Transcription
ScarmanagementSupported byAccredited by the RCNCentre for ProfessionalAccreditation until 11 May2013. Accreditation appliesonly to the educationalcontent and not to anyproduct.
scar MANAGEMENTForewordScars pose a significant concern to individuals and can have a profoundeffect on their lives, functionally and aesthetically, particularly when highlyvisible. An increased awareness of this area is important for healthcareprofessionals to ensure appropriate care in the prevention, assessmentand differential diagnosis, management and maintenance of scars.This handbook offers an overview of the categories of scars includingkeloid, hypertrophic, stretch marks and acne scars and their assessment witha range of supporting images.The recognition of scars using the acronym SCAR is useful for the healthcare professional to consider important aspects of assessment and management. Site, Category, Ageand Reassurance and the aide memoir is helpful in ensuring all issues are considered.The psychological effects of scarring can be significant, and helping patients adjust in apositive way can have a profound effect. An important aspect of this is the size of the scar,which, as the evidence identifies, bears little relevance to the impact on the individual. This isan important message and may be underestimated by healthcare professionals.The Nursing in Practice online staff survey of 251 primary care nurses offers an insight intoboth the classification of scars seen and also the treatments currently recommended. Importantly, 67% of the respondents always discuss care and treatment of scars with patients, and89% discuss the best methods of improving scar appearance. However, a third of the respondents identified a need to improve their own knowledge to improve outcomes for the patient.The management of scars is an important role for all healthcare professionals to consider,and where possible offer accurate assessment, differential diagnosis and evidence-basedcare to maintain aesthetics and function. Where improvement cannot be achieved, adviceon maintenance – including the consideration of camouflage and micro-pigmentation – canbe given.Increased knowledge about scars can ensure that healthcare professionals offerappropriate advice and can ensure that those who need access to a member of themulti-disciplinary team receive it. The role of dispelling myths about scarring and spuriousclaims regarding inappropriate treatments should form part of the healthcare professional’srole in caring for those with a scar.This handbook offers an extremely useful overview of the evidence regarding scarmanagement and I urge healthcare professionals to increase their knowledge and improveoutcomes for patients.By Jackie Stephen-Haynes, Professor in Tissue Viability,Professional Development Unit, Birmingham City Universityand Consultant Nurse, Worcestershire Health and Care NHS TrustScar Handbook
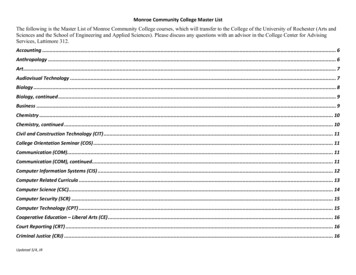
scar MANAGEMENTContentsContents1. Scar recognition and assessment042. THE PSyCHOLOGICAL EFFECTS OF SCARRING103. The NIP/Bio-Oil Survey: the results164. SCAR TREATMENT20Scar Handbook
scar MANAGEMENTChapter 1 Scar recognitionScar recognitionand assessmentScarring has been defined as the macroscopic disturbance of the normalstructure and function of skin architecture, resulting from the end productof a healed wound.1 In other words, scar tissue does not look the same asundamaged skin/tissue. This can cause great distress to individuals,particularly when the area affected is highly visible, the face being the mostobvious.2 This may be regardless of whether the scar is acne-related, largesurgical scarring or trauma-related. Carr et al reported that 67% of womenand 33% of men in the UK were concerned about a scar on their body.3 Self-esteem andconfidence can be seriously affected, in some instances leading to self-imposed isolation.In addition, scars over joints may inhibit movement and may even lead to disability, causingpossible financial hardship in addition to emotional distress.4Wound healingWound healing comprises several overlapping phases: haemostasis, inflammation, destruction, proliferation, re-epithelialisation and finally maturation and remodelling; the latter stagefinally producing the scar