Transcription
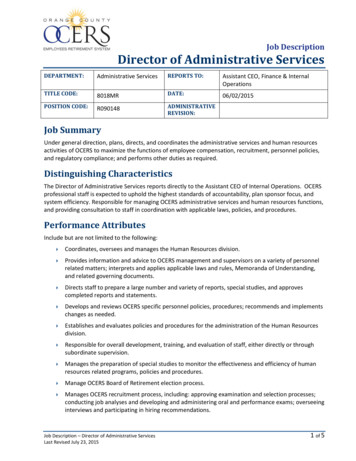
ADMINISTRATIVE OPERATIONSSUMMARY OF CHANGES139ADMINISTRATIVE OVERVIEW140HOW TO GET A CLAIM PAIDVerifying an MBHP/HNE Member's Eligibility141Submitting a Complete and Accurate Claim FormService Facility Address Required on All ClaimsThird Party Liability (TPL) Claims141142142FORMSAdjustment-Reversal FormClaim Review FormThird Party Liability FormTimely Filing Waiver FormWebsite Registration FormAPPENDIXBenefit Service Grid
Summary of Changes:Administrative OperationsAlert #Alert TitleLocation ofInformationDate MailedDate Posted inProvider Manual139
ADMINISTRATIVE OPERATIONS OVERVIEWIn the Administrative Operations Section of this manual, you will find information regardingMember eligibility, claims policies and procedures, instructions on how to submit a claim, andinformation regarding Member appeals.To ensure that you have the most up-to-date information, the Massachusetts Behavioral HealthPartnership/Health New England Be Healthy (MBHP/HNE BH) will notify providers about anychanges in its policies via Provider Alerts. It is important to note that the Provider Manual andall MBHP/HNE BH Provider Alerts are considered part of the Provider Agreement, and as such,requires providers to adhere to all changes outlined in them.Please refer to the information in the Administrative Section of this manual if you have anyclaims-related questions. For additional assistance, please contact the MBHP/HNE BHCommunity Relations Department at 1-800-495-0086 (press 3, then 1 to skip prompts.)140
HOW TO GET A CLAIM PAIDMBHP/HNE BH appreciates the valuable service that our providers perform to our Members, sowe strive to pay all appropriate claims as quickly and accurately as possible. This section is setup to help you get your claims paid as quickly and accurately as possible.Verifying an MBHP/HNE BH Member’s EligibilityIn order to be eligible for reimbursement for MBHP/HNE BH services, providers must verifythe Member’s eligibility and participation in MBHP/HNE BH through the EligibilityVerification System (EVS) on the day the service is provided and for each date of service.However, this is solely for eligibility and is not a guarantee of payment.MBHP/HNE BH recommends that providers check for possible MassHealth and/or MBHP/HNEBH eligibility for each individual who seeks care. An individual may have applied forMassHealth previously and may not be aware that his or her coverage was approved. Verifyingthe available coverage affords a provider the opportunity to complete all necessary MBHP/HNEBH authorization procedures and prevents unnecessary claim denials.Emergency Service Program (ESP) providers are also responsible for verifying Membereligibility and should continue to use EVS for eligibility information.For more information on checking a Member’s eligibility, please visit MassHealth’s web site at:www.mass.gov/MassHealthSubmitting a Complete and Accurate Claim FormClaims Mailing Address:MBHP/HNE BH ClaimsP.O. Box 55871Boston, MA 02205-5871The second step in getting a claim paid is to submit a complete and accurate claim. Please referto our Online Benefit Grid at www.masspartnership.com by clicking the “HNE Be Healthy”button on the left and then clicking “HNE Provider Manual.”This grid explains which codes and modifiers should be used with which services, as well aswhether or not a service requires an authorization.For information on submitting electronic claims, please visit our web .aspx?lnkId emc.ascx&imgID Prov ElectronicClaims.jpg141
Service Facility Address Required on All ClaimsAll paper and electronic claims must have the Service Facility Address completed with theappropriate MBHP/HNE BH-contracted site for that particular service for all Places of Service.For Places of Service 12 (Home) and 03 (School), use the contracted facility address where theprovider of the service normally provides the service when not at a Member’s home or school.Claims without a contracted MBHP/HNE BH facility address in the appropriate place risk beingunnecessarily suspended and/or denied. The information below is to help providers understandhow to submit the Service Facility Address on their claims to MBHP/HNE BH.Electronic claimsThe Service Facility Address should be in Loop 2310D for 837P (Professional) claims and inLoop 2310E for 837I (Institutional) claims.Paper claims On the CMS-1500o The Service Facility Address should be Box 32. On the UB-04 (CMS 1450)o The Service Facility Address should be in FL01.Third Party Liability (TPL) ClaimsThird Party Liability (TPL) claimsProviders must exhaust all avenues of other insurance coverage and payment