Transcription
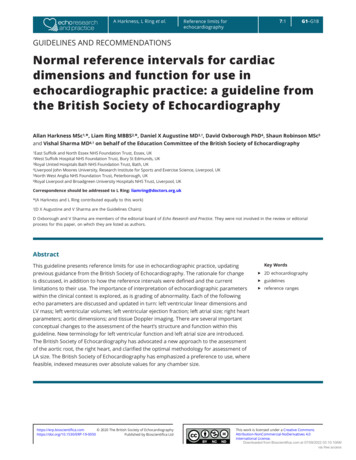
A Harkness, L Ring et al.7:1Reference limits forechocardiographyG1–G18GUIDELINES AND RECOMMENDATIONSNormal reference intervals for cardiacdimensions and function for use inechocardiographic practice: a guideline fromthe British Society of EchocardiographyAllan Harkness MSc1,*, Liam Ring MBBS2,*, Daniel X Augustine MD3,†, David Oxborough PhD4, Shaun Robinson MSc5and Vishal Sharma MD6,† on behalf of the Education Committee of the British Society of Echocardiography1EastSuffolk and North Essex NHS Foundation Trust, Essex, UKSuffolk Hospital NHS Foundation Trust, Bury St Edmunds, UK3Royal United Hospitals Bath NHS Foundation Trust, Bath, UK4Liverpool John Moores University, Research Institute for Sports and Exercise Science, Liverpool, UK5North West Anglia NHS Foundation Trust, Peterborough, UK6Royal Liverpool and Broadgreen University Hospitals NHS Trust, Liverpool, UK2WestCorrespondence should be addressed to L Ring: liamring@doctors.org.uk*(A Harkness and L Ring contributed equally to this work)†(DX Augustine and V Sharma are the Guidelines Chairs)D Oxborough and V Sharma are members of the editorial board of Echo Research and Practice. They were not involved in the review or editorialprocess for this paper, on which they are listed as authors.AbstractThis guideline presents reference limits for use in echocardiographic practice, updatingprevious guidance from the British Society of Echocardiography. The rationale for changeis discussed, in addition to how the reference intervals were defined and the currentlimitations to their use. The importance of interpretation of echocardiographic parameterswithin the clinical context is explored, as is grading of abnormality. Each of the followingecho parameters are discussed and updated in turn: left ventricular linear dimensions andLV mass; left ventricular volumes; left ventricular ejection fraction; left atrial size; right heartparameters; aortic dimensions; and tissue Doppler imaging. There are several importantconceptual changes to the assessment of the heart’s structure and function within thisguideline. New terminology for left ventricular function and left atrial size are introduced.The British Society of Echocardiography has advocated a new approach to the assessmentof the aortic root, the right heart, and clarified the optimal methodology for assessment ofLA size. The British Society of Echocardiography has emphasized a preference to use, wherefeasible, indexed measures over absolute values for any chamber size.https://erp.bioscientifica.com 2020 The British Society of 0Published by Bioscientifica LtdKey Wordsff 2D echocardiographyff guidelinesff reference rangesThis work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/09/2022 03:10:10AMvia free access
A Harkness, L Ring et al.IntroductionThe British Society of Echocardiography (BSE) haspreviously provided reference values and guidelines forchamber quantification through the provision of posters,pocket guides and the EchoCalc app (1, 2). These werebased on joint publications by the American Society ofEchocardiography (ASE) and the European Associationof Cardiovascular Imaging (EACVI), originally publishedin 2005 (3). Newer right heart data were derived fromguidelines published in 2010 (4). The ASE and EACVIsubsequently updated their guidelines in 2015 (5, 6).Since that time further research has been published, usingprospective data collection, on which the BSE has chosento base the current recommendations upon.For the current guidance, the BSE has chosen, insome instances, to deviate from the combined Europeanand American guidance for our own reference intervals.There were several reasons for this. Principally, the BSEwanted to ensure that the reference ranges were derivedfrom the most contemporaneous and prospectivelyacquired data; that reference ranges were derived fromevidence that best applies to the British population; andfinally ensure that echo guidance and cut-offs reflectpractice within the UK. This document will outline theapproach taken by the BSE in producing the up-to-dateBritish guidelines, in addition to detailed explanatorynotes regarding each parameter in turn. Referenceintervals for the parameters in Table 1 are described inthe main document and summarised in SupplementaryTable 1 (see section on supplementary materials givenat the end of this article). Diastolic parameters will becovered in a separate guideline.The overarching objectives of this document were to:1. Provide a simple, practical reference document andguide for everyday use by our members.2. Enable appropriate interpretation of values into aclinically relevant report.3. Encourage the holistic interpretation of measurements –no single number should define normality or pathology.The BSE acknowledges that the changes suggested withinthis document may result in some individuals