tissue. During the later stages of wound healing, all devitalised tissuehas been removed from the wound bed and the defect is filled with granulation or connectivetissue. This is produced by fibroblast cells, whose main task is the synthesis of collagen fibres.These fibres produce keratinocytes, whose function is to balance the removal of old collagenand produce new collagen until the wound defect is healed and the scar produced. If thisprocess produces too much collagen, increased scarring results. If too little is produced, thescar tissue is weak and easily ruptured.5 The scar tissue gradually increases in tensile strength,however this will be at best 70% of its original strength and so vulnerable to injury.6 Initially, thenewly healed wound scar will be livid in colour, gradually during the course of a year, the scarwill become avascular and take on the classical non-pigmented appearance.Normal scarringNormal linear scarScars vary in appearance, usually dependant on the type of injury or surgical procedure, andalso on the type and position of the wound area, race and age.7 Surgical wounds with goodapproximation of the wound edges by suture, staples or glue will heal with minimal scarringand produce a linear scar.84Scar Handbook
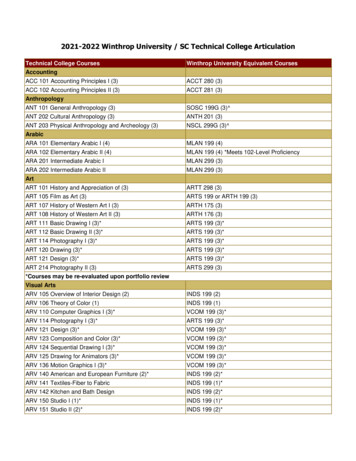
Scar recognition Chapter 1Scars can be divided into the following types:Keloid – grow beyond the boundary of theoriginal wound site, due to an imbalance inthe production of collagen protein.Hypertrophic – raised and red but do notexceed the boundaries of the original woundsite. They can continue to thicken for up tosix months and can be itchy or painful.Contracture scars – causes tighteningof the skin and may cause discomfort oraffect movement. Contracture scars areoften a result of burns.Linear – a minimal scar that occursfollowing surgery where there is goodapproximation of the wound edges bysuture, staples or glue.Atrophic – raised and red but do notexceed the boundaries of the originalwound site. They can continue to thickenfor up to six months and can be veryitchy or painful.Stretch marks – when the skin isstretched rapidly (during pregnancy,weight gain or loss, or adolescent growthspurts) or when skin is put under tensionduring the healing process.Acne scars – a scar that occurs whenthe wound tries to heal itself resultingin too much collagen in one area. Thesescars may be referred to as ‘ice pick’,‘box car’ or ‘rolling’ scars.Superficial dermal scarFigure 1 shows a newly healed donor site wound, fromwhich a split skin graft had been harvested. The resultantwound is very superficial and heals by re-epithelialising,usually within 10-14 days. Once healed, this requires gentlewashing as usual. Pat dry and apply a moisturisingemollient such a basic 50:50 liquid in white soft paraffin,applied sparingly twice a day until the donor site has a dryappearance.Figure 1.Stretched scar resulting from a wound healing bysecondary intentionIf wound healing is delayed by infection or the woundis over a joint that cannot be immobilised, mechanical forcemay result in a stretched scar appearance. Stretched scarscan also be the result of too little collagen deposition in latterstages of wound healing, often caused by malnutrition.4Hypertrophic scarHypertrophic scars are formations of excess scar tissueabove the level of the surrounding skin and often presentFigure 2. A stretched scar.Scar Handbook5
scar MANAGEMENTChapter 1 Scar recognitionFigure 3. Hypertrophic scar in a sternotomy incision. Figure 4. Keloid scar peri umbilicus.as raised, angry, painful/itchy scars, which maintain vascularity and therefore lividity.9Hypertrophic scars remain within the original wound area and usually develop 6-8 weeksafter the epithelialisation is complete. These scars occur more frequently in wounds crossinglines of tension such as over the sternum, upper back and major joints.10 The cause ofhypertrophic scars is the over-production of disorganised collagen fibres. Hypertrophic scarringresolves spontaneously, but can cause distress to the individual. There are many silicone geland sheet products available, which are thought to aid resolution of hypertrophic scarring byincreasing the scar temperature and increasing the rate of collagen breakdown.11 Massage isrecommended