Transcription
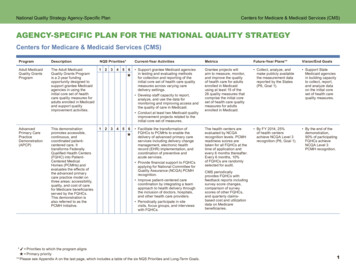
National Quality Strategy Agency-Specific PlanCenters for Medicare & Medicaid Services (CMS)AGENCY-SPECIFIC PLAN FOR THE NATIONAL QUALITY STRATEGYCenters for Medicare & Medicaid Services (CMS)ProgramDescriptionNQS Priorities*Adult MedicaidQuality GrantsProgramThe Adult MedicaidQuality Grants Programis a 2-year fundingopportunity designed tosupport grantee Medicaidagencies in using theinitial core set of healthcare quality measures foradults enrolled in Medicaidand support qualityimprovement activities.12345AdvancedPrimary CarePracticeDemonstration(APCP)This demonstrationpromotes accessible,continuous, andcoordinated patientcentered care. Ittransforms FederallyQualified Health Centers(FQHC) into PatientCentered MedicalHomes (PCMHs) andevaluates the effects ofthe advanced primarycare practice model onthree areas: accessibility,quality, and cost of carefor Medicare beneficiariesserved by the FQHCs.This demonstration isalso referred to as thePCMH Initiative.12345Current-Year ActivitiesMetricsFuture-Year Plans**Vision/End Goals6 Support grantee Medicaid agenciesin testing and evaluating methodsfor collection and reporting of theinitial core set of health care qualitymeasures across varying caredelivery settings. Develop staff capacity to report,analyze, and use the data formonitoring and improving access andthe quality of care in Medicaid. Conduct at least two Medicaid qualityimprovement projects related to theinitial core set of measures.Grantee projects willaim to measure, monitor,and improve the qualityof health care for adultsenrolled in Medicaidusing at least 15 of the26 quality measures thatcomprise the initial coreset of health care qualitymeasures for adultsenrolled in Medicaid. Collect, analyze, andmake publicly availablethe measurement datareported by the States(P6, Goal 1). Support StateMedicaid agenciesin building capacityto collect, report,and analyze dataon the initial coreset of health carequality measures.6 Facilitate the transformation ofFQHCs to PCMHs to enable thedelivery of advanced primary careservices including delivery changemanagement, electronic healthrecord (EHR) implementation, andcoordination of preventive andacute services.The health centers areevaluated by NCQArecognition levels. PCMHreadiness scores aretaken for all FQHCs at thetime of application andevery 6 months thereafter.Every 6 months, 10%of FQHCs are randomlyselected for audit. By FY 2014, 25%of health centersachieve NCQA Level 3recognition (P6, Goal 1). By the end of thedemonstration,90% of participatingFQHCs achieveNCQA Level 3PCMH recognition. Provide financial support to FQHCsapplying for National Committee forQuality Assurance (NCQA) PCMHrecognition. Improve patient-centered carecoordination by integrating a teamapproach to health delivery throughthe inclusion of doctors, hospitals,and other health care providers. Periodically participate in sitevisits, focus groups, and interviewswith FQHCs.* Priorities to which the program aligns Primary priority** Please see Appendix A on the last page, which includes a table of the six NQS Priorities and Long-Term Goals.CMS periodicallyprovides FQHCs withfeedback reports includingsurvey score changes,comparison of surveyscores of other FQHCs,and quarterly claimsbased cost and utilizationdata on Medicarebeneficiaries.1
National Quality Strategy Agency-Specific PlanCenters for Medicare & Medicaid Services (CMS)Centers for Medicare & Medicaid Services (CMS) (Continued)ProgramDescriptionNQS Priorities*BundledPaymentsfor CareImprovement(BPCI)BPCI links paymentsfor the multiple servicespatients receive during anepisode of care to improvecare coordination andquality. This combinationof payments createsa greater incentive todecrease unnecessaryduplication of services,reduce preventablemedical errors, increasepatient safety, andlower costs.1Children’s HealthInsurance ProgramReauthorization Act of2009 (CHIPRA) QualityDemonstrations are a5-year grant program withcumulative grant awardstotaling 100 million.Eighteen States across10 grants participate inmulticomponent projectsaimed at improving healthcare quality and deliverysystems for childrenenrolled in the Medicaidand the Children’s HealthInsurance Program (CHIP).1CHIPRA QualityDemonstrations2233445566Current-Year ActivitiesMetricsFuture-Year Plans**Vision/End Goals Support BPCI participants inimplementing the following threetypes of bundled payment models:–– Model 2: Retrospective Acute CareHospital Stay