prior to billingMBHP, on behalf of HNE Be Healthy. If a Member indicates that he or she is covered by a thirdparty insurer and EVS indicates they are enrolled in HNE Be Healthy, it is the provider'sresponsibility to obtain reimbursement from the third party insurer and notify HNE Be Healthyof the active third party coverage by completing the Third Party Liability form located in theforms section of this manual.Please mail this form to:MBHP/HNE-TPL UnitP. O. Box 55871Boston, MA 02205-5871If there is a possibility that the provider will not receive complete reimbursement from the thirdparty insurer, it is the provider’s responsibility to follow MBHP/HNE BH’s ServiceAuthorization procedures outlined in the Clinical section of this Provider Manual to obtain anauthorization for any service that requires one.Providers must bill the third party insurer prior to billing MBHP/HNE BH. When the providerreceives the Explanation of Benefits (EOB) from the third party insurer, they must send a copyof it along with their claim to MBHP/HNE BH. Claims involving TPL must be submitted within60 days of the date on the third party insurer’s EOB, including MassHealth EOBs. EOBs142
reflecting a timely filing denial from the third party insurer or MassHealth will also be denied fortimely filing by MBHP/HNE BH.All claims have specific time frames in which they have to be submitted to MBHP/HNE BH forpayment.Time limits for filing claimsOutpatient Covered Service and Emergency Service Program (ESP) claims must be submittedwithin 60 days of the date of service to be considered for reimbursement; all claims submittedafter 60 days will be denied.Inpatient and Diversionary Covered Service claims must be submitted within 60 days of thedischarge date to be considered for reimbursement; all claims submitted after 60 days will bedenied. Interim billing on MBHP/HNE BH Inpatient and Diversionary Covered Service claimsis allowed, but the claims must be submitted within 60 days from the last date billed on theclaim.The claim must be physically or electronically delivered to MBHP/HNE BH by the close ofbusiness on day 60, NOT just postmarked by day 60.Timely filing waiver processMBHP/HNE BH has determined that the following reasons justify a waiver of the 60-day timelimit for claims submissions. Other reasons may be considered on a case-by-case basis.Retroactive Member Eligibility:If MassHealth enrolls a Member with MBHP/HNE BH on a retroactive basis, the Timely FilingWaiver Unit will approve waiver requests submitted within 60 days of the EVS change. Pleasebe advised that retroactive MassHealth eligibility does not generally indicate retroactiveMBHP/HNE BH eligibility. Due to MassHealth eligibility restrictions, if a Member isretroactively enrolled in MassHealth and receives MBHP/HNE BH, the Member’s MBHP/HNEBH effective date is usually the day that the enrollment information is changed in EVS.Retroactive Clinical Authorization for Service:If MBHP/HNE BH’s Clinical Department authorizes service on a retroactive basis, the TimelyFiling Waiver Unit will approve waiver requests submitted within 60 days of the approval date.A copy of the approval letter must accompany the waiver request. To apply for a Timely FilingWaiver, the provider must complete a Timely Filing Waiver form, found in the Forms area ofthis section, for each original claim being submitted. Claims may be grouped together by reason,and only one form would need to be submitted.All the Timely Filing Waiver Request form items listed below are required. Incomplete formswill be returned.Provider nameEnter the name of the provider that rendered the service and is seeking reimbursement.143
Provider numberEnter the provider’s Medicaid number.Provider addressEnter the address of the provider seeking reimbursement.Member nameEnter the Member’s name as it appears on the MassHealth card or claim form.One waiver form can be submitted for multiple Members if the waiver request has the samereason for all claims entered in field # 8. In this instance, “multiple” should be entered in theMember Name field.Member numberEnter the ID number as it appears on the MassHealth card or claim form.One waiver form can be submitted for multiple Members if the waiver request has the samereason for all claims entered in field # 8. In this instance, “multiple” should be entered in theMember Number field.Date of serviceEnter the date(s) of service.One waiver form can be submitted for multiple dates of service if the waiver request has thesame reason for all claims entered in field # 8. In this instance, “multiple” should be entered inthe Date of Service field.Original claim numberEnter