for any wound scarring and should commence as soon as epithelialisation iscomplete – a small amount is massaged against the scar with sufficient pressure to blanchthe scar tissue.12Keloid scarKeloid scars result from over-production of collagen fibres – up to 20 times more than normalscars – and can occur any time after wound healing.7 Keloid scars are particularly prevalentin Afro-Carribean and Asian races, and are thought to have a genetic predisposition, whileCaucasian races may also develop keloid scarring in rare cases. Unlike hypertrophicscarring, the keloid does not remain within the boundaries of the original wound site butextend into previously undamaged skin and tissue.7 Keloid scars often develop in burninjuries but can also be caused by tattoos, injection sites, skin reactions and surgery.10Keloids scars do not settle spontaneously, and excision surgery may exacerbate theproblem. Treatment concentrates on prevention by use of pressure garments and massage,as previously described.106Scar Handbook
Scar recognition Chapter 1References1.Ferguson MJW, Whitby DJ, Shah M, et al. Scar formation, the spectral nature of fetal andadult wound repair. Plastic Reconstructive Surgery 1996;97(4):854-60.2. Edwards J. The use of silicone gel in hypertrophic scar management. Journal CommunityNursing 2005;19(2):18-20.3. Carr T, Harris D, James C. The Derriford Appearance Scale (DAS-59); a new scale to measureindividual responses to living with problems of appearance. British Journal of HealthPsychology 2000;5(2):201-15.4. Benbow M. Minimising scarring. Practice Nurse 2006:32(4):53-8.5. Waldrop J, Doughty D. Wound healing physiology. In: Acute and Chronic wounds; nursingmanagement. Mosby, St Louis, USA: Ed Bryant RA; 2000.6. Levenson S, Geever E, Crowley L, Oates J, Berard C, Rosen H. The healing of rat skinwounds. Annals Surgery 1965;161:293-7; 11(8):296-9.7. O’Kane S. Wound remodelling and scarring. Journal Wound Care 2002.8. Bale S, Jones V. Assessing the normal and abnormal. Wound Care Nursing; a patient centredapproach. London: Bailiere Tindall; 1997.9. Eisenbeiss W, Peter FW, Bakhtieri C, Frenz C. Hypertrophic scars and keloids. Journal WoundCare 1998;7(5):255-7.10. Smith FR. Causes of and treatment options for abnormal scar tissue. Journal Wound Care2005;14(2):49-52.11. Musgrave Ma, Umraw N, Fish JS, Gomez M, Cartotto RC. The effect of silicone gel sheets onperfusion of hypertrophic burns scars. Journal Burn Care & Rehabilitation 2002;23(3):208-14.12. Katz B. Silastic gel sheeting is found to be effective in scar therapy. Cosmetic Dermatology1992. June: 32-3.Author: Pauline Beldon PGDipl. Tissue Repair and Wound Healing.Tissue Viability Nurse Consultant.Epsom and St Helier University Hospitals NHS Trust.Scar Handbook7
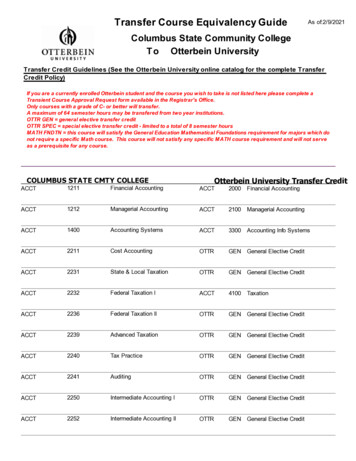
scar MANAGEMENTChapter 1 Scar recognitionScar TreatmentBio-Oil has developed a scar assessment tool to help you identify the type of scarand offer appropriate advice and treatment.S – S ite & Skin type – identify whether scar is on a mobility area, and if the patient’sskin type is likely to produce abnormal or worse scarring.C – Category – is it a keloid, hypertropic, atrophic or contracture scar?A – Age – is the scar new, still maturing or fully matured?R – Reassure & Recommend – reassure patient of commonness of scarring to helpalleviate psychological worry. Recommend treatment options.Site & Skin typeSite – scars on high-mobility areas such as joints can restrict movement as thetissue can tighten. In such cases it will help to massage with a moisturisingproduct to maintain elasticity as the scar matures.Scars heal differently on different areas of the body. Typically the face and neck willproduce better scars than areas such as the tip of shoulders, earlobes and middle of thechest, which can on rare occasions produce keloid scars.Skin Type – darker skin types (particularly Afro-Caribbean and Asian skin) are susceptibleto keloid scarring, where there is an overgrowth of dense fibrous tissue outside of theboundary of the wound. Fair, freckled skin types tend to scar more than other skin types.CategoryThere are four different categories of scar that each heal and matureslightly differently:Keloid scars – grow beyond the boundary of the original