Transcription
What’s New in the Standards of Medical Care in Diabetes – 2016?William H. Herman, MD, MPHFriday, March 4, 20161:00 p.m. – 1:45 p.m.Caring for patients with diabetes is hard work. Each year, the American Diabetes Associationupdates the Standards of Medical Care in Diabetes to reflect new evidence, to organize theevidence to make it more useful to clinicians, and to assist clinicians in tailoring treatment tovulnerable populations with diabetes and making care more patient-centered. In thispresentation, Dr. Herman highlights some of the important revisions to the Standards of Care in2016 in the areas of obesity management for the treatment of type 2 diabetes, SGLT-2 inhibitorsfor the management of type 2 diabetes, lipid management in diabetes, the treatment of diabeticretinopathy, and the treatment of gestational diabetes mellitus.References:Obesity Management for the Treatment of Type 2 Diabetes1. Gudzune KA, Doshi RS, Mehta AK, Chaudhry ZW, Jacobs DK, Vakil RM, Lee CJ, BleichSN, Clark JM. Efficacy of commercial weight-loss programs: an updated systematicreview. Ann Intern Med 2015;162:501-512. Review. Erratum in: Ann Intern Med. 2015May 19;162(10):739-740.2. Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic andclinical review. JAMA 2014;311:74-86.3. Pi-Sunyer X, Astrup A, Fujioka K, Greenway F, Halpern A, Krempf M, Lau DC, le RouxCW, Violante Ortiz R, Jensen CB, Wilding JP; SCALE Obesity and PrediabetesNN8022-1839 Study Group. A Randomized, Controlled Trial of 3.0 mg of Liraglutide inWeight Management. N Engl J Med 2015;373:11-22.4. Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD, AminianA, Pothier CE, Kim ES, Nissen SE, Kashyap SR; STAMPEDE Investigators. Bariatricsurgery versus intensive medical therapy for diabetes--3-year outcomes. N Engl J Med2014;370:2002-2013.5. Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness andrisks of bariatric surgery: an updated systematic review and meta-analysis, 2003-2012.JAMA Surg 2014;149:275-287.Approaches to Glycemic Treatment1. Nathan DM, Buse JB, Kahn SE, Krause-Steinrauf H, Larkin ME, Staten M, Wexler D,Lachin JM; GRADE Study Research Group. Rationale and design of the glycemiareduction approaches in diabetes: a comparative effectiveness study (GRADE).Diabetes Care 2013;36:2254-2261.2. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, DevinsT, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE; EMPA-REG OUTCOMEInvestigators. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes.N Engl J Med 2015;373:2117-2128.Cardiovascular Disease and Risk Management1. Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, Darius H,Lewis BS, Ophuis TO, Jukema JW, De Ferrari GM, Ruzyllo W, De Lucca P, Im K,Bohula EA, Reist C, Wiviott SD, Tershakovec AM, Musliner TA, Braunwald E, Califf RM;
IMPROVE-IT Investigators. Ezetimibe Added to Statin Therapy after Acute CoronarySyndromes. N Engl J Med 2015;372:2387-2397.2. Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, de Craen AJ, Seshasai SR,McMurray JJ, Freeman DJ, Jukema JW, Macfarlane PW, Packard CJ, Stott DJ,Westendorp RG, Shepherd J, Davis BR, Pressel SL, Marchioli R, Marfisi RM, MaggioniAP, Tavazzi L, Tognoni G, Kjekshus J, Pedersen TR, Cook TJ, Gotto AM, Clearfield MB,Downs JR, Nakamura H, Ohashi Y, Mizuno K, Ray KK, Ford I. Statins and risk ofincident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet2010;375:735-742.3. Ridker PM, Pradhan A, MacFadyen JG, Libby P, Glynn RJ. Cardiovascular benefits anddiabetes risks of statin therapy in primary prevention: an analysis from the JUPITER trial.Lancet 2012;380:565-571.4. Richardson K, Schoen M, French B, Umscheid CA, Mitchell MD, Arnold SE, HeidenreichPA, Rader DJ, deGoma EM. Statins and cognitive function: a systematic review. AnnIntern Med 2013;159:688-697.Microvascular Complications and Foot Care1. Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, Gibson A, Sy J,Rundle AC, Hopkins JJ, Rubio RG, Ehrlich JS; RISE and RIDE Research Group.Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials:RISE and RIDE. Ophthalmology 2012;119:789-801.Management of Diabetes in Pregnancy1. Balsells M, García-Patterson A, Solà I, Roqué M, Gich I, Corcoy R. Glibenclamide,metformin, and insulin for the treatment of gestational diabetes: a systematic review andmeta-analysis. BMJ 2015;350:h102.
