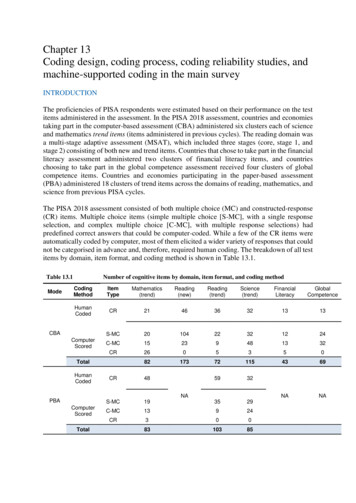
Transcription
AdvancedCoding Principlesfor theAllergy PracticePresented byTeresa Thompson, CPC, CMSCS, CCCTM Consulting, Inc.Carlsborg, WATeresathom@aol.comLearning Objectives Describe details of coding forpatients’ allergy testing andimmunotherapy Discuss the use of codespertinent to A/I practice
Improving Your Bottom Line Coding conservatively – is it anissue? Co-pays – are they collected Fees that are not current – review Diagnosis not appropriate toencounter Not coding all services – hospitalconsults, subsequent care,procedures Timeliness of submission3Improving Your Bottom Line New providers and no provider #– Only 30 days to prior to NPI with CMS Scheduling of patients – charging forn/s? Staff overload – overtime? Lack of research for best price - antigens New procedures and equipment notrecognized as payable by carriers– 95012- Nitric oxide expired gasdetermination4
Fee Schedules Read your contracts thoroughlybefore signing Know your reimbursement rates Ask if the carrier follows CMSguidelines– What about mid level providers? What bundling program is used –are they available on the carrierwebsite Preventive a covered benefit?5Fee Schedules What is the “legal” payment time foryour state Does the carrier change yourcodes? When should you contact yourinsurance commissioner or medicalsociety? What is proper for appealingclaims?6
Maximizing for a Greater Profit Review, posting & processing of EOB topatient account –payment correct Following guidelines published percarrier Regular auditing & monitoring of allphases Are all charges being collected What is percentage of uncollectedcharges Continual education and training of allstaffResults? Profitable practice Patient satisfaction Staff accountability, pride andsupport
Claims Submission What is covered and what is noncovered? What is legal payment time forcarrier? Down coding – is it happening?Claims Submission Appeals – What is the appropriateprocedure for your major insurancecompanies? What is required? Telephone orpaper appeal?
Claims Submission What is your basis for appealing? Are the modifiers beingrecognized? Contract policies – do you have acopy?DOCUMENTATIONANDTOOLS
Documentation Translate medical record into codes– ICD-9 codes and CPT codes Electronic health record versuspaper chartMost Common Errors Diagnoses do not matchdocumentation Physician codes rule out possible,probable, as definitive diagnosis Co-morbidities are coded with nodocumentation in note to supportcoding Lack of specificity in documentationand coding
CPT ModifiersE/M Modifiers 25 -- Significant, separatelyidentifiable E/M service by thesame physician on the same day ofthe procedure or other service
25 Modifier Tips Chief complaint must be appropriatelydocumented to support an E/M plusallergy test, PFT or shots By CPT and CMS guidelines, 25modifier is required for E/M, allergytesting, allergy injection and/orpulmonary function test performed onthe same day.26 Professional Component The interpretation component ofa code which has both aprofessional and technicalcomponent Example – PFT read in hospital 26 is the professional componentonly
59 Distinct Procedure Example:– 94060 with 94664 Included in the pre and post when theinstruction is done to teach patienthow to use MDI to accomplish the preand post 9466459 when the instruction is donefor the patient’s knowledge to use adevice after the encounter76 Repeat Procedure BySame Physician Example: 94640 9464076 When more than one nebulizertreatment is administer to a patienton one day
HCPCS MODIFIERS GAWaiver of liability on file GYNon-covered service byMedicareAllergy Procedures and Services22
Aerosol Demo/Eval pt utilizBronchodilation responsivenessBronchospasm Eval - ProlongedLaryngoscopy - flexible, dxNasal endoscopyNasopharyngoscopyNon pressured Inhalation trmt less than 1 hourContinuous inhalation tx with RX 1hrContinuous inhalation tx with Rx ea addt'l 1hrOximetry, singleOximetry, multiplePulmonary Stress Test, SimpleRespiratory Flow Volume LoopSpirometry, baseVital Capacity, total (separate P.)Nitric oxide expired gas 6449464594760947619462094375940109415095012Allergy Testing and ordering of immunotherapy needsto be done based on orders from the physician Testing is either percutaneous, intradermal perantigen, or intradermal sequential &incremental Not all carriers recognize testing code 95027 RAST testing may be performed – check forcoverage per patient Interpretation and report included in code fortest Interpretation & report by physician is part oftest