wound site, due to an imbalancein the production of collagen protein.Hypertrophic scars – raised and red but do not exceed the boundaries of the original woundsite. They can continue to thicken for up to six months and can be very itchy or painful.Contracture scars – causes tightening of the skin and may cause discomfort or affectmovement. Contracture scars are often a result of burns.Atrophic – typically small, flat or depressed relative to the surrounding skin and oftencaused by acne where collagen is destroyed within the dermis where the cysts occured.Skin can be dryer and less elastic.Stretch marks (striae) – streaky lines on the surface of the skin in areas where skin has8Scar Handbook
Scar recognition Chapter 1stretched during pregnancy or rapid growth such as the abdomen, breasts and hips. Newstretch marks will be red or purple in appearance, while mature stretch marks will be silveryor white.AgeAge of scar – young scars (typically less than 6-9 months since the wound healed)will present red and possibly raised. Young scars are still maturing so it is importantto reassure the patient that the colour will fade over time. Older scars will be faded and pale.Age of patient – both keloid and hypertrophic scarring are more common in younger(typically 10-30 years old) patients with darker skin.Reassure & RecommendReassure – whilst scars do not always present a medical issue, they can have apsychological impact on the patient. So where a patient has aesthetic concerns,reassure that scars are extremely common (on average each person has three scars on theirface or body). For new scars you can reassure that the scar will continue to mature andimprove for up to two years.Maintain elasticity – for scars on mobility areas or those causing discomfort, skin shouldbe kept supple, with regular application of a topical oil or cream.Self-care – nothing can completely remove a scar; however, applying a topical oil or creamcan help to improve skin condition and empower the patient to connect with the scar andfeel more positive.Refer – for cases of severe or abnormal scarring (eg, keloid) where the scar is causingphysical pain or severe mental distress it may be necessary to refer to a dermatologist orplastic surgeon to discuss further treatment options, including corticosteroid injections orsurgical procedures. In cases of severe scarring, there are several support groups thepatient may find helpful. These include Changing Faces, British Association of SkinCamouflage, The Scar Information Service and Burned Children’s age.cfm?ID e.nhs.uk/pip admin/docs/keloid scars 339.pdfScar Handbook9
scar MANAGEMENTChapter 2 The psychological effects of scarringThe psychological effectsof scarringWhile there is a plethora of information about scarring, theprocesses remain poorly understood and there appears to belittle universal agreement on its clinical definition. Scars maycause psychological, functional or growth problems. Thepsychological effects that a scar has on the person and thespecific issues that may affect patients with scars from acne,stretch marks (striae), post-operative scars and burn scars willbe discussed in this article. Patients will have to live with the effects of scars and therefore it ishelpful to think about this from a patient’s perspective.1 It is also acknowledged that thesupport a patient receives from healthcare professionals is to enable them to adjust in apositive way to their scars.2 Therefore this chapter will also explore ways in which the nurse canhelp the patients come to terms with a scar, giving practical examples as appropriate.Body ImageWestern society places a lot of importance on how we look. Rumsey and Harcourt state thatthe literature suggests there is a relationship between appearance and self-concept, with avisible disfigurement leading to lowered self-confidence.3 This lowered self-confidence canaffect all areas of the patient’s life, such as when forming relationships or receiving negativereactions from others.4Before addressing how the nurse may help patients to adapt from a psychological perspective, it is helpful to first look at why these types of scars may give rise to psychological problems.Acne is common in adolescents with over 80% of teenagers in both sexes having beenaffected