plus Post-Acute Care–– Model 3: Retrospective Post-AcuteCare Only–– Model 4: Acute Care HospitalStay Only The models use either retrospectivepayment bundling, in which CMS andproviders set a target payment amountfor a defined episode of care, orprospective payment bundling in whichCMS makes a single, prospectivelydetermined bundled payment. Provide assistance to providers inorder to select health conditionsto bundle, develop the health caredelivery structure, and determine howpayments will be allocated amongparticipating providers. Conduct Webinars and learningsessions to share findings on theprivate sector’s involvement withepisode-based payments andcare redesign.BPCI compares the totalpayment amount of adefined episode of carewith the target price set byCMS and providers. CMSmonitors clinical quality,patient experience, andoutcomes of care. Further coordinationamong health careproviders through thebundling of payments forsingle episodes of care(P3, Goal 1). Improve care transitionsto decrease numberof readmissions andlower health care costs(P6, Goal 1). Replacefragmented carewith coordinatedcare amongdoctors, hospitals,and other healthcare providers. Lower health carecosts throughimproved carecoordination. Experiment with and evaluate theuse of the initial core set of children’shealth care quality measures forMedicaid and CHIP. Promote the use of health informationtechnology in the delivery of carefor children. Implement provider-based modelsthat improve the delivery of Medicaid/CHIP children’s health care services. Demonstrate the impact of the modelchildren’s electronic health recordformat (two grantees are participatingin this activity).Each demonstration hasidentified its own set ofmeasureable objectivesand outcomes. Continue to identify bestpractices for improvingchildren’s health care(P6, Goal 1). Improve children’shealth care qualitythrough the useof health qualitymeasures, healthinformationtechnology, andprovider-baseddelivery models.* Priorities to which the program aligns Primary priority** Please see Appendix A on the last page, which includes a table of the six NQS Priorities and Long-Term Goals.Models 2–4 use astandardized set ofmeasures established byCMS. Additional measuresfor all models can beproposed by applicants.(Model 1 implementationis currently suspendedand under review.)2
National Quality Strategy Agency-Specific PlanCenters for Medicare & Medicaid Services (CMS)Centers for Medicare & Medicaid Services (CMS) (Continued)ProgramDescriptionNQS Priorities*Communitybased CareTransitionsProgram (CCTP)This program is part ofPartnerships for Patients.CCTP tests models forimproving care transitionsfrom the hospital to othersettings and for reducingreadmissions for high-riskMedicare beneficiaries.1234512345Current-Year ActivitiesMetricsFuture-Year Plans**Vision/End Goals6 Select and award 2-year agreementsto pay CBOs an all-inclusive rate pereligible discharge based on the costof care-transition services provided atthe patient level and implementationof hospital-level systemic changes. Provide funding for testing modelsthat improve care transitions bytargeting specific populations andproviding strategies for identifyinghigh-risk patients.CMS evaluates andtracks each CBO’stargeted performancethresholds on qualityand utilization measuressuch as 30-day all-causereadmission rates, 90and 180-day readmissionrates, mortality rates,observation services,and emergencydepartment visits. Provide assistance toCBOs to incorporatecare-transitioninterventions andservices to addressreadmissions(P3, Goal 1). Aid CBOs inimproving providercommunications andpatient engagement(P3, Goal 1). Document measurablesavings to the Medicareprogram from CCTP(P6, Goal 1). Preserve orenhance quality ofcare for Medicarebeneficiarieswhile providingcare-transitioninterventionsacross settings. Help achievePartnership forPatient goals: (1)reduce preventableerrors in hospitalsby 40%, and (2)reduce hospitalreadmissionsby 20%.6 Provide support for 500 primarycare practices to test payment anddelivery models. Convene CMS and participatingpayers to share utilization and costdata with providers. Coordinate with commercial andState health insurance plans to offeradditional non-visit payment to primarycare doctors and nurses to bettercoordinate care for their patients. Promote a market-based communitythrough three annual meetings,monthly Web-based meetings, anddissemination of materials. Share best practices for health andhealth care quality improvements