Transcription
Prior Authorization of Radiation Therapy forFidelis CareProvider Orientation 2015 eviCore healthcare. All Rights Reserved. This presentation contains CONFIDENTIAL and PROPRIETARY information.
Company HighlightsHeadquartered in Bluffton, SC4K employeesincluding 1K cliniciansOffices across the US including: Lexington, MA Melbourne, FL Colorado Springs, CO Plainville, CT Franklin, TN Sacramento, CA Greenwich, CTSHARINGA VISIONAT THE CORE OF CHANGE.100M membersmanaged nationwide12M claimsprocessed annually2
Integrated SolutionsLAB MANAGEMENT19M livesMEDICAL ONCOLOGY14M livesRADIATION THERAPY29M livesMUSCULOSKELETAL34M livesSPECIALTY DRUG100k livesRADIOLOGY65M livesSLEEP14M livesCARDIOLOGY46M livesPOST-ACUTE CARE320k lives3
Since 2009 20 regional and national clients 29M total membershipRadiation Therapy SolutionExperience 19.7M Commercial membership 5.3M Medicare membership 4M Medicaid membership200 average cases built per day4
Our Clinical Approach5
Radiation Therapy by the Numbers1517Radiationoncologists on staffRadiation Therapytrained nurses on staffCase Statistics70%Cases ImmediatelyApproved291.3%Appeal RateMillion livescovered47%Web Utilization Rate6
Evidence-Based GuidelinesThe foundation of our radiation therapy m a panelof communityphysiciansExpertsassociatedwith academicinstitutionsCompliantwith MedicareNCDs/LCDsAdvisory Board MembersAligned with National Societies American Society for Radiation Oncology Dr. Anthony Berson – eviCore healthcare American College of Radiology Memorial Sloan-Kettering, NY National Comprehensive Cancer Network (NCCN) Stanford University Medical Center, CA Medicare Guidelines Shields Oncology, MA Center for Radiation Oncology, NY Beth Israel Deaconess Medical Center; Harvard, MA Detroit Medical Center, Sinai Grace Hospital, MI7
Service Model8
Client Provider OperationsThe Client Provider Operations team is responsible for high-level service delivery toour health plan clients as well as ordering and rendering providers nationwideBest ColorsClient ProviderRepresentativesClient ProviderRepresentativesare cross-trained toinvestigate escalatedprovider and healthplan issues.Client ServiceManagersRegional ProviderEngagement ManagersClient Service Managerslead resolution ofcomplex service issuesand coordinate withpartners for continuousimprovement.Regional Provider EngagementManagers are on-the-groundresources who serve as the voice ofeviCore to the provider community.9
Why Our Service Delivery Model WorksOne centralized intake pointallows for timely identification,tracking, trending, and reportingof all issues. It also enableseviCore to quickly identify andrespond to systemic issuesimpacting multiple providers.Complex issues are escalatedto resources who are thesubject matter experts and canquickly coordinate with matrixpartners to address issues at aroot-cause level.Routine issues are handled bya team of representatives whoare cross trained to respond to avariety of issues. There is noreliance on a single individual torespond to your needs.10
Radiation Therapy Prior AuthorizationProgram for Fidelis Care11
Program OvervieweviCore will begin accepting requests on September 20, 2017 for datesof service October 1, 2017 and beyondPrior authorization appliesto services that are: Outpatient Elective/non-emergentPrior authorizationdoes not apply to servicesthat are performed in: Emergency roomInpatient23-hour observationIt is the responsibility of the ordering provider to request priorauthorization approval for services. It is the responsibility of theperforming facility to confirm that the referring physiciancompleted the prior authorization process.12
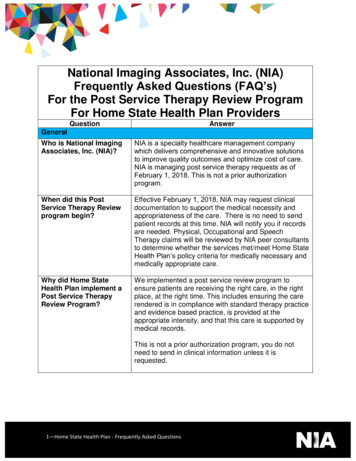
Applicable MembershipAuthorization is required for Fidelis Care members enrolled in the followingprograms: Medicaid Managed Care (MMC)Child Health Plus (CHP)Medicare Advantage (MA)Dual Advantage (DUAL)Medicaid Advantage Plus (MAP)Metal-level Products (qualified health plan)Essential Plan (EP)Healthier Life (HARP)Members who do not require prior authorization are: Fidelis Care at Home (FCAH) Managed Long Term CareFully Integrated Duals Advantage (FIDA)13
