Transcription
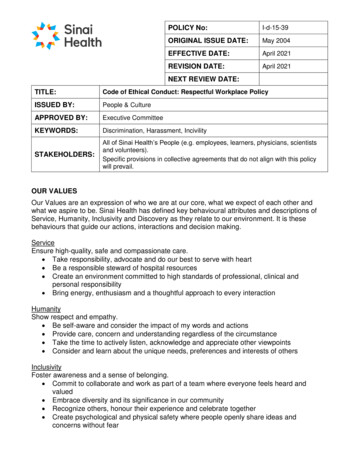
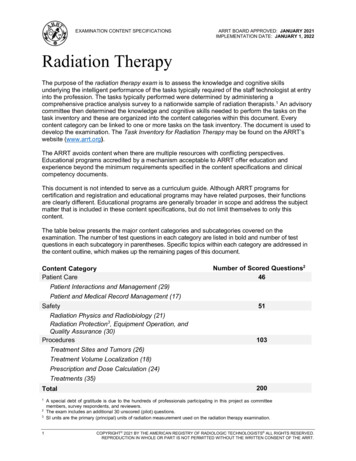
EXAMINATION CONTENT SPECIFICATIONSARRT BOARD APPROVED: JANUARY 2021IMPLEMENTATION DATE: JANUARY 1, 2022Radiation TherapyThe purpose of the radiation therapy exam is to assess the knowledge and cognitive skillsunderlying the intelligent performance of the tasks typically required of the staff technologist at entryinto the profession. The tasks typically performed were determined by administering acomprehensive practice analysis survey to a nationwide sample of radiation therapists.1 An advisorycommittee then determined the knowledge and cognitive skills needed to perform the tasks on thetask inventory and these are organized into the content categories within this document. Everycontent category can be linked to one or more tasks on the task inventory. The document is used todevelop the examination. The Task Inventory for Radiation Therapy may be found on the ARRT’swebsite (www.arrt.org).The ARRT avoids content when there are multiple resources with conflicting perspectives.Educational programs accredited by a mechanism acceptable to ARRT offer education andexperience beyond the minimum requirements specified in the content specifications and clinicalcompetency documents.This document is not intended to serve as a curriculum guide. Although ARRT programs forcertification and registration and educational programs may have related purposes, their functionsare clearly different. Educational programs are generally broader in scope and address the subjectmatter that is included in these content specifications, but do not limit themselves to only thiscontent.The table below presents the major content categories and subcategories covered on theexamination. The number of test questions in each category are listed in bold and number of testquestions in each subcategory in parentheses. Specific topics within each category are addressed inthe content outline, which makes up the remaining pages of this document.Content CategoryPatient CarePatient Interactions and Management (29)Patient and Medical Record Management (17)SafetyRadiation Physics and Radiobiology (21)Radiation Protection3, Equipment Operation, andQuality Assurance (30)ProceduresNumber of Scored Questions24651103Treatment Sites and Tumors (26)Treatment Volume Localization (18)Prescription and Dose Calculation (24)Treatments (35)Total1231200A special debt of gratitude is due to the hundreds of professionals participating in this project as committeemembers, survey respondents, and reviewers.The exam includes an additional 30 unscored (pilot) questions.SI units are the primary (principal) units of radiation measurement used on the radiation therapy examination.COPYRIGHT 2021 BY THE AMERICAN REGISTRY OF RADIOLOGIC TECHNOLOGISTS ALL RIGHTS RESERVED.REPRODUCTION IN WHOLE OR PART IS NOT PERMITTED WITHOUT THE WRITTEN CONSENT OF THE ARRT.