who werepreviously labelled as having an echocardiographicabnormality now being considered as normal (and viceversa). Although this can present a challenge to clinicians,the changes are necessary and are reflective of the currentevidence-base. The BSE advocates that echo departmentsdiscuss the new reference limits with end-users, includingcardiologists and other clinicians, to ensure that thehttps://erp.bioscientifica.com 2020 The British Society of 0Published by Bioscientifica Ltd7:1Reference limits forechocardiographyTable 1G2Echocardiographic parameters covered by the BSE2019 guidelines.BSE reference intervals 2019Linear left ventricular dimensions and LV massLeft ventricular volumesLeft ventricular ejection fractionLeft atrial volumeIndexed right ventricular end diastolic areaIndexed/non-indexed right atrial areaRight ventricle and right ventricular outflow tract diameterRight ventricular fractional area changeAortic root dimensionsTissue Doppler: mitral annular s′ and right ventricular s′changes suggested within this document are rationalisedand that patient care is not adversely affected.MethodsSource dataA reference interval for any echocardiographic parametershould be derived from a population of apparently normalindividuals: that is to say, a group of individuals who aredevoid of overt cardiovascular disease. It is preferred ifindividuals with multiple risk factors for cardiovasculardisease (for example, a history of smoking or strongfamily history of coronary disease) are excluded as theymay have as yet undiagnosed cardiac abnormalities thatcould influence the results. Once the population hasbeen defined, adequate numbers of ‘normal’ participantsacross the spectrum of ages and body sizes are neededto ensure that the reference limits can be consideredrepresentative of the population at large. Studies ideallyshould be prospectively recruited and not identified fromretrospective review of echo databases. There should beclear echo protocols such that each parameter is obtainedusing optimized views and best practice. In the perfectscenario, echo images would be reported in a core-lab, ordedicated independent echo-lab, to guarantee that theanalysis of images and therefore the results are consistent.Finally, the individuals included in the reference datashould reflect the population to which the ranges willthen be applied.The ASE/EACVI guidance from 2015 extracted echodata from several large databases to derive referenceintervals (5, 6). This was commendable as it maximizesthe number of participants, but for some parametersresults in suboptimal methodology: for example, leftventricular ejection fraction (LVEF) from the apicalfour-chamber view was obtained from more than 2000This work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/09/2022 03:10:10AMvia free access
A Harkness, L Ring et al.individuals, but the biplane LVEF intervals were derivedfrom around 500 patients. In addition, including datafrom multiple sources means that the echocardiographicmethods for all subjects were not necessarily uniform,nor was quality assured with the use of a dedicatedindependent echo-lab. Finally, some results were obtainedfrom a North American population and therefore may notbe completely applicable to the British iographic reference intervals have beenpublished subsequent to the joint ASE/EACVI guidance.The first of these was the Normal Reference Ranges forEchocardiography (NORRE) dataset which has resultedin multiple publications (7, 8, 9, 10). The NORRE projectincluded over 700 individuals, and the study design andexecution fulfil many of the ideal criteria outlined above.Participants were prospectively recruited, with predefined echo protocols. All echo data were analysed bya core-lab, ensuring consistency of results. The includedindividuals were free from both overt cardiovasculardisease and had low clinical probability of latent disease,were not taking any cardio-active medication, and allhad lab testing for hyperglycaemia, dyslipidaemia,and renal function. Competitive athletes and obeseindividuals were excluded. Care was taken to ensure thatsufficient numbers of individuals from all age categorieswere included. This study was a European collaborativeproject and therefore the results can be consideredapplicable to the UK population (7).The second study was the EchoNormal project, alarge meta-analysis of more than 50,000 individuals ofdiffering ethnicities, obtained from over 40 differentstudies undertaken worldwide (11). After exclusions,more than 22,000 participants were used to define7:1Reference limits forechocardiographyG3reference intervals. The results from the EchoNormalproject provide a valuable insight into ethnic variation,and age-dependent changes of echo parameters. It iscommendable that the cohort used in EchoNormal waslarge. However, the meta-analysis design means that theinclusion criteria for each