Prior authorization is required for allRadiation Therapy treatment techniques,included but not limited to the following:Clinical Modalities 3D Conformal IMRT Image-Guided Radiation Therapy Brachytherapy SRS/SBRT Proton Therapy Hyperthermia RadiopharmaceuticalsTo find a list of CPT(Current Procedural Terminology)codes that require prior authorizationthrough eviCore, please reNon- Clinical Modalities SIM Planning Devices Imaging Physics Management14
Prior Authorization RequestsHow to request prior authorization:www.evicore.comAvailable 24/7 and the quickestway to create prior authorizationsand check existing case statusWEBOr by phone: 1866-706-21087:00 a.m. to 7:00p.m. (EST)Monday - Friday15
Clinical Review ProcessMethods of IntakeSTARTClinical DecisionSupportReal-Time Decision with WebNurseReviewAppropriateDecisionEasy forprovidersand staffMDReviewPeer-topeer16
Needed InformationMemberRendering FacilityMember IDMember nameDate of birth (DOB)Referring/Ordering PhysicianPhysician nameNational provider identifier (NPI)State and Zip CodeFacility nameStreet addressiRequestsPatient’s intended treatment planPatient’s clinical presentationCompleted physician worksheet17
Holistic Treatment Plan RevieweviCore healthcare relies on information about the patient’s unique presentationand physician’s intended treatment plan to authorize all services from the initialsimulation through the delivery of the last fraction of radiation. Providers specify a diagnosis rather than request individual CPT codes Diagnosis and treatment plan compared to the evidence-based guidelines developed byour Medical Advisory Board If request is authorized/covered or partially authorized/covered, then the treatmenttechnique and number of fractions will be provided For questions about specific CPT codes that are included with each episode of care,please reference the eviCore Radiation Therapy Coding Guidelines located viders.aspx?solution Radiation%20Therapy#ReferenceGuidelines Correct coding guidelines are based on ASTRO/ACR Radiation Therapy coding resources.18
Prior Authorization OutcomesApproved Requests: Delivery:Denied Requests:Delivery:Delivery:All requests are processed within 3 business daysafter receipt of all necessary clinical information.Radiation therapy authorization time spans canrange from a few weeks to six months dependent onthe treatment plan and cancer type. Faxed to ordering providerMailed to the memberInformation can be printed on demand from theeviCore healthcare Web Portal Communication of denial determinationCommunication of the rationale for the denialHow to request a Peer Review Faxed to the ordering providerMailed to the member19
Prior Authorization Outcomes – Commercial/MedicaidReconsiderations Peer-to-Peer Review: Additional clinical information can be providedwithout the need for a physician to participateMust be requested on or before the anticipated dateof serviceIf a request is denied and requires further clinicaldiscussion for approval, we welcome requests forclinical determination discussions from referringphysicians. In certain instances, additionalinformation provided during the consultation issufficient to satisfy the medical necessity criteria forapproval.Peer-to-Peer reviews can be scheduled at a timeconvenient to your physicianPeer-to-Peer Review20
Prior Authorization Outcomes – Medicare / Medicare AdvantagePre-Decision Consultation If your case requires further clinical discussion for approval, we welcomerequests for clinical determination discussions from referring physiciansprior to a decision being rendered. In certain instances, additional information provided during the predecision consultation is sufficient to satisfy the medical necessity criteriafor approval21