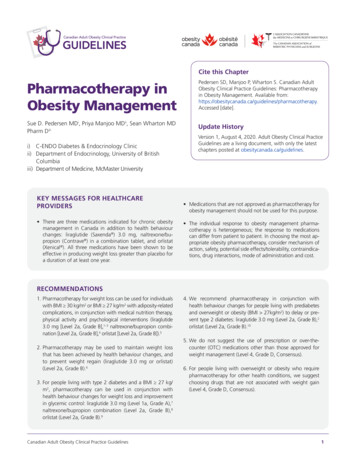
What’s New in the2016 Standards ofMedical Care in DiabetesSpeaker Financial DisclosureInformationDr. Herman serves onData Safety Monitoring Boards forMerck and LexiconWilliam H. Herman, MD, MPHStefan S. Fajans/GlaxoSmithKline Professor of DiabetesProfessor of Internal Medicine and EpidemiologyUniversity of MichiganDirector, Michigan Center for Diabetes Translational ResearchChair, American Diabetes Association Professional Practice CommitteeOutlineOutline Obesity management in the treatmentof type 2 diabetes The role of SGLT-2 inhibitors in thetreatment of type 2 diabetes Controversies in lipid management indiabetes New treatments for diabetic retinopathy Pharmacologic treatments forgestational diabetes mellitus Obesity management in the treatmentof type 2 diabetes The role of SGLT-2 inhibitors in thetreatment of type 2 diabetes Controversies in lipid management indiabetes New treatments for diabetic retinopathy Pharmacologic treatments forgestational diabetes mellitusDietRecommendations Diet, physical activity, and behavioraltherapy designed to achieve 5% weightloss should be prescribed for overweightand obese patients with type 2 diabetesready to achieve weight loss. Interventions should be high intensity ( 16sessions in 6 months) and offer long-termweight maintenance counseling.ADA. Diabetes Care 39(Suppl 1):S47, 2016Components and Costs of High IntensityCommercial or Proprietary Weight-Loss StrategiesWeightWatchersLow-calorieconventional foodsActivitytrackingSelfmonitoringGroup sessionsOnline coachingOnline community forum43Jenny CraigLow-calorie mealreplacementsEncouragesincreasedactivityGoal settingSelfmonitoring1-on-1 counseling570SupportMonthlyCost, NutrisystemLow-calorie mealreplacementsExercise plansSelfmonitoring1-on-1 counselingOnline community forum280HMRVery-low-calorie orlow-calorie mealreplacementsEncouragesincreasedactivityGoal settingGroup sessionsTelephone coachingMedical supervision682MedifastVery-low-calorie orlow-calorie itoring1-on-1 counselingOnline coaching424OPTIFASTVery-low-calorie orlow-calorie solving1-on-1 counselingGroup supportMedical supervision665Adapted from KA Gudzune. Ann Int Med 162:501, 2015
Differences in Mean Percentage of Weight Changewith Low Calorie* and Very Low Calorie**Weight-Loss Programs over Time10LCDVLCDDifferenceinMean %WeightChange9.38.24.12.72.8 3.02.912 mos24 mos03 mos6 mos* Weight Watchers** HMR or OptifastAdapted from KA Gudzune. Ann Int Med 162:501, 2015FDA-Approved Medications for the Long-TermTreatment of Obesity1-Year weight change statusDrug nameAdult dosingAdverse effectsAveragewholesale price(per month)Average weightloss relative toplacebo% Patients with 5% loss ofbaseline weightCommonSeriousOrlistat(Xenical)120 mg t.i.d. 6153.4 kg35-73%Abdominal pain,fecal urgency, fatmalabsorptionLiver failure andoxalatenephropathyLorcaserin(Belviq)10 mg b.i.d. 2633.2 kg38-48%Headache,fatigueSerotoninsyndrome, heartvalve disorders( 2.4%)Phentermine/topiramate ER(Qsymia)Maximum dose:15 mg/92 mgq.d. 2398.9 heTopiramate istertogenic (cleftlip/ palate)Naltrexone/bupropion(Contrave)Maximum