atthe local, State, and Federal levels.CPCI measures programimplementation throughnine primary care practicemilestones determinedby CMS for the first year,including risk status,access to medical records,and meeting attendance.Due to the diversity ofpractice sites, the specificmetrics are decided byeach practice to illustratecare improvement. Help patientscreate a plan ofcare incorporatingindividual health risks,circumstances, andvalues (P2, Goal 2). Improve the valueproposition ofprimary care to lowerhealth system costs(P6, Goal 1). Provide market-basedlearning opportunitiesto share best practices(P3, Goal 3). Include practicesin Shared Savingsprogram in years 2–4(P6, Goal 1). Establish a newnational model tocoordinate care,improve health, andlower costs for allAmericans. Invest in primarycare practicesthroughoutcommunitiesto help smallbusinesses,patients, andtaxpayers use theirhealth care dollarsmore wisely.Community-basedorganizations (CBOs) willbe paid for care transitionservices.ComprehensivePrimary CareInitiative (CPCI)This multipayer 4-yearinitiative fosterscollaboration betweenpublic and private healthcare payers to strengthenprimary care throughthe testing of health carepayment and deliverymodels. This programprovides participatingpractices with resourcesto (1) manage carefor patients with highhealth care needs,(2) ensure access to care,(3) deliver preventivecare, (4) engage patientsand caregivers, and(5) coordinate care acrossthe medical neighborhood.* Priorities to which the program aligns Primary priority** Please see Appendix A on the last page, which includes a table of the six NQS Priorities and Long-Term Goals.3
National Quality Strategy Agency-Specific PlanCenters for Medicare & Medicaid Services (CMS)Centers for Medicare & Medicaid Services (CMS) (Continued)ProgramDescriptionNQS ramThe HVBP Programimplements a pay-forperformance approachto health care paymentby rewarding hospitalsfor the quality of carethey provide to Medicarepatients, rather than thequantity of proceduresthey perform. This programattempts to transform thequality of hospital careby realigning hospitals’financial incentives.123456Current-Year ActivitiesMetricsFuture-Year Plans**Vision/End Goals Conduct national provider calls andWebinars for hospitals and otherstakeholders to discuss summaries ofactivity, developments in the program,and provide previews of the program’sfuture plans. Encourage care quality improvementand use of best clinical practicesthrough restructured incentives.Hospitals receiveincentive payments basedon their performanceacross 12 clinical processof-care measures and8 patient experienceof-care measures or onthe improvement of theirperformance relative to abaseline performance. In FY 2014, incentiveswill expand performancemeasurement toinclude an additionalclinical process of caremeasure and threeoutcome measures(P6, Goal 1). Transform healthcare in hospitals byimproving patients’experience of careand following bestclinical practices.* Priorities to which the program aligns Primary priority** Please see Appendix A on the last page, which includes a table of the six NQS Priorities and Long-Term Goals.4
National Quality Strategy Agency-Specific PlanCenters for Medicare & Medicaid Services (CMS)Centers for Medicare & Medicaid Services (CMS) (Continued)ProgramDescriptionNQS Priorities*Medicareand MedicaidElectronicHealth Records(EHR) IncentiveProgramThis program providesincentive payments toeligible professionals(EPs), eligible hospitals,and critical accesshospitals (CAHs) as theymeet a set of criteria forthe use of Certified EHRtechnology within theMedicare and Medicaidprograms. Certified EHRsshould be used (1) in ameaningful manner, (2) forelectronic exchangeof health informationto improve quality ofhealth care, and (3) tosubmit clinical qualitymeasures (CQMs) andother such measuresselected by the Secretary.CMS implements thisprogram through theconstructs of meaningfuluse and clinical qualitymeasurement.123456Current-Year ActivitiesMetricsFuture-Year Plans**Vision/End Goals Support providers in reporting clinicalquality measures, overall health ITtransition, and the implementation ofCertified EHR technology. Capture electronic health informationin a standardized format and useit to track key clinical conditions,enable clinical decision support,facilitate electronic health informationexchange in care coordinationprocesses, and engage patients andtheir families in their care. Provide patients with timely electronicaccess to their