by the age of 20.5 The onset of puberty can increase body image concerns andemotional stress can exacerbate acne.2,6-7 Patients with acne also suffer from self-esteemissues and feel embarrassed about their condition.7 Acne is often found on the face anddisfigurements to the face may cause more problems because of the connection betweenthe face and self.8 Aktan et al found that although boys appeared to have more severe acne,girls appeared to have greater anxiety.7 However, Smithard et al found that there was nodifference in the anxiety levels of boys and girls, and concluded that both sexes should betreated the same.5 One possibility for the differences found in the two studies could be thatfemales’ coping strategies involve talking about their concerns more than males.5 There are10Scar Handbook
The psychological effects of scarring Chapter 2also many inaccuracies regarding the causes of acne, and the nurse should dispel mythssuch as causation of acne through lack of face-washing or poor diet, etc.9Striae or stretchmarks are thought to occur in about 50% of pregnant women, althoughthis condition is not restricted to pregnant women.10,11 The key here is to be aware that theexact mechanism of occurrence – or why striae occur in some and not others – is notunderstood.11 This means that it is difficult to predict who will have striae. There is someevidence that younger women and those with a family history are more likely to developstretch marks.12 A Cochrane review did not find any evidence that using various creamsprevented striae.10 However, NHS Choices advises avoiding rapid weight gain, and suggeststhat a healthy diet and daily massage with a moisturiser can help reduce the risk ofdeveloping stretch marks.13 Although striae tend to occur on the abdomen, hips and breastsand can be hidden by clothing, they could cause embarrassment when going swimming orin changing rooms. When striae is particularly severe it can cause severe itching anddiscomfort.14 Striae are also a feature of Cushing’s disease, and high doses of steroid therapyhave been known to induce the condition.11Post-operative scars are better understood, and occur as a direct result of surgery. Withplanned surgery there is time to discuss scarring. The nurse should have an understandingof the healing process. This is because when the wound has epithelialised there is still afurther stage of wound healing, that of maturation.15 This takes a period of about 12-18months (post-epithelialisation) when the scar starts to settle down. Collagen becomesreorganised and the initial lumpiness of the scar eventually goes. The extra blood supply(from angiogenesis) also goes back to normal and the scar will pale.15 The nurse needs tospend time with patients, ensuring that they are aware of the likely course of events in termsof scar formation. For example, if a lump is being removed they need to be aware of thedepth of the lump and that there may be a ‘dent’ in the skin from where the lump has beenremoved. Using pictures from previous patients may help them to appreciate the amount ofscarring.16 Young and Hutchinson also found that patients are extremely concerned aboutscarring after routine surgery.17Burn scars differ from post-operative scars in that they are likely to be larger and mayhypertrophy (see Edwards for further information on hypertrophic scars18). Burns also have anelement of trauma for the patient. Patients may wish to talk about how the accident happenedand relive the event as a way of coming to terms with it. The nurse should make time to listento the patients’ concerns.Helping patients come to terms with a scarOther people’s reactions influence body image,2 therefore the nurse needs to be aware ofhow he/she approaches the patient regarding their scar as patients may pick up both verbalScar Handbook11