dose:16 mg/180 mgb.i.d. 2392.0-4.1 iaLiraglutide(Saxenda)Maintenancedose: 3 mg s.c.q.d. 1,2825.8-5.9 achePancreatitis,acute renalfailure,contraindicatedwith MTC orMEN2Adapted from ADA. Diabetes Care 39(Suppl 1):S47, 2016Metabolic Surgery:Baseline Characteristics of the STAMPEDEPopulation with Type 2 DiabetesParameterIntensiveMedicalTherapy(N 40)GastricBypass(N 48)SleeveGastrectomy(N 49)Age – yrs50 848 848 8Female sex (%)685878Caucasian race (%)73757436.4 3.037.1 3.436.1 3.9Body-mass index – (kg/m2)Body-mass index 35 kg/m2 (%)Duration of diabetes – yrsInsulin users (%)4527378.8 5.388.0 5.368.3 4.49434443PR Schauer. N Engl J Med 370:2002, 2014PharmacotherapyRecommendations Weight loss medications may be effective asadjuncts to diet, physical activity, and behavioralcounseling for selected patients with type 2diabetes and BMI 27 kg/m2. If a patient’s response to weight loss medicationsis 5% after 3 months or if there are safety ortolerability issues at any time, the medicationshould be discontinued and alternativemedications or treatment approaches should beconsidered.ADA. Diabetes Care 39(Suppl 1):S47, 2016Bariatric SurgeryRecommendations Bariatric surgery may be considered for adultswith BMI 35 kg/m2 and type 2 diabetes,especially if diabetes or associated comorbiditiesare difficult to control with lifestyle andpharmacological therapy. Patients with type 2 diabetes who haveundergone bariatric surgery need lifelong lifestylesupport and annual medical monitoring.ADA. Diabetes Care 39(Suppl 1):S47, 2016Mean Change in BMI by Treatment Group,STAMPEDE StudyPR Schauer. N Engl J Med 370:2002, 2014
Mean Change in Glycated Hemoglobin byTreatment Group, STAMPEDE StudyPolar Chart of Scores of Quality-of-Lifeat 3-years by Treatment Group, STAMPEDE StudyPR Schauer. N Engl J Med 370:2002, 2014Meta-analysis of Risks of Bariatric Surgery fromRandomized Controlled Trials, 2002-2012Mean (95% CI)Mortality 30 dEstimates, %Study/arm/No. of patients0.08 (0.01-0.24)15/30/1803Mortality 30 dEstimates, %Study/arm/No. of patients0.31 (0.01-0.75)15/30/1703Complication ratesEstimates, %Study/arm/No. of patients17.00 (11.00-23.00)16/30/1778Reoperation ratesEstimates, %Study/arm/No. of patients6.95 (3.27-12.04)12/23/1322PR Schauer. N Engl J Med 370:2002, 2014Outline Obesity management in the treatmentof type 2 diabetes The role of SGLT-2 inhibitors in thetreatment of type 2 diabetes Controversies in lipid management indiabetes New treatments for diabetic retinopathy Pharmacologic treatments forgestational diabetes mellitusSH Chang. JAMA Surg 149:275, 2014Algorithm for AntihyperglycemicTherapy in Type 2 DiabetesGlycemia Reduction Approaches in Diabetes:A Comparative Effectiveness Study(GRADE)Specific Aim to compare the effectiveness of fourmedications combined with metformin toachieve and maintain HbA1c 7%ADA. Diabetes Care 39(Suppl 1):S52, 2016