RADIATION THERAPY EXAMINATIONCONTENT OUTLINEARRT BOARD APPROVED: JANUARY 2021IMPLEMENTATION DATE: JANUARY 1, 2022Patient Care1. Patient Interactions and ManagementA. Ethical and Legal Aspects1. patients’ rightsa. consent(*e.g., informed, oral, implied)b. confidentiality (HIPAA)c. American Hospital Association (AHA)Patient Care Partnership (Patients’Bill of Rights)1. privacy2. extent of care (e.g., DNR)3. access to information4. living will, health care proxy,advanced directives5. research participation6. goal of care (e.g., definitive,palliative)2. legal issuesa. verification (e.g., patientidentification, treatment site,prescription)b. common terminology(e.g., battery, negligence,malpractice, beneficence)c. legal doctrines (e.g., respondeatsuperior, res ipsa loquitur)d. restraints versus immobilization (e.g.,positioning aids used to preventmotion)3. ARRT Standards of EthicsB. Interpersonal Communication1. modes of communicationa. verbal/writtenb. nonverbal (e.g., eye contact,touching)2. challenges in communicationa. interactions with others1. language barriers2. cultural and social factors3. physical, sensory, or cognitiveimpairments4. age5. emotional status, acceptance ofcondition (e.g., stage of grief)b. explanation of medical termsc. strategies to improve understanding3. patient educationa. explanation of treatment orprocedure (e.g., purpose, length oftime, radiation dose)2b. pre- and post-treatment orprocedure instructions (e.g.,preparation, diet, andmedications)c. respond to inquiries about otherimaging modalities (e.g., dosedifferences, types of radiation,patient preparation)d. treatment compliance(e.g., positioning, skin marks)4. support servicesa. hospiceb. other professionals(e.g., dietitian, clergy, socialservices)C. Ergonomics and Monitoring1. body mechanics (e.g., balance,alignment, movement)a. patient transfer techniquesb. ergonomic devices (e.g., transferboard, Hoyer lift, gait belt)2. assisting patients with medicalequipmenta. infusion catheters and pumpsb. oxygen delivery systemsc. other (e.g., nasogastric tubes,urinary catheters, tracheostomytubes)3. patient monitoring anddocumentationa. vital signsb. signs and symptoms (e.g., motorcontrol, cognitive changes)c. fall preventiond. weightD. Medical Emergencies1. non-contrast allergic reactions (e.g.,latex)2. cardiac/respiratory arrest(e.g., CPR, AED)3. physical injury or trauma4. other medical disorders(e.g., seizures, diabetic reactions)*The abbreviation “e.g.,” is used to indicate that examplesare listed in parentheses, but that it is not a complete listof all possibilities.(Patient Care continues on the following page.)
RADIATION THERAPY EXAMINATIONCONTENT OUTLINEARRT BOARD APPROVED: JANUARY 2021IMPLEMENTATION DATE: JANUARY 1, 2022Patient Care (continued)E. Infection Control1. chain of infection (cycle of infection)a. pathogenb. reservoirc. portal of exitd. mode of transmission1. directa. dropletb. direct contact2. indirecta. airborneb. vehicle borne (fomite)c. vector borne (mechanical orbiological)e. portal of entryf. susceptible host2. asepsisa. equipment disinfectionb. equipment sterilizationc. medical aseptic techniqued. sterile technique3. CDC Standard Precautionsa. hand hygieneb. use of personal protective equipment(e.g., gloves, gowns, masks)c. safe handling of contaminatedequipment/surfacesd. disposal of contaminated materials1. linens2. needles3. patient supplies4. blood and body fluidse. safe needle practices4. transmission-based precautionsa. contactb. dropletc. airborne5. additional precautionsa. neutropenic precautions (reverseisolation)b. healthcare-associated (nosocomial)infections3F. Handling and Disposal of Toxic orHazardous Material1. types of materialsa. chemicalsb. chemotherapyc. metals (e.g., block alloy)2. safety data sheet (e.g., materialsafety data sheet)G. Pharmacology1. contrast media types and properties(e.g., iodinated, water soluble,barium, ionic versus non-ionic)2. appropriateness of contrast mediato procedurea. patient conditionb. patient age and weightc. laboratory values(e.g., BUN, creatinine, eGFR)3. complications/reactionsa. local effects(e.g., extravasation/infiltration,phlebitis)b. systemic effects1. mild2. moderate3. severec. emergency medicationsd. radiation therapist’s responseand documentation(Patient Care continues on the following page.)
