, the limitation on the size of sessions to 50 persons per session is challenging in theurban context where population density is higher and immunization sessions are necessarily larger.Finally, waste management is far more challenging in an urban context, where the volume of waste ishigher and the areas for disposal are more limited. All of these issues are likely to become morechallenging as these cities continue to expand in the next 5 to 10 years that would require development ofa specific Urban EPI strategy for the next cycle in order to address these challenging policy andoperational issues.Hepatitis B Birth Dose and MCV2 DTP4Although there remain many obstacles to achieving timely and high coverage for hepatitis B birth dose,there has been significant improvement when compared to the 2009.9 Hospitals have functional coldchain and vaccine management systems, and are reporting data regularly to provincial and DistrictPreventive Medicine Centers. There is reasonably high coverage in the hospital settings, andcontraindications for immunization with hepatitis B birth dose are documented according to the MoHguidelines. In remote areas, absence of mobile/outreach strategy (due to lack of operational financingand adequate human resources) means that for those who still deliver at home, a timely hepatitis B birthdose is not possible in some circumstances. In some locations, hesitancy to vaccinate from clinicians and12National EPI Review, Vietnam, August 201510
families is still evident due to fear of AEFI. Given that nationwide delivery at facility is 92%, there remainmany opportunities for the improvement in coverage through communication strategy with families andclinicians. MCV2 and DTP4 coverage is high in some provinces, while in others there remains significantdrop out from the previous doses, highlighting the importance of coverage monitoring and drop outtracing, and local area communication strategy to support completion of the vaccination according to theexisting schedule.Service IntegrationIn terms of EPI service delivery strategy, most immunizations are provided at facilities, which means thatby definition the services are integrated into the PHC services. There was little evidence however that EPIwas integrated with other services during outreach and/or mobile health strategy. Program finances andguidance is managed vertically, so there remains limited policy guidance on this issue. Given the scope ofthe issue (PHC), it would seem that improved service integration for outreach or mobile strategy wouldrequire appropriate health sector policy and guidance.1.2.2 COVERAGE AND REPORTING OF VACCINE PREVENTABLE DISEASESHigh coverage has been maintained by most antigens for the last 10 years with a number of exceptions.There was a sharp drop in immunization coverage for DTP3 in 2013, related to a nationwide suspension ofpentavalent vaccine following an AEFI. The other notable observation is the hepatitis B birth dosecoverage, which is lower than expected given the high facility delivery rate in Viet Nam (92%). Althoughthe coverage has recovered from the decline during the previous planning cycle, recent AEFI events mayhave also contributed to the moderate coverage levels.Error! Reference source not found.Despite the overall high coverage, a plan recently developed inAXIS TITLEDPT3DPT1Hepb Birth Dose10090807060504030201002014 2013 2012 2011 2010 2009 2008 2007 2006 2005 2004 2003 2002 2001 2000Viet Nam to strengthen immunization services has pinpointed the areas of the country with immunizationcoverage lower than 80%.As part of this planning, an analysis of rural districts with 80% coverage for DTP-HepB-Hib3 or MCV2in 2014 identified 91 districts in the country distributed in 26 provinces: 12 districts are in the north, 4 incentral regions and 10 in the south. A total of 68 out of the 91 districts reported measles cases in 2014,with a range from 1 case to 179 cases per district.11
This issue of inequities in health outcomes has been confirmed by publication of infant mortality rates byregion, which has found that the highest rates are in the two poorest regions, the Central Highlands andthe Northern midlands and mountain areas.13 Ethnic minority groups, which constitute 14% of thenational population, have significantly poorer health and socio economic status than the majority ethnicgroup.14In 2014 Viet Nam faced measles outbreak. An analysis of the outbreak revealed that, since the beginningof 2014, more than 86% of those infected were not immunized or their vaccination status was unknown. 15Also of note was the occurrence in April-May 2012 of two isolated cases of Circulating Vaccine-derivedPoliovirus type II (cVDPV2) detected in two provinces in the Southern region, although there have beenno reports of cVDPV since then.Table 3 documents the reported cases of vaccine preventable diseases between 2010 and 2014: themeasles outbreak in 2014 (final case number over 15,000, with incidence of 71/ 1 million), 16 rubellaoutbreak in 2011, and the persistence of reported JE cases (n 450 in 2014) despite the scale up of theimmunization program to 80% of the target population.Table 3. Disease Prevention and 2136Japanese 7'2592'300Rubella (CRS)1392189Tetanus (neonatal)3446393235Tetanus (total)244306253186196A downward trend in vaccine preventable diseases were confirmed by number of studies andpublications17 that confirms potential for new vaccines to contribute further to mortality and morbiditydecline.Acute respiratory infections are the leading cause of hospital admission and childhood mortality. Themost common causative agents in children have been found to be S. pneumonia, accounting forapproximately 30 to 50 percent of cases, and H. influenza B (Hib) causing from 10 to 30 percent of cases.Similarly, the most common causative agents of meningitis have proven to be Hib, N. meningitidis and S.13MOH Joint Annual Health Sector Review 2014UNFPA Ethnic Groups in Viet Nam: An analysis of key indicators from the 2009 Viet Nam Population and Housing Census,UNFPA, 2011, Hanoi, Viet Nam15WHO Measles control in Vietnam April atures/measles control vietnam 2014/en/16WHO Manila Measles Rubella Bulletin Volume 9 Issue 6 June 201517A Joint Annual Health Sector Review1412
pneumonia. According to health statistics in Viet Nam, the main causative agent of acute diarrhoea thatrequires hospital admissions is rotavirus.18 Although 11 vaccines for routine immunization are ava
4 1. Situational Analysis 1.1. COUNTRY PROFILE Viet Nam (population 91.6 million) in recent years has experienced steady rates of economic growth and social development.