the claim’s original claim number found on the Summary Voucher. In addition, indicatewhether the original claim was timely filed by placing an “X” in the Yes or No box. One waiverform can be submitted for multiple claims if the waiver request has the same reason for allclaims entered in field # 8. In this instance, “multiple” should be entered in the Original ClaimNumber field.ReasonPlace an “X” on the line that best describes the reason for requesting the timeliness waiver.SignatureThe waiver request cannot be processed without a typed, signed, stamped, or computer-generatedsignature. MBHP/HNE BH will not accept “SIGNATURE ON FILE” as an acceptable providersignature.DateIndicate the date that the form is completed.Send the completed Timely Filing Waiver form and completed claim forms along with anysupporting documentation to justify the waiver of the 60-day time limit to:144
MBHP/HNE BH -Timely Filing Waiver UnitP. O. Box 55871Boston, MA 02205-5871All Timely Filing Waiver Requests will be reviewed to determine the appropriateness of therequest. The waiver request will either be approved or denied. The approval of a waiver requestdoes not exempt claims from standard claim processing rules and edits. After approval of awaiver request, a claim can still be denied for reasons unrelated to the actual waiver request.All Timely Filing Waiver Requests will appear on a future Summary Voucher as either a paid ordenied claim. Any approved waiver requests will appear accompanied by an explanation ofbenefits (EOB) code that states “Timeliness Waiver Request Approved.” Any denied waiverrequests will be accompanied by an EOB code that states “Timeliness Waiver Request Denied.”Resubmission of denied claimsClaims that have been denied due to incorrect or incomplete required data elements may beresubmitted with the appropriate information, but must be resubmitted for payment considerationwithin 60 days from the date of denial by MBHP/HNE BH.Corrected claims may be resubmitted either on paper or electronically using the Original ClaimNumber from the original claim located on the Provider’s Summary Voucher. The OriginalClaim Number needs to be on the resubmitted claim in fields:FL 64 on the UB-04 (CMS-1450)Item 22 on the CMS-1500Electronic submitters should place this information in the corresponding fields on the electronicclaim formats. Failure to put in the Original Claim Number on the paper or electronic claim willresult in the claim being denied.Resubmitted claims received after 60 days from the date of the EOB will be denied. The claimmust be physically or electronically delivered to MBHP/HNE BH by the close of business onday 60, NOT just postmarked by day 60.Adjusting incorrectly paid claimsClaims requiring reconsideration of incorrect payment amounts, excluding denials, must beresubmitted to MBHP/HNE BH on an Adjustment/Reversal Request form within 180 days fromthe date of service to be considered for adjustment. Denied claims should follow theResubmission of Denied Claims process previously described. Electronic submissions of theAdjustment/Reversal Request form will not be accepted. The Adjustment/Reversal form can befound in the forms area of this section. One form should be completed for each original claimbeing adjusted. If multiple claims are being adjusted for the same reason, oneAdjustment/Reversal form can be completed for the group of claims. Each claim must still beaccompanied by any required documentation. All items on the form are required.Instructions for completing the Adjustment/Reversal form are:145
Provider informationEnter the name, number, and address of the provider to whom the payment was made.Member informationEnter the Member’s name and number as it appears on the Summary Voucher.Claim informationEnter the claim number and date as listed on the Summary Voucher.Reason for adjustmentPlace an “X” on the line that best describes the reason for requesting the Adjustment/Reversal,and enter the required information. If “Other, Please Explain” is marked, describe the reason forthe Adjustment/Reversal request.Provider signature and dateAn Adjustment/Reversal request cannot be processed without a typed, signed, stamped, orcomputer-generated signature and the date that the form was completed.A copy of the corrected claim form and a copy of the Summary Remittance Voucher page onwhich the original claim appears must be included with the Adjustment/Reversal form. It is notnecessary to attach a refund check to the Adjustment/Reversal form. Any reduction or increasein payment will be applied to the weekly payment cycle following processing. TheAdjustments/Reversals will