health information.In 2013, EPs must reporton six total clinical qualitymeasures. Eligiblehospitals and CAHs mustreport on all 15 clinicalquality measures. Implement morerigorous healthinformation exchanges(HIEs) to increasepatient access tocomprehensive data(P3, Goal 1). Increase electronictransmission of patientcare summaries acrossmultiple settings(P3, Goal 1). Require providers tobe responsible forpromoting patientengagement with onlinehealth information (5%of patients must accesstheir health information)(P3, Goal 3). Align clinical qualitymeasures acrossquality reportingprograms to reduce theburden on providersand emphasize NQSpriorities (P3, Goal 1). Utilize clinical qualitymeasure data to informpolicy decisions, clinicalprocesses, and clinicaldecision support tocontinuously improvethe quality of care(P3, Goal 1). Promote the spreadof EHRs to improvehealth care andreduce costs. Use EHRs toincrease patientaccess to selfmanagement tools. Use EHRs toachieve theNQS qualityimprovement goalsand priorities.* Priorities to which the program aligns Primary priority** Please see Appendix A on the last page, which includes a table of the six NQS Priorities and Long-Term Goals.In 2013, EPs arerequired to meet 15 coreobjectives ranging fromE-Prescribing (eRx) toclinical summaries ofpatients’ office visits.They are also required toreport on 5 out of the 10menu objectives whichrange from summary ofcare record for transitionsof care to reminders forpatients’ preventive/followup care, includingone public health-relatedobjective.In 2013, eligible hospitalsand CAHs are required tomeet 14 core meaningfuluse objectives and 5 out ofthe 10 menu objectives.5
National Quality Strategy Agency-Specific PlanCenters for Medicare & Medicaid Services (CMS)Centers for Medicare & Medicaid Services (CMS) (Continued)ProgramDescriptionNQS Priorities*MedicareShared SavingsProgramThe Medicare SharedSavings programprovides incentives forbetter coordination andcooperation amongproviders and with theirpatients to improvebeneficiary outcomesand increase valueof health care by (1)promoting accountabilityfor the care of Medicarefee-for-service (FFS)beneficiaries, (2) requiringcoordinated care for allservices provided underMedicare FFS, and (3)encouraging investmentin infrastructure andredesigned careprocesses. Participatingproviders receive aportion of the savings ifthey successfully achievequality standards andlower growth in healthcare costs.123456Current-Year ActivitiesMetricsFuture-Year Plans**Vision/End Goals Currently oversee the 114Accountable Care Organizations(ACOs) participants in the MedicareShared Savings Program and 32additional ACO participants in thePioneer ACO initiative. Enact annual application processto bring additional ACOs online inJanuary each year. Provide support to ACOs in identifyinggaps in care and opportunities forbetter coordination and qualityimprovement, and redesigning careprocesses through feedback reportsand claims data. Assist ACOs with understandingprogram requirements and achievingprogram goals and objectives throughthe sharing of information and otherlearning activities.ACOs are evaluated on33 quality measures in4 domains of patient/caregiver experience:preventive health,care coordination/patient safety, andat-risk populations, asestablished by CMS. Phase in pay-forperformance measuresas organizationscomplete their secondand third years ofprogram participation(P6, Goal 1). Track quality andcost metrics reportedby participants tomonitor and improveperformance(P3, Goal 3). Promote patientengagement by sharinghealth care expertiseand increasing thebeneficiary’s role inshared decisionmaking(P2, Goal 2). Reduce unnecessaryhealth care coststhrough increasedcare coordination(P1, Goal 3). Improve thequality of care forMedicare FFSbeneficiariesthroughaccountabilityand redesignedinfrastructure andcare processes. Increase patientengagement tomake informedhealth caredecisions. Promotecoordinationand informationamong healthcare providers.* Priorities to which the program aligns Primary priority** Please see Appendix A on the last page, which includes a table of the six NQS Priorities and Long-Term Goals.6