scar MANAGEMENTChapter 2 The psychological effects of scarringand non-verbal communication. This is extremely important when the scars are unpleasantor on obvious places of the body such as the face.16 Feedback may help to reassure patientsand might start the formation of a trusting relationship, which will allow patients to talk tonurses regarding their feelings about the scar.The size of the scar should not matter. A small survey undertaken by the Scar InformationService found that the majority of patients who were concerned about their scars had smallscars.16 The survey found that patients with smaller scars perceived healthcare professionalsto be less sympathetic to them, giving more sympathy to those with large scars. Young andHutchinson also found that the size of the scar did not alter patients’ concerns.16 Thereforethe nurse must not make the patient feel their concerns are trivial.The literature appears to focus on visible scars.20-22 The author believes that all scars arevisible, but some are easier to hide than others, through use of clothing for example. Whatmay be more important is thesignificance of the area affectedto the patient and that should bediscussed.2 The more significantthe area, the more support willbe needed.Many patients complain ofpruritis (itchy skin) from the scars.The exact cause does not appearto be known but massaging thescar with a little moisturiser mayhelp.23 If the itchiness is severethen antihistamine tablets couldbe prescribed.It is fairly common for scarsto be massaged to improve thecosmetic appearance.23-24Massage may disrupt the fibrotictissue and increase the pliabilityof the scar, but the exactmechanism of how it worksappears to be unknown.24However, Shin and Bordeauxfound that the evidence tosupport the use of massagewas inconclusive.24 Even so,they support its use, saying thatit is ‘anecdotally effective’ and12Scar Handbook
The psychological effects of scarring Chapter 2appears to be more effective with post-operative scars than any other type. In fact, massagemay also have other psychological benefits as patients may find this relaxing. Patients maybe concerned about what to use as a moisturiser when massaging scars. There is noevidence in the literature to suggest that any cream or oil was better than another, but theuse of a moisturiser prevents damage from friction while massaging.If the scar is hypertrophic then using silicone gel sheets over the scar may help to reducethe scar, although the exact mechanism of action is still unknown even though it has been inuse for more than 20 years.25,26 If silicone gel is to be used, the patient should increase weartime slowly until they can tolerate eight hours or more.27Coping strategiesBefore coming to terms with a disfigurement it appears that most patients go through a stageof mourning the loss of how they used to look before accepting their new self.2,8 Throughoutthe grieving process the patient will need someone to listen and encourage them to talk abouttheir feelings. The importance of listening to the patients’ worries cannot be overstated.Other coping strategies may include direct approaches, such as talking about issues.That way it is possible to find out what the issues are to the patient and then practicalsuggestions can be offered. If the scar concerns the patient so much, they can be referred toa plastic surgeon, who may be able to make the scar less noticeable,16 or it may be possibleto arrange for the patient to have cosmetic camouflage to hide the scar.On a more practical note, the patient could gently massage the scar twice daily using amoisturiser or oil. Although the evidence to support massage is inconclusive,24 it does givesome control back to the patient and, as well as helping to disrupt the fibrotic tissue, mayalso help to control some of the itching.If patients start to have difficulties interacting with others due to their scars, they maybenefit from social-skills training specifically for people with disfigurements.3 Bessel andMoss found the evidence for this was poor, but it may prove helpful for some patients.28Support NetworkA good social support network is a way of helping people deal with any stress.2,3 It isimportant that the nurse also discusses the impact of scars with the patient’s relatives/friends (with the patient’s permission). If those relatives also have difficulty coming to termswith how the person looks then this may be a starting point for them to discuss their feelings.ConclusionIn order to be able to deal effectively with patients who have scars, the nurse needs to havean understanding of the causes of scarring. It should be noted that the size of the scar is oflittle importance compared with the patient’s perception of the scar. It is also important thatnurses are sufficiently well informed to be able to dispel popular myths around the causesand prevention of scars. The key issue, however, is simply to make time to talk to the patient.Scar Handbook13