ALLERGY TESTINGPuncture/Prick allergenic extract #95004Intradermals allergenic extract #95024Allergy test Prick and ID - venoms #Allergy test Prick & ID biologicals & drugs#95017Skin end point titration95027Delayed ID testing #95028Patch Test #95044Inhalation bronchial challenge95070with antigensIngestion challenge test initial 120 minutesIngestion challenge test: ea additional 60min95018950719507695079ALLERGEN IMMUNOTHERAPYAllergen-Mult. Dose # Doses95165Allergen - Single Dose #95144Venom Antigen - 1 single stinging95145Venom Antigen - 2 single stinging95146Venom Antigen - 3 single stinging95147Venom Antigen - 4 single stinging95148Venom Antigen - 5 single stinging95149Whole Body - biting insect95170Rapid Desensitization #Hr95180
Allergy Immunotherapy Watch!!! Third party payers implementing thedefinition of a dose the same asMedicare Third party payers not allowing “offthe board treatment” Limits on the number of dosesallowed per the carrier guidelines peryear or per date SLIT – Correct code is 95199Allergy 95165 – two definitions– Medicare – per cc of theconcentrated solution– CPT – A dose is the amount ofantigen(s) administered in a singleinjection from a multiple dose vial– Check coverage for patient’s – maybe pharmaceutical benefit ratherthan a professional benefit
Immunotherapy 95170Whole body biting insect fire ants 95180Rapid desensitization Charge by time – time must be documented Only time of desensitization test, not time inoffice Doses given for desensitization may also becharged95165 Examples Patient is beginning immunotherapyfor trees and molds. Because ofpatient’s sensitivity, patient’santigens are separated. Patient hasfour vials of both the molds andtrees. There are ten medical dosesin each of the vials. The vials are 5cc vials
95165 Coding CPT coding would be 95165 with ?units CMS coding would be 95165 for ?units since the build up vials are notbillable to CMS The anticipated number of units thepatient will get determines the unitsfor the dilution vials95165 – Maintenance Vials Pt needs a refill for both trees andmolds. The vials are 5 cc vials andthe patient is on .5 cc for a dose. CPT coding – 95165? units CMS coding – 95165? units The CMS coding would be 10 unitssince there are 2 vials of 5 ml each
Venom Immunotherapy The code that is used isdetermined by the sum of allvenoms that will be provided at asingle visit If a patient gets honey bee andmixed vespid, the code would be95148 for 4 venoms Patient has mixed honey andwasp ?Immunotherapy 95170Whole body biting insect fire ants 95180Rapid desensitization Charge by time – time must be documented Only time of desensitization test, not time inoffice Doses given for desensitization may also becharged
INJECTIONSAllergy Injection - 195115Allergy Injections - 2 95117Allergy Inj Antigen95120Allergy Inj Antigen 2 Xolair Injection951259637296401OTHER INJECTIONSAntibiotic Inj ( )96372Immun. admin. Single with counseling 9046090471Immuno admin, ea add'l. with counseling 9056 90472Flu Vac under 3yr pre free90655Flu Vac under 3yr90657Flu Vac 3yr , split virus V04.81 – V06.690658Flu Vac intranasal90660IV Med Admin push96374Infusion Therapy 1st hr9636596366ea. add'tl hr.PneumovaxV03.82 – V06.690732Therapeutic Inj963723535SUPPLIES/ MISCELLANEOUSLab Handling99000Nasal Smears89190SolumedrolJ2930SyringesA4206Special Reports99080TriamcinoloneJ3301XolairJ2357Portable peak flow meter(A4614)S8096Peak flow expir. flow physicianserviceS8110Nebulizer & suppliesA7003throughA701736
Asthma Education S Code for BC/BS and HealthInsurance Association of America S9441 – asthma education nonphysician provider per session 98960 – education – for nonphysician per patient – notspecific to asthma Requires standardizedcurriculumPeak Flow Reading For Medicare/Medicaid it isincluded in the E/M S code for third party payers S8110 – Peak expiratory flowrate (physician services)
Chart Auditing What do you when a letter arrivesasking for multiple chart notes? Who is your lead for release ofrecords? Do you know your risk? Monitoring your most frequent codesis maintaining a healthy practice How often do you run a utilization foryour practice?Chart Auditing EHR and incentives need to bemonitored Watch “canned” statements andrepetitions Have an outside “look” forcompliance Know the key componentsrequired to support your coding