National Quality Strategy Agency-Specific PlanCenters for Medicare & Medicaid Services (CMS)Centers for Medicare & Medicaid Services (CMS) (Continued)ProgramDescriptionNQS Priorities*Million HeartsInitiativeMillion Hearts is a nationalHHS initiative, co-ledby CMS and CDC andexecuted by Federal,State, and private sectorpartners, that coordinatescardiovascular diseaseprevention and treatmentactivities across the publicand private sectors.12345Partnership forPatientsThis public-privatepartnership promotespatient safety and qualityby aiming to (1) keeppatients from gettinginjured or sicker, and(2) help patients healwithout complication. Thisinitiative strives to reducepreventable hospitalacquired conditionsand 30-day hospitalreadmissions.12345TMCurrent-Year ActivitiesMetricsFuture-Year Plans**Vision/End Goals6 Conduct educational campaignsto increase awareness about heartdisease prevention and empowerpatients to take control of theirheart health. Participate in community efforts topromote smoke-free air policies andreduce sodium in the food supply. Use health information technologyand quality improvement initiatives tostandardize and improve the deliveryof care for high blood pressure andhigh cholesterol. Scale-up proven clinical andcommunity strategies across thenation that address major riskfactors for cardiovascular disease,including appropriate Aspirin usefor those at risk, Blood pressurecontrol, Cholesterol management,and Smoking cessation (the ABCS ofcardiovascular disease).This initiative will track thenumber of heart attacksand strokes each year inthe United States. Theinitiative will also track keymeasures related to theABCS of cardiovasculardisease (e.g., smokingprevalence, trans fatconsumption, aspirin use).The National Committeefor Quality Assurance willalso align cardiovascularHealthcare EffectivenessData and Information Set(HEDIS) measures to theMillion Hearts campaign. Prevent 1 million heartattacks and strokes by2017 (P4, Goal 3). Achieve 65% adherenceto proven preventiontechniques—aspirinuse, blood pressurecontrol, and treatmentfor high cholesterol(P4, Goal 2). Reduce smokingprevalence from 19% to17% of the population(P5, Goal 2). Decrease sodiumintake by 20% and transfat consumption by50% of the population(P5, Goal 2). EmpowerAmericans to makehealthy choices. Improve carefor people atrisk by focusingon the ABCS ofcardiovasculardisease suchas better bloodpressure controland smokingcessation.6 Assist 26 Hospital EngagementNetworks with conducting trainingprograms for hospitals to increasepatient safety, providing technicalassistance to hospitals to achievequality measurement goals, andimplementing a tracking system tomonitor hospital progress on qualityimprovement goals. Provide educational resourceson how health care providers canmake care safer and improvecare coordination.This partnership trackspatient safety and qualitythrough the followingmeasures: hospitalreadmission rates, adversedrug events (ADE),catheter-associated urinarytract infections (CAUTI),central line-associatedbloodstream infections(CLABSI), injuries fromfalls and immobility,obstetrical adverse events,pressure ulcers, surgicalsite infections, venousthromboembolism (VTE),ventilator-associatedpneumonia (VAP), andother hospital-acquiredconditions. Further collaborationamong health careproviders to reducecomplications in caretransitions (P3, Goal 1). Increase the numberof community-basedorganizations (CBOs) topartner with acute-carehospitals and providecare transition services(P1, Goal 1). Continue to identifyall-cause harms anddevelop effectivestrategies for preventingthem in the future(P1, Goal 2). Reducepreventablehospital-acquiredconditions 40%by 2013. Decrease 30day hospitalreadmissions 20%by 2013.* Priorities to which the program aligns Primary priority** Please see Appendix A on the last page, which includes a table of the six NQS Priorities and Long-Term Goals.7
National Quality Strategy Agency-Specific PlanCenters for Medicare & Medicaid Services (CMS)Centers for Medicare & Medicaid Services (CMS) (Continued)ProgramDescriptionNQS Priorities*PhysicianQualityReportingSystem (PQRS)PQRS promotes thereporting of qualitymeasure data through theuse of incentive paymentsand payment adjustmentsfor participating providerswho satisfactorily reporton quality measures datafor covered professionalservices for Part BMedicare beneficiaries.This program helpswith the implementationof the goals of valuebased purchasing.123456Current-Year ActivitiesMetricsFuture-Year Plans**Vision/End Goals Collaborate with participantson program and data collectionrequirements. Align participation and reportingcriteria with other quality reportingprograms within CMS. Conduct monthly national calls withproviders to discuss the program andother relevant updates, providing timefor questions and answers. Provide