Special CircumstancesAppeals Retro Requests must be submitted with 3 businessdays following the first day of treatment. Requestssubmitted after 3 business days will beadministratively denied. Retros are reviewed for medical necessity. Turnaround time on retro requests is 30 calendar days.Retrospective Studies:Outpatient UrgentStudies:eviCore will process first level appealsRequests for appeals must be submitted toeviCore within 60 business days of the initialdetermination for Medicaid, HARP, and Medicare,and 180 calendar days for Essential Plan andChild Health Plus.The request and all clinical information providedwill be reviewed by a physician other than the onewho made the initial determination.A written notice of the appeal decision will bemailed to the member and faxed to the provider Contact eviCore by phone to request an expeditedprior authorization review and provide clinicalinformationUrgent Cases will be reviewed with 72 hours of therequest.22
Physician Worksheet The physician worksheet is bestcompleted by the physician duringthe initial consultation with thepatient. Inaccurate information causesauthorized services to differ from thosethat are actually delivered and can leadto adverse determinations. You can access the physicianworksheets viders.aspx?solution Radiation%20Therapy#ReferenceGuidelines23
Web Portal Services24
eviCore healthcare website Point web browser to evicore.com Click on the “Providers” link Login or Register
Creating An AccountTo create a new account, click Register.26
Creating An AccountSelect a Default Portal, and complete the registration form.27
Creating An AccountReview information provided, and click “Submit Registration.”28
User Registration-ContinuedAccept the Terms and Conditions, and click “Submit.”29
User Registration-ContinuedYou will receive a message on the screen confirming your registration issuccessful. You will be sent an email to create your password.30
Create a PasswordYour password must be atleast (8) characters longand contain the following:Uppercase lettersLowercase lettersNumbersCharacters (e.g., ! ? *)31
Account Log-InTo log-in to your account, enter your User ID and Password. Agree tothe HIPAA Disclosure, and click “Login.”32
Account Overview33
Welcome ScreenProviders will need to be added to your account prior to case submission. Click the “ManageAccount” tab to add provider information.Note: You can access the MedSolutions Portal at any time if you are registered. Click theMedSolutions Portal button on the top right corner to seamlessly toggle back and forthbetween the two portals without having to log-in multiple accounts.34
Add PractitionersClick the “Add Provider” button.35
Add PractitionersEnter the Provider’s NPI, State, and Zip Code to search for the provider record to addto your account. You are able to add multiple Providers to your account.36
Adding PractitionersJohn Smith0123456789123 Test StreetFranklinTN37067(000) 000-0000(111) 111-1111Select the matching record based upon your search criteria37
Manage Your Account Once you have selected a practitioner, your registration will be completed.You can then access the “Manage Your Account” tab to make any necessaryupdates or changes. You can also click “Add Another Practitioner” to add another provider to youraccount.38
Case Initiation39
Initiating A Case Once registered, providers are granted access to the web portal. After logging into your account, a welcome screen provides options. Choose“request a clinical certification/procedure” to begin a new case request.40
Select ProgramSelect the Program for your certification.41
Select ProviderSelect the Practitioner/Group for whom you want to build a case.42
Select Health PlanChoose the appropriate Health Plan for the case request.43
Select Address44
Contact InformationEnter the Physician’s name andappropriate information for thepoint of contact individual.45
Member InformationEnter the member information including the Patient ID number, date of birth, andpatient’s last name. Click “Eligibility Lookup.”46
Clinical Details47
Verify Service SelectionICD-10 CodeICD-10 Code48
Site SelectionSelect the appropriate site for the request.49
Site SelectionConfirm the site selection.50
Clinical Certification Verify all information entered and make any needed changes prior to movinginto the clinical collection phase of the prior authorization process. You will not have the opportunity to make changes after that point.51