scar MANAGEMENTChapter 2 The psychological effects of .15.16.17.18.19.14Magnan M. Psychological considerations for patients with acute wounds. Critical Care NursingClinics of North America 1996;8:183-93.Price B. Body Image: Nursing concepts and care. New York: Prentice Hall; 1990.Rumsey N, Harcourt D. Body image and disfigurement: issues and interventions. Body Image2004;1:83-97.Thompson A, Kent G. Adjusting to disfigurement: processes involved in dealing with beingvisibly different. Clinical Psychology Review 2001;(21):663-82.Smithard A, Glazebrook C, Williams H. Acne prevalence, knowledge about acne andpsychological morbidity in mid-adolescence: a community based study. British Journal ofDermatology 2001;145:274-79.Croll J. Body image and adolescents in Story S, ed. Guidelines for adolescent nutrition services2005. Online at: www.epi.umn.edu/let/pubs/img/adol ch13.pdf (accessed: 12.2.2012)Aktan S, Ozmen E, Sanli B. Anxiety, depression, and nature of acne vulgaris in adolescents (areport). International Journal of Dermatology 2000;39:354-7.Drench M. Changes in body image secondary to disease and injury. Rehabilitation Nursing1994;19:31-6.Magin P, Adams J, Heading G, Pond D, Smith W. The causes of acne: a qualitative study ofpatient perceptions of acne causation and their implications for acne care. DermatologyNursing 2006;18:344-70.Young G, Jewell D. Creams for preventing stretch marks in pregnancy (review). The CochraneCollaboration: Wiley: 2010. Online at: 8.CD000066/pdf (Accessed 12.2.2012)Elsaie M, Baumann L, Elsaaiee L. Striae distensae (stretch marks) and different modalities oftherapy: an update. Dermatol Surg 2009;35:563-73.Osman H, Rubeiz N, Tamim H, Nassar AH. Risk factors for the development of striaegravidarum. Am J Obstet Gynecol 2007;196(1):62.e1-62.e5.NHS Choices. Stretch marks – Prevention. Available at: n.aspxChang A, Agredano Y, Kimball A. Risk factors associated with striae gravidarum. J Am AcadDermatol 2004;51:881-5.Flanagan M. Physiology of wound healing. Journal of Wound Care 2000;9:299-300.Atkinson, A. Body image considerations in patients with wounds. Journal of CommunityNursing 2002;16:32-6.Young V, Hutchison J. Insights into patients and clinician concerns about scar appearance.Plastic and Reconstructive Surgery 2009;124:256-65.Edwards J. Scar Management. Journal of Community Nursing 2002;16:24-9.Scar Information Service. Scarring: a research report into keloid and hypertrophic scarring.London: Smith and Nephew; 1999.Scar Handbook
The psychological effects of scarring Chapter 220. Tebble N, Thomas D, Price P. Anxiety and self-consciousness in patients with minor faciallacerations. Journal of Advanced Nursing 2004;47:417-26.21. Rumsey N, Clarke A, White P, Wyn-Williams M, Garlick W. Altered body image: appearance-relatedconcerns of people with visible disfigurement. Journal of Advanced Nursing 2004;48:443-53.22. Valente S. Visual disfigurement and depression. Plastic Surgical Nursing 2009;29:10-6.23. Roques C. Massage applied to scars. Wound Repair and Regen 2002;10:126-8.24. Shin T, Bordeaux J. The role of massage in scar management: a literature review. DermatolSurg 2011. Doi: 10.1111/j.1524-4725.2011.02201.x online at: 4725.2011.02201.x/pdf (accessed 12.2.2012)25. Gold M, Foster T, Adair M, Burlison K, Lewis T. Prevention of hypertrophic scars and keloidsby the prophylactic use of topical gel silicone sheets following a surgical procedure in an officesetting. Dermatol Surg 2001;27:641-4.26. Musgrave M, Umraw N, Fish J, Gomez M, Carlotto R. The effect of silicone gel sheets onperfusion of hypertrophic burn scars. Journal of Burn Care and Rehabilitation 2002;23:208-14.27. Fette A. Influence of silicone on abnormal scarring. Plas
scar tissue is weak and easily ruptured. 5 The scar tissue gradually increases in tensile strength, however this will be at best 70% of its original strength and so vulnerable to injury. 6 Initially, the newly healed wound scar will be livid in colour, gradually during the course of a year, the scar