incentive payment of 0.5%of eligible professional’s totalestimated Medicare Part B PhysicianFee Schedule (PFS) to those whosuccessfully report PQRS measures.For 2012, 143 individualquality measures and 12measure groups wereeligible for claims-basedreporting. Reportingmechanisms includeclaims, qualified registry,qualified Electronic HealthRecord (EHR), and GroupPractice Reporting Option(GPRO) Web interface.Measure specificationscan vary by year. Increase the numberof PQRS participantsto expand the qualitymeasure datacollecting and reporting(P3, Goal 1). Continue alignmentefforts with otherCMS quality reportingprograms to reduceadministrativeburden and increaseparticipation in qualityreporting (P3, Goal 1). Advance datacollection andreporting of qualityinformation. Reduceadministrativeburden of reportingwith other qualityreporting programswherever possible.* Priorities to which the program aligns Primary priority** Please see Appendix A on the last page, which includes a table of the six NQS Priorities and Long-Term Goals.Starting in 2015, PQRSwill no longer use anincentive structure.Medicare Part B PFSpayment adjustmentswill decrease by 1.5% fornonparticipants based onthe 2013 reporting year.8
National Quality Strategy Agency-Specific PlanCenters for Medicare & Medicaid Services (CMS)Appendix A. National Quality Strategy Priorities and Long-Term Goals#PriorityLong-Term Goals (Recommended by the National Priorities Partnership)1Making care safer by reducingharm caused in the deliveryof care.1. Reduce preventable hospital admissions and readmissions.2. Reduce the incidence of adverse health care-associated conditions.3. Reduce harm from inappropriate or unnecessary care.2Ensuring that each person andfamily are engaged as partnersin their care.1. Improve patient, family, and caregiver experience of care related to quality, safety, and access across settings.2. In partnership with patients, families, and caregivers—and using a shared decisionmaking process—develop culturally sensitive and understandablecare plans.3. Enable patients and their families and caregivers to navigate, coordinate, and manage their care appropriately and effectively.3Promoting effectivecommunication and coordinationof care.1. Improve the quality of care transitions and communications across care settings.2. Improve the quality of life for patients with chronic illness and disability by following a current care plan that anticipates and addresses pain and symptommanagement, psychosocial needs, and functional status.3. Establish shared accountability and integration of communities and health care systems to improve quality of care and reduce health disparities.456Promoting the most effectiveprevention and treatmentpractices for the leading causesof mortality, starting withcardiovascular disease.1. Promote cardiovascular health through community interventions that result in improvement of social, economic, and environmental factors.Working with communitiesto promote wide use ofbest practices to enablehealthy living.1. Promote healthy living and well-being through community interventions that result in improvement of social, economic, and environmental factors.Making quality care moreaffordable for individuals,families, employers, andgovernments by developingand spreading new health caredelivery models.1. Ensure affordable and accessible high-quality health care for people, families, employers, and governments.2. Promote cardiovascular health through interventions that result in adoption of the most important healthy lifestyle behaviors across the lifespan.3. Promote cardiovascular health through receipt of effective clinical preventive services across the lifespan in clinical and community settings.2. Promote healthy living and well-being through interventions that result in adoption of the most important healthy lifestyle behaviors across the lifespan.3. Promote healthy living and well-being through receipt of effective clinical preventive services across the lifespan in clinical and community settings.2. Support and enable communities to ensure accessible, high-quality care while reducing waste and fraud.9
with the target price set by CMS and providers. CMS monitors clinical quality, patient experience, and outcomes of care. Models 2-4 use a standardized set of measures established by CMS. Additional measures for all models can be proposed by applicants. (Model 1 implementation is currently suspended and under review.) Further coordination