Pause/Save OptionOnce you have entered the clinical collection phase of the case process, you can savethe information and return within (2) business days to complete.52
Medical ReviewAcknowledge the Clinical Certification statements, and hit “Submit Case.”53
ApprovalICD-10Once the clinical pathwayquestions are completedand the answers have metthe clinical criteria, anapproval will be issued.Print the screen and storein the patient’s file.54
Medical ReviewIf additional information is required, you will have the option to either uploaddocumentation, enter information into the text field, or contact us via phone.55
Building Additional CasesOnce a case has been submitted for clinical certification, you can return to the MainMenu, resume an in-progress request, or start a new request. You can indicate if anyof the previous case information will be needed for the new request.56
Authorization look up Select Search by Authorization Number/NPI. Enter the provider’s NPI andauthorization or case number. Select Search. You can also search for an authorization by Member Information, and enter the healthplan, Provider NPI, patient’s ID number, and patient’s date of birth.57
Authorization Status58
Eligibility Look Up59
Provider Resources60
Radiation Therapy ResourcesClinical Guidelines, Physician Worksheets, and other resources can be accessed online: aspx?solution Radiation%20Therapy#ReferenceGuidelines Click the “View Physician Worksheets” button to access specific worksheets.61
eviCore Provider Blog Series The eviCore blog series focuses on making processes more efficient and easierto understand by providing helpful tips on how to navigate prior authorizations,avoid peer-to-peer phone calls, and utilize our clinical guidelines. You can access the blog publications from the Media tab or via the direct link athttps://www.evicore.com/pages/media.aspx.62
Provider Resources: Pre-Certification Call CenterPre-CertificationCall CenterWeb-BasedServicesClient ProviderOperations7:00 AM - 7:00 PM local time (866) 706-2108 Obtain pre-certification or check the status of an existing caseDiscuss questions regarding authorizations and case decisionsChange facility or CPT Code(s) on an existing caseDocuments63
Provider Resources: Web-Based ServicesPre-CertificationCall CenterWeb-BasedServiceswww.evicore.comTo speak with a Web Specialist, call (800) 646-0418 (Option # 2) oremail portal.support@evicore.com.Client ProviderOperations Request authorizations and check case status onlineAuto save – no data lostUpload electronic PDF/Word files with additional clinicaldocumentsDocuments64
Provider Resources: Client Provider OperationsPre-CertificationCall CenterWeb-BasedServicesclientservices@evicore.com Client ProviderOperations Eligibility issues (member, rendering facility, and/or orderingphysician)Questions regarding accuracy assessment, accreditation, and/orcredentialingIssues experienced during case creationRequest for an authorization to be resent to the health planDocuments65
Provider Resources: Implementation DocumentProvider Enrollment Questions Contact Fidelis Care at 1-888-FIDELIS]Pre-CertificationCall CenterWeb-BasedServicesFidelis Care Implementation site - includes all althplan/fideliscareClient ProviderOperations Provider Orientation PresentationCPT code list of the procedures that require prior authorizationQuick Reference GuideeviCore clinical guidelinesFAQ documents and announcement lettersDocumentsYou can obtain a copy of this presentation on the implementation site listedabove. If you are unable to locate a copy of the presentation, please contactthe Client Provider Operations team at ClientServices@evicore.com.66
Thank You!67
Fidelis Care . Company Highlights 4K employees including 1K clinicians 100M members . Lexington, MA Colorado Springs, CO Franklin, TN Greenwich, CT 2 SHARING A VISION AT THE CORE OF CHANGE. 3 Integrated Solutions CARDIOLOGY 46M lives RADIOLOGY 65M lives . Providers specify a diagnosis rather than request individual .