of the 43 studies included werenot necessarily identical, and the definition of ‘normal’was not uniform. Echo images were analysed in theindividual centres, and therefore consistency could not beguaranteed. For some parameters (including ventricularvolumes and LVEF), data from one or more centres wereexcluded as it appeared to deviate significantly from theresults seen elsewhere, which raises questions regardingvalidity. Finally, a large proportion of the participantswere not European, and therefore the relevance to a UKpopulation is less clear.For these reasons, the current BSE reference intervalswere in large part derived from the NORRE dataset.Defining reference intervalsThis guideline proposes reference intervals forechocardiography. These are not the same as ‘normalranges’, and it is of paramount importance to understandthe difference as this necessarily affects the way in whichthe ranges produced within this document are applied inday-to-day practice.Statistical convention used throughout the literaturestates that a reference interval includes 95% of thenormal population (Fig. 1). By definition, this excludesthe remaining ‘normal 5%’ who appear at the upper andlower extreme. If the parameter in question is normallydistributed, the 95% reference intervals can be obtainedfrom the data using the mean 1.96 standard deviation.Figure 1The normal distribution curve. Using acombination of the population mean andstandard deviation, reference limits can becalculated. A range of values encompassing 2standard deviations above and below thepopulation mean includes 96.4% of all ‘normal’subjects. Similarly, 3 standard deviationsencompass 99.7% of the normal population.https://erp.bioscientifica.com 2020 The British Society of 0Published by Bioscientifica LtdThis work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/09/2022 03:10:10AMvia free access
A Harkness, L Ring et al.However, for almost a century, 1.96 has been rounded to2, which covers 95.4% of the population (12). Thus:Upper reference limit (URL) mean value (2 standard deviation)Lower reference limit (LRL) mean value –(2 standard deviation)It is a frequent misconception that if an individual parameterfalls outside of the reference limits it should always beconsidered as abnormal. If we take the example of leftventricular (LV) dimensions: using the above methodology,it is expected that 4.6% of all normal patients will havevalues that are either above the upper reference limit orbelow the lower reference limit. In clinical practice, moreimportance is often applied to one extreme: practitionersmay consider an increased LV size as clinically more relevantthan a reduced size. Even in this scenario, a substantialnumber of individuals (2.3% of ‘normal’ patients) willhave LV dimensions that are above the URL. It is thereforeessential to interpret any value that falls outside of thereference limits within the clinical context, rather thanimmediately consider them as abnormal.Similarly, it is also possible for a parameter to fallwithin the reference interval, and yet, it may not actuallybe ‘normal’ for that individual. For example, a patient maybe noted to have an LVEF result that drops from 65 to 55%on sequential measurements. Although both of these LVEFvalues are within the ‘normal reference limit’, in this case,it is quite possible that there is an underlying pathologicalprocess and incipient LV systolic dysfunction. It is thereforeof paramount importance that echocardiographic values,whether they are superficially normal or not, are alwaysinterpreted in the clinical context. If a patient has hadprevious echo studies, comparison between historical andcontemporary findings is of significant clinical utility.The above statistical methodology has been appliedto the NORRE data to derive reference limits for mostechocardiographic parameters. Detailed explanations areprovided where the BSE has deviated from this practice.Grading of abnormalityOnce an echocardiographic value falls outside of the referenceintervals, it is common practice to consider the parameter inquestion as being ‘mildly, moderately or severely’ abnormal(bearing in mind that, as discussed above, the normal/mildlyabnormal zone will have some overlap). There are severalreasons why this approach is useful: it helps to give an ideaas to the magnitude of abnormality to the referring clinician,it may provide use in monitoring of disease progression,https://erp.bioscientifica.com 2020 The British Society of 0Published by Bioscientifica LtdReference limits forechocardiography7:1G4or it may provide information as to prognosis for a particulardisease. To a clinician, an abnormality labelled as ‘severe’will usually demand attention and probably treatment (i.e.it should not be ignored).The partition between a ‘mild and moderate’, or‘moderate and severe’ abnormality can be defined ina number of ways. Perhaps the ideal