RADIATION THERAPY EXAMINATIONCONTENT OUTLINEARRT BOARD APPROVED: JANUARY 2021IMPLEMENTATION DATE: JANUARY 1, 2022Patient Care (continued)2. Patient and Medical RecordManagementA. Evaluation1. epidemiology and etiologya. cancer risk factorsb. prevalence and incidence2. cancer screening3. signs and symptoms4. history and physical examination5. imaging studies (e.g., CT, MRI, PET/CT)6. other diagnostic studiesa. lab resultsb. surgical reportsc. pathology reportsB. Assessment1. treatment side effectsa. signs and symptomsb. causesc. management2. blood studiesa. types of studies(e.g., CBC, BUN, PSA)b. factors affecting blood values3. dietary counselinga. common problemsb. causesc. dietary managementC. Documentation1. information included in treatmentrecorda. prescriptionb. monitor unitsc. target dose (daily andaccumulated)d. energy and type of radiatione. datef. time of day for b.i.d. treatmentg. fractionh. elapsed daysi. field number and descriptionj. doses to other regions of interestk. set-up instructionsl. imaging orders2. elements of record keepinga. patient identificationb. accountability (e.g., signatures)c. accuracy and legibilityd. variance from prescription(errors, prescription changes)e. medical events (definition andrequired documentation)3. basic charge capture terminology 1a. professional and technicalcomponentsb. general principles and purpose(e.g., billable services,procedures, and devices)14Specific CPT codes are not covered.
ARRT BOARD APPROVED: JANUARY 2021IMPLEMENTATION DATE: JANUARY 1, 2022RADIATION THERAPY EXAMINATIONCONTENT OUTLINESafety1. Radiation Physics and RadiobiologyA. Sources of Radiation1. radioactive material2. machine-produced radiationa. target interactions (i.e.,bremsstrahlung, characteristic)b. particles (e.g., protons)B. Principles of Radiation Physics1. wave characteristics2. attenuation3. inverse-square law4. x-ray beam quality5. interactions with mattera. photon interactions(e.g., Compton, photoelectriceffect, pair production)b. electron interactionsc. particle interactions(e.g., proton, neutron)d. attenuation by various tissuesC. Biological Effects of Radiation1. Units of measurement (NCRP #160)a. absorbed dose (Gy)b. dose equivalent (Sv, rem)c. exposure (C/kg)d. effective dose (Sv, rem)e. air kerma (Gy)2. radiosensitivitya. dose-response relationshipsb. relative tissue radiosensitivities(e.g., LET, RBE)c. oxygen effect3. somatic effectsa. cellsb. tissue (e.g., hemopoietic, skin,reproductive organs)c. embryo and fetusd. carcinogenesis5e. early versus late or acute versuschronicf. deterministic versus stochasticg. short-term versus long-termexposureh. acute radiation syndromes1. hemopoietic2. gastrointestinal (GI)3. central nervous system (CNS)4. genetic effects (e.g., geneticallysignificant dose)D. Radiation Tissue Tolerance1. tolerance levels (i.e., whole organTD5/5)2. adverse effects3. dose to critical structures4. radiobiological factors(e.g., dose, fractionation schemes,volume)5. biological factors(e.g., age, anatomic variation, medicalconditions)6. medical factors(e.g., prior surgery, pacemakers)7. other factors (e.g., radiosensitizers,radioprotectors)8. contribution from other sourcesa. chemotherapyb. brachytherapy 2c. other fields (e.g., prior or abutting)d. radiation effect modifierse. daily imagingf. CT simulationOnly basic concepts related to common uses ofbrachytherapy are covered, including dose to surroundingtissue and radiation protection issues. Specific proceduresand isotope characteristics are not covered.2(Safety continues on the following page.)