ScreeningType 2 diabetesTreated with metformin aloneHbA1c 6.8% at screeningLess than 10 years duration at randomizationMetformin run-inWhere do SGLT-2 Inhibitors Fit into theAlgorithm for Antihyperglycemic Therapy?Titratemetformin to 1000 (min) – 2000 (goal) mg/dayHbA1c 6.8-8.5% at final run-in visitRandomizationn 6000 eligible subjectsSulfonylurea(glimepiride)n 1500DPP-IV inhibitor(sitagliptin)n 1500GLP-1 analog(liraglutide)n 1500Insulin(glargine)n 1500Cumulative Incidence of Nonfatal MI,Nonfatal Stroke, or Cardiovascular Death byTreatment Group, EMPA-REG Interpreting the results of the EMPA-REGOutcome Trial that examined the effects ofempagliflozin, as compared with placebo,on cardiovascular morbidity and mortalityin patients with type 2 diabetes at highrisk for cardiovascular events who werereceiving standard care.Absolute Reductions in Incidence ofCardiovascular Outcomes in EMPA-REGPlacebo(N 2333)Empagliflozin(N rimary outcomecardiovasculardeath, non-fatalmyocardialinfarction, or nonfatal stroke43.937.4-6.5 (-12.6, -0.4)Placebo(N 2333)Pooled empagliflozin(N 4687)63 963 9Sex (% male)7271Race (% White)727330.7 5.230.6 5.3 10 years since diagnosis of type 2 diabetes (%)5757Insulin treated (%)49488.08 0.848.07 0.85Coronary artery disease7676History of myocardial infarction4647Coronary artery bypass graft24Cardiac failureHistory of strokePeripheral artery disease21Characteristic*Age – years SDBody mass index – kg/m2Glycated hemoglobin (%)0.04All-cause mortality28.619.4-9.1 (-13.8, -4.5) 0.001Cardiovasculardeath20.212.4-7.7 (-11.6, -3.9) 0.001Hospitalization forheart failure14.59.4-5.1 (-8.4, -1.8)0.003B Zinman. N Engl J Med 373:2117, 2015Baseline Characteristics of the EMPA-REG Study PopulationRate differencep-value(95% CI)B Zinman. N Engl J Med 373:2117, 2015Baseline Characteristics of the EMPA-REG Study PopulationPlacebo(N 2333)Pooled empagliflozin(N 4687)63 963 9Sex (% male)7271Race (% White)727330.7 5.230.6 5.3 10 years since diagnosis of type 2 diabetes (%)5757Insulin treated (%)49488.08 0.848.07 0.85Coronary artery disease7676History of myocardial infarction464725Coronary artery bypass graft24251110Cardiac failure11102423History of stroke242321Peripheral artery disease21CV risk factor (%)Characteristic*Age – years SDBody mass index – kg/m2Glycated hemoglobin (%)CV risk factor (%)B Zinman. N Engl J Med 373:2117, 201521B Zinman. N Engl J Med 373:2117, 2015
Outline Obesity management in the treatmentof type 2 diabetes The role of SGLT-2 inhibitors in thetreatment of type 2 diabetes Controversies in lipid management indiabetes New treatments for diabetic retinopathy Pharmacologic treatments forgestational diabetes mellitusRecommendation for Statin Treatment inPeople with DiabetesAgeRisk factorsRecommended statin intensity 40 yearsNoneNone40-75 years 75 yearsASCVD risk factor(s)*Moderate or highASCVDHighNoneModerateASCVD risk factorsHighASCVDHighNoneModerateASCVD risk factorsModerate or highASCVDHigh*ASCVD risk factors include LDL cholesterol 100 mg/dL (2.6 mmol/L), high blood pressure,smoking, overweight and obesity, and family history of premature ASCVD.ADA. Diabetes Care 39(Suppl 1):S60, 2016High-intensity and moderate-intensitystatin therapy*High-intensity statin therapyModerate-intensity statin therapyLowers LDL cholesterol by 50%Lowers LDL cholesterol by 30% to 50%Atorvastatin 40-80 