appear as negative claim amounts regardless of whether a refundcheck is submitted. If submitted, the refund check will appear as an applied amount at the end ofthe Summary Remittance Voucher detailing the claims that were adjusted/reversed. The checknumber of the provider’s refund check will appear as the transaction reference number on anMBHP/HNE BH Summary Remittance Voucher.Please mail completed forms and claims to:MBHP/HNE BHAttn. Adjustments/ReversalsP. O. Box 55871Boston, MA 02205-5871Claim review processPrior to submitting a Claim Review Form, the provider may choose to contact MBHP/HNE BH’sCommunity Relations Department at 1-800-495-0086 to rectify the issue; if the issue cannot beresolved by the Community Relations Representative, a Claim Review may be necessary. AClaim Review is a review of a denied claim or a payment dispute. Therefore, a Claim Reviewmust be preceded by a claim submission.Requests for a Claim Review concerning retroactive Member eligibility, and retroactive clinicalauthorization for service should only be submitted after completion of the Timely Filing WaiverProcess.146
Providers must submit a Claim Review Form to MBHP/HNE BH and a formal letter explainingthe rationale for the request in order to initiate the Claim Review process. For a Claim Reviewinvolving a clinical level-of-care issue, a copy of the entire medical record may be required. Ifthe Claim Review concerns a claim or claims that have not met the original timely filingrequirement, you must also complete the section detailing the reason the claim was not submittedwithin the required filing time.Some examples of supporting documentation that may help in getting the Claim Reviewapproved should accompany the Claim Review Form and formal letter. Explanation of benefits from primary insurance carrierTime-stamped faxes or copies of authorizationsPrintouts from EVSMonthly EDS Summary Reports indicating eligibility checks performed during the monthin questionAny other supporting documentationThis information should be mailed to:MBHP/HNE BHClaim Review CoordinatorP. O. Box 55871Boston, MA 02205-5871The Claim Review must be received by MBHP/HNE BH within 180 days from the date ofservice or date of discharge on the claim. Any Claim Review received after 180 days will bereturned with a letter of denial, and MBHP/HNE BH’s Claim Review Committee will take nofurther action.MBHP/HNE BH’s Claim Review Committee may request additional information beforerendering a decision. The provider will be notified in writing of the final decision. As set forthin the Provider Agreement, the provider shall have no recourse against the MassHealthBehavioral Health Program for a decision made by MBHP/HNE BH.Specific outpatient limitations Providers must submit a separate claim for each treating practitioner.A provider may render two separate and distinct outpatient services to the same recipienton the same day when clinically necessary. Providers may render the same service to thesame recipient on the same day only in exceptional cases where it is clinically necessaryand pre-authorized by MBHP/HNE BH. The general limitations on multiple outpatientservices are listed below. Deviation from these guidelines must be clinically necessary andpre-authorized by MBHP/HNE BH.147
MBHP/HNE BH ADMINISTRATIVE OPERATIONSFORMS Adjustment-Reversal Form Claim Review Form Third Party Liability Form Timely Filing Waiver Form Website Registration Form
MASSACHUSETTS BEHAVIORAL HEALTH PARTNERSHIP/HEALTH NEW ENGLAND BE HEALTHY(MBHP/HNE BH)ADJUSTMENT/REVERSAL FORMAdjustmentReversalPayment increasePayment decreaseProvider name:Enrollee name:Provider number:Enrollee number:Provider address:MBHP/HNE BH claim number:MBHP/HNE BH paid date://Reason for AdjustmentEnrollee name/RID:Correct enrollee Correct RIDDate of service:Incorrect dateCorrect dateBilling code error:Incorrect codeCorrect codeUnits incorrect:Incorrect units Correct unitsIncorrect professionalLevel billed:Incorrect levelCorrect levelProvider/vendor paid: Incorrect provider # Correct provider #Incorrect vendor # Correct vendor #Other reimbursement: Source: Amount:Authorization extended - authorization number:Other: (please explain)If there are any questions regarding this adjustment request, please contact MBHP/HNE BH’s Community RelationsDepartment at 1-800-495-0086.Provider signature:Date:MBHP/HNE BHProcessor: Code:Date:REV 12/2009ApprovedDenied