RADIATION THERAPY EXAMINATIONCONTENT OUTLINEARRT BOARD APPROVED: JANUARY 2021IMPLEMENTATION DATE: JANUARY 1, 2022Safety (continued)2. Radiation Protection, EquipmentOperation, and Quality AssuranceA. Minimizing Patient Exposure1. exposure factorsa. kVpb. mAs2. shieldinga. rationale for useb. typesc. placement3. collimation/beam width4. patient considerationsa. positioningb. communicationc. pediatricd. morbid obesityB. Personnel Protection (ALARA)1. sources of radiation exposure2. basic methods of protection(i.e., time, distance, shielding)3. personnel monitoring (NCRPrecommendations for personnelmonitoring, Report #116)a. occupational exposureb. public exposurec. embryo/fetus exposured. dose equivalent limitse. evaluation and maintenance ofpersonnel dosimetry recordsC. Facilities and Area Monitoring1. NRC regulations(10 CFR, parts 20 and 35)a. classification of areas (restricted,controlled, unrestricted)b. required postings (signs)c. area monitoring devices2. barrier requirementsa. primaryb. secondary6D. MRI Magnetic Field Screening1. biomedical implants2. ferrous foreign bodies3. medical conditions(e.g., pregnancy)4. prior diagnostic or surgical procedures5. topical or externally applied items(e.g., tattoos, medication patches,body piercing jewelry, monitoringdevices, clothing)6. ancillary equipment (e.g., oxygentank, IV pole)E. Handling and Disposal of RadioactiveMaterialsF. Components and Operation1. linear accelerator2. CT simulatorG. Instrumentation1. ionization chamber2. Geiger-Müller detector3. TLD/OSL (optically stimulatedluminescence)4. diodes5. neutron detectors(Safety continues on the following page.)
RADIATION THERAPY EXAMINATIONCONTENT OUTLINESafety (continued)H. Quality Control Procedures1. warm-up and inspection of linearacceleratorsa. interlock systemsb. safety lightsc. emergency switchesd. laser alignmente. critical machine parameters(e.g., pressure, temperature)f. electrical and mechanical hazardsg. imaging systemsh. audio/visual systems2. warm-up and inspection of CTsimulatorsa. safety lightsb. emergency switchesc. laser alignmentd. QC water phantom (e.g., CTnumber, noise)e. tube warm-up3. radiation output verificationa. methodsb. frequencyc. effect of environment (e.g.,humidity) on measurements4. light and treatment field checksa. light and radiation field agreementb. collimator indicator agreementc. multileaf collimator performanced. sidelight/laser accuracy check(isocenter)5. rotation checka. safety proceduresb. operation of gantry/console6. evaluation of quality assurance resultsa. interpretationb. course of actionc. documentation7ARRT BOARD APPROVED: JANUARY 2021IMPLEMENTATION DATE: JANUARY 1, 2022
RADIATION THERAPY EXAMINATIONCONTENT OUTLINEARRT BOARD APPROVED: JANUARY 2021IMPLEMENTATION DATE: JANUARY 1, 2022Procedures1. Treatment Sites and TumorsA. Anatomy, Pathophysiology, LymphaticDrainage, and Metastatic Patterns1. brain and spinal cord2. head and neck (including thyroid andsalivary glands)3. breast4. lung5. abdomen, pelvis, GI, and GUa. esophagus, stomach, small bowel,large bowel, rectum, and anusb. pancreas, adrenals, liver, andgallbladderc. ureters, kidneys, bladder, and urethra6. reproductivea. prostate, testes, penisb. endometrium, cervix, ovaries, uterus,vagina, and vulva7. skeletal8. miscellaneousa. lymphoma (Hodgkin andnon-Hodgkin)b. sarcomas (bone and soft tissue)c. multiple myelomad. skine. leukemiaf. mycosis fungoidesg. bone marrow transplanth. benign (e.g., heterotopic bone,keloid, AVM, meningioma)i. oncologic emergencies (e.g., wholebrain, SVC, cord compression)B. Tumor Classification1. histopathologic types(e.g., benign, sarcomas, carcinomas)2. histopathologic gradea. purpose (differentiation and growthrate)b. grading system (e.g., GX, G1-G4)3. staging (basic concepts; not specificsites)a. purposeb. systems (e.g., TNM, Ann Arbor)82. Treatment Volume LocalizationA. Treatment Techniques and AnatomicRelationships1. radiation therapy techniques2. sectional and topographic anatomy3. critical organs4. patient positioning andimmobilization5. types and uses of contrast mediaB. CT Simulation1. CT image acquisition (e.g., mA, slicethickness)2. CT image processing and display(e.g., reconstruction, window level,field of view, CT number)3. contour volume and isocenterdetermination4. image transmission, storage, andretrieval5. programmable lasersC. Documentation and Verification ofSimulation Procedure1. implement according to physicianorder2. anatomic position3. equipment orientation4. accessory equipment5. field parameters6. set-up instructions7. set-up photographs8. temporary and/or permanentreference marks(Procedures continues on the following page.)