mgAtorvastatin 10-20 mgRosuvastatin 20-40 mgRosuvastatin 5-10 mgSimvastatin 20-40 mgWhere do non-statin lipidlowering therapies fit into themanagement of dyslipidemiain diabetes?Pravastatin 40-80 mgLovastatin 40 mgFluvastatin XL 80 mgIMPROVE-ITPitavastatin 2-4 mg*Once-daily dosing.ADA. Diabetes Care 39(Suppl 1):S60, 2016Efficacy of Ezetimibe Added to StatinTherapy after Acute Coronary SyndromesLipid Management The addition of exetimibe to moderateintensity statin therapy provides additionalcardiovascular benefit compared withmoderate-intensity statin therapy alone andmay be considered for patients with a recentacute coronary syndrome with LDLcholesterol 50 mg/dl.CP Cannon. N Engl J Med 372:2387, 2015ADA. Diabetes Care 39(Suppl 1):S60, 2016
Recommendation for Statin and Combination Treatment inPeople with DiabetesAge 40 years40-75 years 75 yearsRecommendedstatin intensityRisk factorsNoneNoneASCVD risk factor(s)Moderate or highASCVDHighNoneModerateASCVD risk factorsHighASCVDHighACS and LDL cholesterol 50 mg/dL in patients whocannot tolerate high-dose statinsModerate plusezetimibeNoneModerateASCVD risk factorsModerate or highASCVDHighACS and LDL cholesterol 50 mg/dL in patients whocannot tolerate high-dose statinsModerate plusezetimibeADA. Diabetes Care 39(Suppl 1):S60, 2016Lipid Management, continued Combination therapy (statin/fibrate) has notbeen shown to improve atheroscleroticcardiovascular disease outcomes and isgenerally not recommended. However,therapy with statin and fenofibrate may beconsidered for men and both triglyceride level 204 mg/dL and HDL cholesterol level 34mg/dL.ADA. Diabetes Care 39(Suppl 1):S60, 2016Lipid Management, continued Combination therapy (statin/niacin) has notbeen shown to provide additionalcardiovascular benefit above statin therapyalone and may increase the risk of stroke andis not generally recommended.Does statin therapy increasethe risk of type 2 diabetes?ADA. Diabetes Care 39(Suppl 1):S60, 2016Association Between Statin Therapy and IncidentDiabetes in 13 Major Cardiovascular TrialsOverall (P 11.2% [95% CI 0.0-50.2%])Association Between Different Statins andDevelopment of Diabetes1.09 (1.02-1.17)N Sattar. Lancet 375:735, 2010N Sattar. Lancet 375:735, 2010
Association Between Different Statins andDevelopment of DiabetesAtorvastatin1.14 (0.89-1.46)Simvastatin1.11 (0.97-1.26)Rosuvastatin1.18 (1.04-1.33)PravastatinHow do the benefits of statintherapy compare to the risks ofstatin therapy?1.03 (0.90-1.19)Lovastatin0.98 (0.70-1.38)Overall1.09 (1.02-1.17)N Sattar. Lancet 375:735, 2010Treating 255 nondiabetic patients withstatins for 4 years will result in: 1 additional case of diabetes 5.1 fewer cardiovascular eventsN Sattar. Lancet 375:735, 2010Cardiovascular Benefits and Diabetes Risks ofStatin Therapy in Primary Prevention:The JUPITER TrialNo Major Risk Factors for DiabetesCVDDiabetesP Ridker. Lancet 380:565, 2012Cardiovascular Benefits and Diabetes Risks ofStatin Therapy in Primary Prevention:The JUPITER TrialOne or More Major Risk Factors for DiabetesCVDDiabetesP Ridker. Lancet 380:565, 2012Do statins cause cognitiveimpairment?