method would beto define the severity of the abnormality according toprognostic significance: progression from mild to moderateto severe abnormality would be associated with clearimpact on cardiovascular outcomes from contemporarystudies. In reality, however, most echocardiographicparameters such as LVEF or LA size display a continuousassociation with survival (i.e. as the LVEF gets progressivelylower, survival is progressively poorer (13)), and specificcut-offs are defined more for clinical simplicity and utilityas opposed to being genuinely disease defining. A differentmethodology would be to define partitions according toclinical intervention(s) available at specific points.Another frequent practice is to define these partitionsas a function of the standard deviation and the mean.Just as the upper reference limit is usually two standarddeviations above the mean, the partition between mildand moderate abnormality is defined as three standarddeviations above the mean, and the moderate/severethreshold as four standard deviations above the mean. Thisis akin to paediatric cardiologist’s use of Z-scores, wherethe Z-score is the number of standard deviations from themean (14). Although superficially this approach may notappear to have clinical relevance, it has value in providinginformation as to how frequently this magnitude ofvariation would be expected within a normal population.Taking the example of LV dimensions: just as 2.3% ofnormal individuals will have an LV size above the upperreference limit, a tiny proportion of normal individuals(just 0.15% of the normal population) would havevalues in the ‘moderate’ range using this methodology.Furthermore, essentially no normal patients would everbe expected to have LV dimensions in the ‘severe’ range(Fig. 1). This further re-iterates the clinical approach thatonce an individual parameter is close to severely abnormalimmediate clinical attention is warranted.Within these guidelines, grading ranges have beenprovided only where they have clinical utility.Normal variationMany, if not all, echocardiographic parameters varyaccording to gender, body habitus (either height, weightor both), ethnicity, fitness, and age. If all these variablesThis work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/09/2022 03:10:10AMvia free access
A Harkness, L Ring et al.were factored into every single measurement, reportingtimes would become unreasonable, and the associatedreference tables would be unwieldy. We have attemptedto include as many useful variables as is practical, whilstmaintaining the simplicity for busy echo practitioners.However, this has necessarily led to some compromises.One compromise is regarding age-related variations.Several echocardiographic criteria (for example left andright ventricular size and LVEF) vary with normal aging,whereas others (including left and right atrial volumesand LV mass) do not (8). The BSE believes that it would beimpractical to divide reference tables to account for thisvariation in some but not all parameters, particularly ifthe absolute difference is often so small as to be clinicallyinsignificant. This compromise approach re-iterates theneed to interpret values that are slightly outside thereference limits with caution, particularly if they areobtained in patients at the extremes of age.Echocardiographic parameters are usually indexedaccording to BSA. For certain parameters, such as leftatrial (LA) volumes, there is a wealth of evidence thatthis approach is reasonable (15, 16). For others, thisapproach may not be as useful. For example, althoughthe NORRE dataset published indexed values for internalLV dimensions and LA diameter, neither of these areroutinely used in clinical practice. The absolute LVinternal diameter is a predictor of outcomes in mitral andaortic valve disease and is used to guide timing of surgicalintervention (17, 18, 19). There is less data to supportthe use of indexed values in this regard. Therefore, theBSE has chosen to publish indexed values only for thoseparameters where there is a clear clinical indication forthis approach.In obese patients, caution is advised wheninterpreting indexed values, particularly as the NORREdatabase excluded individuals with a BMI 30 kg/m2. Themetabolic demand of fatty tissue is considerably lowerthan muscle, and therefore, obesity is less likely to drivechanges in chamber size or wall thickness. In essence,indexing for body surface area (BSA) when individuals arevery overweight may result in an underestimation of thedegree of cardiac remodelling (20).LimitationsThere are three patient cohorts in whom these referencetables may not be applicable. These are non-Caucasianindividuals, athletes, and pregnant patients.The NORRE dataset included healthy Caucasianvolunteers only, and therefore, the values provided inhttps://erp.bioscientifica.com 2020 The British Society of 0Published by