Allergist Coding CurveNational 99201 99202 99203 99204 99205.47 %5.00 %30.15%51.32%National99241992429924399244.52 %3.48 %30.42%54.02%13.06%9924511.56%41Allergist Coding CurveNational 99211 99212 99213 99214 992153.98 %6.77%55.25%31.09%2.91 %42
Components of Evaluationand Management CodesComponents of the E & M HistoryExamMedical Decision MakingTime is ONLY important whenmore than 50% of the encounteris counseling and coordination ofcare
Requirement for New/ConsultPatient vs. Established Patient History, Exam & Medical DecisionMaking need to be at the same levelor higher to support the level of care Two of the three of the componentsat the same level or higher tosupport the level of care The history and exam must beappropriate to the patient’spresenting -3 of 3992419924299243992449925599245NEW PT- 3 of 39920199202992039920499205CHIEF X of PRESENT ILLBrief(1-3)Brief(1-3)Extended(4 )Extended(4 )Extended(4 REVIEW OFProblemExtendedCompleteCompleteSYSTEMSPertinent (1)HISTORY(2-9 System)(10 system)(10 system)PAST HXPertinent-1Complete-1eaComplete-1eaFAMILY HXPertinent-1Complete-1eaComplete-1eaSOCIAL mentdocumentdocument1 organ 2-45-78 organ8 organsystemOrgan systemssystemssystemsorgansMED. DEC MAKING(2 of the 3 must be met or exceeded)MGMT OPT. & DX.Minimal (1)Minimal (1)Limited (2)Multiple (3)Extensive(4)AMT DATA &COMPLEXMinimal(1)Minimal (1)Limited (2)Moderate (3)Extensive(4)RISK OF COMPLICAT.MinimalMinimalLowModerateHigh
ESTABLISH PT2 OF RequiredRequiredBriefBriefExtendedExtendedProb. PertinentExtendedCompletePAST HISTORYPertinent-1Complete:FAMILY HISTORYPertinent-1Choice of 2SOCIAL HISTORYPertinent-1ele PFS Hx.HISTORYCHIEF COMPLAINTHX PRESENT ILL.SYSTEM documentdocumentdocument2-4 organ sys5-7 organsystem8 organ systems1organMED. DEC MAKINGMGMT/OPTION DXMinimal (1)Limited (2)Multiple (3)Extensive(4)AMT ve(4)RISK OF COMPLICAT.MinimalLowModerateHighHistory Audit Sheet HPI: Chief Complaint –Reason forencounter– Location – specific to area of the body– Quality – describe the pain – dull sharp; woundjagged, dirty or clean– Severity – measure on a scale– Duration- how long, since when, etc– Context- how complaint occurred– Modifying factor- what has alleviated symptoms– Signs and symptoms – additional information frompatient
History Audit Sheet Review of Systems:– Ten are required for a complete ROS– Pertinent positives and negatives must bedocumented– A notation of negative for the remainingreview of systems may be documented forthe remaining systems– Can be documented by staff patient– Must be reviewed by physician– Can be separate or part of the HPI– Cannot use one statement in bothcategoriesHistory Audit Sheet Past, Family and Social History:– Past – Events in the patient’s pastmedical/surgery history– Family – Diseases that impactpatient’s health– Social - Factors which are ageappropriate that impact from anenvironmental and social pattern
Exam Audit Sheet The 1995 guidelines or the 1997guidelines can be used fordocumentation Allergy has a specific exam forthe specialty Abnormal findings must bedescribed Normal findings can be indicatedby negative
1995 Exam Components Problem focused: one organsystem Expanded problem focused: twoor more organ systems (2-4) Detailed: two or more withdetailed information (5-7) Comprehensive: eight or moreorgan systemsMedical Decision Making Number of diagnosis andtreatment options Amount of data and complexity ofdata Risk
Number of Diagnosis &Treatment Options New problemEstablished problem stableEstablished problem worseningEstablished problem, improvedWorkup plannedNo workup plannedAmount & Complexityof Data Review/order lab testsReview/order routine x-raysReview/order medicine testsDiscussion of tests results withperforming physician Decision to obtain old records &document Direct visualization & independentinterpretation documented
Risk Presenting problem Diagnostic procedure Management optionsPresenting Problem Minimal:– One self limited or minor problem Low:– Two or more self-limited or minorproblems– One stable chronic illness– Acute uncomplicated illness/injury
Presenting problem, con’t Moderate:– One or more chronic illness with mildexacerbation– Two or more stable chronic illnesses– Undiagnosed new problem withuncertain prognosis– Acute illness with systemicsymptoms– Acute complicated injuryPresenting Problem, con’t High:– Chronic illness with severeexacerbation– Acute or chronic illness/injury thatmay pose a threat to life or bodilyfunction