Statins and Cognitive Function:A Systematic ReviewOutlineK Richardson. Ann Intern Med 159:688, 2013Dementia0.87 (0.82-0.92)Alzheimer disease0.79 (0.63-0.99)Mild cognitive impairment0.66 (0.51-0.86)Favors Statin UsersFavors Nonusers Obesity management in the treatmentof type 2 diabetes The role of SGLT-2 inhibitors in thetreatment of type 2 diabetes Controversies in lipid management indiabetes New treatments for diabetic retinopathy Pharmacologic treatments forgestational diabetes mellitusDiabetic Retinopathy: Macular EdemaHard exudatesDiskHemorrhagesDiskHard exudatesMaculaType 1HemorrhagesType 2Intravitreal Ranibizumab for theTreatment of Diabetic Macular EdemaCompared to sham-treated patients, thosetreated with intravitreal ranibizumab were:Diabetic macular edemaRandomization (1 eye per patient)24-month controlled treatment period(monthly intravitreal/sham injections: rescue laser,if eligible, beginning month 3)QD Nguyen. Ophthalmology 119:789, 2012 More likely to achieve VA 20/40 or betterMore likely to have improved visual acuityLess likely to have worsened visual acuityLess likely to require laser proceduresNo more likely to experience ocular ornon-ocular harmQD Nguyen. Ophthalmology 119:789, 2012
Outline Obesity management in the treatmentof type 2 diabetes The role of SGLT-2 inhibitors in thetreatment of type 2 diabetes Controversies in lipid management indiabetes New treatments for diabetic retinopathy Pharmacologic treatments forgestational diabetes mellitusPharmacologic Therapy of GDM Medications should be added if required toachieve glycemic targets. Insulin is the first line agent recommended forthe treatment of GDM in the U.S. Individual randomized controlled trials supportthe efficacy and short-term safety ofmetformin (pregnancy category B) andglyburide (pregnancy category B). However,both agents cross the placenta, and long-termsafety data are not available for either agent.Management of GDM 70 to 85% of women diagnosed with GDMusing Carpenter-Coustan or National DiabetesData Group (NDDG) criteria can control GDMwith lifestyle modifications alone. The proportion is even greater when the lowerIADPSG diagnostic criteria are used.Pharmacologic Treatmentsfor GDM: Glyburide vs Insulin Effective (only 10% requiresupplemental insulin) 2-fold higher incidence of macrosomia 100 g higher mean birth weight 2-fold higher incidence of neonatalhypoglycemiaBalsells. BMJ 2015;350:h102Pharmacologic Treatmentsfor GDM: Metformin vs Insulin Less effective (⅓ to ½ requiresupplemental insulin) Less maternal weight gain Less pregnancy-induced hypertension Less severe neonatal hypoglycemia Lower gestational age at delivery andmore preterm birthBalsells. BMJ 2015;350:h102Pharmacologic Treatmentsfor GDM: Conclusions Insulin is the preferred treatment Metformin (plus insulin when required)performs slightly better than insulinalone Glyburide is inferior to both insulin andmetforminBalsells. BMJ 2015;350:h102
Outline Obesity management in the treatmentof type 2 diabetes The role of SGLT-2 inhibitors in thetreatment of type 2 diabetes Controversies in lipid management indiabetes New treatments for diabetic retinopathy Pharmacologic treatments forgestational diabetes mellitus
2.7 4.1 2.8 2.9 9.3 8.2 3.0 0 10 3 mos 6 mos 12 mos 24 mos Difference in Mean % Weight Change LCD VLCD Adapted from KA Gudzune. Ann Int Med 162:501, 2015 * Weight Watchers ** HMR or Optifast Pharmacotherapy Recommendations Weight loss medications may be effective as adjuncts to diet, physical activity, and behavioral counseling for selected .