Bioscientifica LtdReference limits forechocardiography7:1G5the tables will not be as reliable in individuals of differentethnic origin (7). For example, there is some evidence thatindividuals of Afro-Caribbean or Asian descent differ fromCaucasian counterparts with regards LV mass values (11).The BSE has chosen not to include ethnicity-specificreference intervals for several reasons. Firstly, as wediscussed earlier, currently available ethnicity-specificdata from EchoNormal is not as robust as NORRE. As yetunpublished data from the upcoming World Allianceof Societies of Echocardiography Normal Values Study(WASE trial, presented in abstract form) suggests that inaddition to ethnicity, the country in which an individuallives results in important echocardiographic variation.For example, individuals of Chinese descent differconsiderably if they live in China compared to thosethat live in Europe. Similar inter-country variation wasseen with all ethnicities. This further reinforces the BSE’sbelief that using data obtained from China or Asia toderive reference intervals for individuals living in theUK would not be valid. Secondly, an ethnic-specificapproach would necessarily require all sonographers toask for a patient’s ethnic origin prior to undertaking anecho exam, which could be considered unreasonable.Thirdly, it is likely that individuals of mixed heritagewould not fit solely into one dataset or another, whichwould introduce further difficulties when asking patientsregarding their ethnicity and subsequently interpretingthe echo findings.Therefore, the BSE proposes that the presentedreference tables are used for patients of all ethnicities butreminds sonographers to be aware of potential variationsecondary to ethnicity. Although the available data are notsufficient to derive specific reference limits, the followingcould be considered within the clinical context: Individuals of Afro-Caribbean descent appear to bevery similar to Caucasians with regards LV volumesand function. LV mass, however, may be marginallyhigher, and therefore a ‘mild’ increase in LV massshould be interpreted with caution and within theclinical context. Individuals of East Asian or Indian origin may havea tendency towards slightly smaller LV volumes. Assuch it is possible that LV volumes approaching theproposed upper reference limits may in fact be slightlyabnormal for such ethnic groups and should beinterpreted within the clinical context. There are insufficient data to provide advice regardingthe effects of ethnicity on LA volume or right heart sizeat this time.This work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/09/2022 03:10:10AMvia free access
A Harkness, L Ring et al.Echocardiography in athletes should also be interpretedwith caution. Participation in competitive sport results inremodelling and morphological alterations of the heart,including increases in: LV dimensions and volumes, rightventricular (RV) dimensions, LV mass, and LA volumes(21, 22, 23, 24). The magnitude of these morphologicalalterations appears to be linked to both the volume andtype of exercise undertaken. There is no practical or widelyaccepted way in which the effects of exercise on cardiacstructure can be readily standardized or accounted for.NORRE actively excluded individuals who participatedin competitive sport. For this reason, sonographers andclinicians should be cognizant of these potential influenceswhen interpreting the echocardiographic findings of suchindividuals (23).Finally, caution is advised when using these referencetables to interpret echocardiographic studies in pregnantwomen. Physiological cardiac adaptation duringpregnancy includes enlargement of the left and rightventricles and the atria, in addition to changes in left andright ventricular function (25). NORRE excluded pregnantindividuals from the study.TimingTiming of measurements is critical. ECG timings can varywith the lead used and is affected by conduction defectsand coronary artery disease (26). The 2015 chamberguidelines and many textbooks have varying definitions(5, 6). The definitions from the EACVI/ASE/Industry TaskForce paper on standardising deformation imaging havethus been adopted as follows (27).Ventricular end systoleThe timing of ventricular end systole is taken as the framewhere the aortic valve initially closes. This coincides witha closure click on the pulsed-wave Doppler tracing ofaortic valve flow. When obtaining images from the apical2- or 4-chamber views, end-systole is defined as the frameprior to mitral valve opening (5, 6). In addition, this isthe point at which maximal volume of the LA should beobtained.Ventricular end diastoleThe timing of ventricular end diastole is taken as theframe before the mitral valve closes. Surrogates for thisare the frame with the largest LV cavity size (diameter orvolume), the start of the ECG QRS complex, or the ECGR-wave (a common trigger