ARRT BOARD APPROVED: JANUARY 2021IMPLEMENTATION DATE: JANUARY 1, 2022RADIATION THERAPY EXAMINATIONCONTENT OUTLINEProcedures (continued)3. Prescription and DoseCalculationA. Treatment Prescription1. total target dose2. fractionation schedules3. beam energy4. types of radiation5. treatment volume(e.g., GTV, CTV, PTV)6. number of fields7. fixed/rotational fields8. field weighting9. field orientation10. treatment unit capabilities andlimitations11. plan modifications12. beam modifiersB. Geometric Parameters and PatientMeasurements1. field size and shape2. target depth3. patient thickness4. SSD (TSD) and SAD (TAD)5. collimator setting6. abutting fields (e.g., gap calculations)7. fusion with outside diagnostic studiesC. Dose Calculation and Verification1. selection of energy2. equivalent square (open and blockedfield)3. scatter factors (e.g., collimator,phantom)4. depth of maximum equilibrium (dmax)5. percentage depth dose6. TAR, TMR7. SSD (TSD), SAD (TAD)8. inverse square9. extended distance factors10. wedges (e.g., wedge angle or factor)11. off-axis calculation12. isodose curve characteristics(e.g., penumbra, DVH)13. factors for beam modifiers(e.g., tray factor, bolus, compensator)14. inhomogeneity correction factors15. machine output data16. verification and documentation94. TreatmentsA. Treatment Options (indications,benefits, risks)1. chemotherapy2. surgery3. radiation therapya. external beam (e.g., photon,electron)b. brachytherapy 24. multimodality treatmentB. Verification and Application of theTreatment Plan1. patient position2. isocenter location and shifts3. treatment parameters(e.g., beam orientation, energy)4. prescription5. techniquesa. 2Db. 3Dc. non-volumetric arc therapyd. 4D (e.g., respiratory gating)e. IMRTf. volumetric arc therapyg. stereotactic6. imaging proceduresa. kV imagingb. cone beam CT (CBCT)c. MV imagingOnly basic concepts related to common uses ofbrachytherapy are covered, including dose to surroundingtissue and radiation protection issues. Specific proceduresand isotope characteristics are not covered.2(Procedures continues on the following page.)
RADIATION THERAPY EXAMINATIONCONTENT OUTLINEARRT BOARD APPROVED: JANUARY 2021IMPLEMENTATION DATE: JANUARY 1, 2022Procedures (continued)C. Treatment Machine Set-Up1. auxiliary set-up devicesa. couch indexingb. positioning aidsc. alignment lasersd. motion management1. surface guided radiation therapy(SGRT)2. gating systems3. abdominal compression2. machine operationsa. collimator or cone settingsb. optical or mechanical distanceindicatorc. gantry angled. collimator anglee. field lightf. treatment couchg. six degrees of freedom couchh. console controlsi. pendant controls3. parametersa. SSD (TSD), SAD (TAD), depthb. gantry, collimator, and field sizesettingsc. beam energy and typeD. Treatment Accessories1. beam modifiersa. compensating filtersb. shieldingc. blocks (e.g., thickness, half valuelayer (HVL), half-value thickness(HVT))d. multileaf collimatione. bolusf. wedges (enhanced dynamicwedge, physical wedge)2. immobilization devicesa. customb. standard10E. Treatment Administration1. patient monitoringa. visualb. audioc. back-up systemsd. monitoring regulationse. emergency situations2. record and verify systems3. image acquisition and registration4. site verification5. dose verification (e.g., diodes)6. equipment malfunctionsa. types (e.g., radiation, electrical,mechanical, software)b. troubleshooting and correctionc. documentation and reportingV 2021.02.25
Radiation Therapy . The purpose of the radiation therapy exam is to assess the knowledge and cognitive skills . radiation therapist's response 1. linens . and documentation . 2. needles . 3. patient supplies (Patient Care continues on the followingpage.) 4. blood and body fluids .