Diagnostic ProceduresOrdered Minimal:– Lab tests requiring veni-puncture– X-rays– Ultrasounds Low:– Superficial needle biopsies– Skin biopsies– Pulmonary function testsDiagnostic Procedures, con’t Moderate:– Diagnostic endoscopy– Deep needle or incisional biopsy High:Diagnostic endoscopy with riskfactors
Management Options Minimal:– Rest– Gargles– Elastic/superficial dressings Low:– Over the counter drugs – salinewashes– Minor surgery – ear piercing– Physical TherapyManagement Options, con’t Moderate:– Minor surgery with risk– Elective major surgery– Prescription drug management– Closed treatment of fracture w/omanipulation
Management Options, con’t High:– Elective major surgery with risk– Emergency major surgery– Decision not to resuscitate or deescalate care because of poorprognosis– Drug therapy requiring intensivemonitoring for toxicity.– High morbidity mortality withouttreatment
What About Time? Time is only used if more than 50%of the encounter is counseling andco-ordination of care. You mustdocument:1. Total face to face time2. The amount which wascounseling3. The counseling and coordinationof care discussionCase #1 - History CC: Rash. Pt has experiencedsymptoms since 6 months of age.She has had frequent rashes onher trunk and extremities. Herskin gets dry with red patches.Rash is perennial, no seasonalchanges so far. She has haddistatin and topical Benadryl.
Case # 1 - History Past history – birth wt 6 lbs,neonatal jaundice Medication allergies: NKDA Family hx: Hay fever, migraine –mother ROS: Constipation and bloating.All remaining 14 systems arenegativeCase #1 - Exam Gen: ht 35 1/2 “, Wt- 24#, Pulse118, RR 24 WN – thin Skin – normalNose - normal Head – normalMouth - normal Eyes – normalNeck - normal Ears – normalResp - normal Ears – normalHeart – normal Extrem – normal Neuro - normal
Case #1 – A/P Lab data – negative CBC & IG Prick testing for peanut, egg,cows milk, wheat, walnut, fish,soy shrimp and corn are negative Inhalants are negative for treesand grassesCase #1 A-P Chronic atopic dermatitis, in remissiontoday Role for IgE-mediated food allergyappears unlikely, food intoleranceremains possible Rec: Daily hydration followed byCerave cream. Limited use ofhydrocortisone cream. No dietaryrestrictions for now. Be observant forsigns of food intolerances.
Case #2 CC: watery eyes, nasal congestionchronic. Pt has had increasingrhinoconjunctivitis symptoms over thepast year. She was tested for allergywhen she was living in another statemany years ago and found to beallergic to dust mite and animal dander.She is concerned about allergies as atrigger for her symptoms. She also hasa history of asthma.Case #2 Past medical history – negative Family history – brothers have hayfever and asthma Social history – not a smoker,enjoys outdoor activities and has adog for a pet ROS – GI, Endocrine, Resp arepositive the remaining 14 systemsare negative
Case #2 Gen – BP 118/70, Ht 5’10”, Wt 150,Pulse 82, RR 12, healthy in NAD Skin – normalHead – normal Eyes – normalEars – normal Nose – pale boggy mucosa, edema ofturbinates, discharge watery clear, nopolyps Mouth – normalNeck – normal Resp – normalHeart – normal Abd – normalExtrem – normal Neuro – normalA/P Seasonal and perennial allergicrhinoconjunctivitis that has worsenedover the past year Mild persistent asthma with allergictrigger Rec: nasal irrigations Environmental controls Decongestants with antihistamine Nasal spray, RX for eyedrops,allergy immunotherapyrecommended, Rx for asthma
Case #3 CC: evaluation of allergies – R/OVCD vs asthma, cough - reviewmeds. Cough is worse at nightbut not waking up. Vomiting, thickmucus associated with cough.Headache over the past 3-4days. Sinus pressure for threedays also. No change in environmental hx,ROS not updated.Case #3 Exam:General – normal Skin – normalSinus tender both left and rightEyes – normalLungs - normalEars – normalHeart - normalNose – septum normal, mucuswatery and clear with edema Oropharynx – normal Neck - normal
Case #3 A/P Dx: Seasonal, perennial allergicrhinitis which is worse; asthmawhich is not well controlled –cough, PND RX – trial of bronchodilator,consider CT if cough persist,check for GERD Questions? Thank you for coming80
Aerosol Demo/Eval pt utiliz 94664 Bronchodilation responsiveness 94060 Bronchospasm Eval - Prolonged 94070 Laryngoscopy - flexible, dx 31575 Nasal endoscopy 31231