for analysis software).https://erp.bioscientifica.com 2020 The British Society of 0Published by Bioscientifica Ltd7:1Reference limits forechocardiographyG6BSE reference intervalsThe following section outlines the new BSE referencelimits for left and right heart parameters, combinedwith explanations of the methodology, decision-makingprocess, and discussions regarding the potential clinicalimpact of the new reference intervals. Where appropriate,we have described the methodology by which some ofthe measurements should be acquired, but for a moredetailed description regarding the echocardiographicmeasurements and how they should be obtained, pleasesee the BSE minimum dataset (28).Left ventricular linear dimensions and LV massNew reference intervals for linear LV dimensions andLV mass are presented in Table 2. LV dimensions shouldbe obtained from the parasternal long-axis (PLAX)window preferentially using 2D imaging. The BSE woulddiscourage the use of M-mode measurements as routine,although they are acceptable if the long-axis of the leftventricle is perpendicular to the angle of incidence ofthe ultrasound beam. LV mass should be calculated usingthe linear method from 2D imaging and reported afterindexing to BSA (8).The BSE has chosen to publish an upper referencelimit only for wall thickness measures with no separateTable 2Linear left ventricular dimensions and mass.NormalMalesLV dimensionsLVIDd (mm)LVIDs (mm)IVSd (mm)LVPWd (mm)LV massLVMi (g/m2)LV mass (g)FemalesLV dimensionLVIDd (mm)LVIDs (mm)IVSd (mm)LVPWd (mm)LV massLVMi (g/m2)LV mass ��6141–45––61–6546–50–– 65 50––40–11072–219111–127–128–145– ��56–5943–46–– 59 46––33–9951–17398–115–116–131– 131–IVSd, inter-ventricular septal thickness in diastole; LV, mass calculated usingthe linear method; LVIDd, left ventricular internal diameter in diastole; LVIDs,left ventricular internal diameter in systole; LVMi, left ventricular mass index;LVPWd, left ventricular posterior wall thickness in diastole.This work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0International License.Downloaded from Bioscientifica.com at 07/09/2022 03:10:10AMvia free access
A Harkness, L Ring et al.partitions for mild, moderate, or severe changes, as usingstandard deviations to define partitions would resultin such narrow ranges that they would be clinicallymeaningless.LV wall thickness by itself does not define an individualas having left ventricular hypertrophy (LVH). Rather, thepresence or absence of LVH is determined from LV massafter indexing to BSA. Wall thickness measurements,combined with the LV internal diameter in diastole, canbe used to determine the relative wall thickness (RWT)using the following formula:RWT IVSd LVPWdLVIDdThe combination of indexed LV mass and relative wallthickness can be used to define LV geometry (Fig. 2). In thecontext of an increased mass, an RWT 0.42 defines thepattern of LVH as being ‘concentric’. If the RWT is 0.42,7:1Reference limits forechocardiographyG7the pattern of LVH is ‘eccentric’. The pattern of LVHprovides an insight into the underlying pathophysiologicalstate. Concentric LVH is characteristically seen inpatients with increased afterload such as aortic stenosisor hypertension. Eccentric LVH is more likely to be seenin scenarios with increased LV pre-load and associatedcompensatory hypertrophy, such as chronic aorticregurgitation (AR) or mitral regurgitation (MR).A common misconception is that concentric LVH issynonymous with uniform thickening of the myocardialwalls. It is possible to have localised or focal areas ofincreased wall thickness in patients with concentric LVH,just as there may be uniform thickening of muscle inpatients with eccentric LVH.If LV mass is normal (i.e. the patient does not haveLVH), an RWT 0.42 demonstrates the presence of‘concentric remodelling’. This can be thought of as a prehypertrophy state and may help to identify individualswho would benefit from identification and optimizationof risk factors (i.e. hypertension) (6).Left ventricular volumesReference intervals for LV volumes are presented inTable 3. Left ventricular volumes should be obtained using2D imaging from the apical 4- and 2-chamber windowsusing the biplane Simpson’s method. When obtaining LVvolumes using the biplane method, care should be takento ensure that the apical 4- and 2-chamber windows areseparated by 60 of rotation (and not 90 as is sometimesassumed). In addition, it is paramount that the LV is notforeshortened. Volumes should be reported after indexingto BSA.Table 3Left ventricular volumes.MalesLVEDVi (mL/m
7:1 G3 individuals, but the biplane LVEF intervals were derived from around 500 patients. In addition, including data from multiple sources means that the echocardiographic methods for all subjects were not necessarily uniform, nor was quality assured with the use of a dedicated independent echo-lab. Finally, some results were obtained