Claim Review FormMASSACHUSETTS BEHAVIORAL HEALTH PARTNERSHIP/HEALTH NEW ENGLAND BE HEALTHY(MBHP/HNE BH)Provider Name:Contact Person:Provider Number:Telephone Number:Provider Address:Extension:Claim Review RequestedEnrollee Name:Type of Service:Enrollee Number:InpatientHolding/Obs BedDetoxPartial/Day TreatmentOutpatient ProfessionalResidentialFSTTestingCSPOther:Date(s) of Service (If outpatient, please list dates):Please note that a formal letter explaining the reasons for the review must be attached to this formalong with any documentation that supports the request. This may include, but is not limited to,REVS printouts obtained on the dates in question, notes charted from conversations with MBHP/HNEBH employees, MBHP/HNE BH authorization letters, remittance advices, or other materials deemedimportant to substantiate your request.Was a claim submitted?YesNoIf no prior claim was submitted, a claim must be submitted with this form.Was the original claim filed timely?YesNoIf “No,” please briefly explain why:If there are any questions regarding this request, please contact MBHP/HNE BH’s Community RelationsDepartment at 1-800-495-0086.Provider signature:Date:MBHP/HNE BH OnlyReceived date: / /Review number:Date presented to committee: / /ApprovedDeniedComments:Revised: 12/2009
MASSACHUSETTS BEHAVIORAL HEALTH PARTNERSHIP/HEALTH NEW ENGLAND BE HEALTHY(MBHP/HNE BH)THIRD PARTY LIABILITY FORMMember InformationEnrollee’s name: Enrollee’s RID:Enrollee’s date of birth: / /Reason For Third Party Liability FormAdd policyUpdate existingpolicyCancel existingpolicyDelete incorrectpolicyThird Party Liability InformationPolicyholder’s name: Relationship to enrollee:Insurance carrier name:Policyholder’s SSN:Policy number (if different):Group number:Policy start date: / / Policy end date: / /Employer name:Employer address:Plan type:SingleFamilyCurrent Medicaid recipients covered by insurance plan:Name:RID:Date of birth/ // // /PCG Notes OnlyPCG comments:MBHP/HNE BH Use OnlyTPL log number:Coverage start date: / /TPL processor:Coverage end date: / /Date: / /Notes:Rev 12/2009
MASSACHUSETTS BEHAVIORAL HEALTH PARTNERSHIP/HEALTH NEW ENGLAND BE HEALTHY(MBHP/HNE BH)TIMELY FILING WAIVER FORMProvider name:Enrollee name:Provider number:Enrollee number:Provider address:Date of service:Original claim number:Was the original claim filed in a timely manner?YesNoIf “No,” please briefly explain why:Reason for Waiver RequestRetroactive Enrollee EligibilityRetroactive Clinical AuthorizationOther (please explain):Please note that any requests for consideration not covered by the reasons above must be submitted using MBHP/HNEBH’s Administrative Appeal Form.If there are any questions regarding this adjustment request, please contact MBHP/HNE BH’s Community RelationsDepartment at 1-800-495-0086.Provider signature: Date:MBHP/HNE BH OnlyProcessor:Date:Code:ApprovedDeniedComments:REV 12/2009
Massachusetts Behavioral Health Partnership/Health New England Be Healthy (MBHP/HNE BH)PROVIDER WEB SITE REGISTRATION FORMEach facility or individually contracted provider may request multiple accounts bycompleting this form for each contracted site/Medicaid number.Provider Name: Individual practitionerInpatient facilityOutpatient facilityGroupEmergency Service ProgramNPI #User name: (pleaseprint legibly)Password: (please printlegibly)E-mail address: (pleaseprint legibly)Phone number:*Please ensure that the User Name and Password you create is something you will remember. Allpasswords should be kept confidential.CEO/President or Individual Practitioner name (PLEASE PRINT)DATECEO/President or Individual Practitioner signatureCompletion of this registration form is required for all providers contracted withMBHP/HNE BH. MBHP/HNE BH providers are required to adhere to the policies andprocedures outlined in the MBHP/HNE BH Provider Manual. The Provider Manual andAlerts can be found on the www.masspartnership.com under the “HNE Be Healthy”section.The login name and password allows providers to have access to the MBHP/HNE BHProvider Manuals, IVR registration, and all Alerts. It is recommended that providersreview the web site on a regular basis to obtain news and information regarding policyand procedure changes.If you have any questions about this form please contact David Wildman at:800-495-0086, ext. 453101 or Brian O’Hara at 617-790-5671.Fax or Mail the completed form to: Provider Relations, MBHP/HNE BH, 100 HighStreet 3rd Floor, Boston, MA 02110 – Fax: (877) 390-2324
MBHP/HNE BH ADMINISTRATIVE OPERATIONSAPPENDIX Benefit Service Grid
MBHP/HNE BH recommends that providers check for possible MassHealth and/or MBHP/HNE BH eligibility for each individual who seeks care. An individual may have applied for . Claims Mailing Address: MBHP/HNE BH Claims . P.O. Box 55871 . Boston, MA 02205-5871 . The second step in getting a claim paid is to submit a complete and accurate claim .