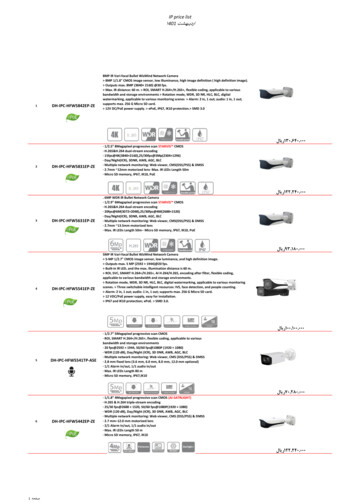
Transcription
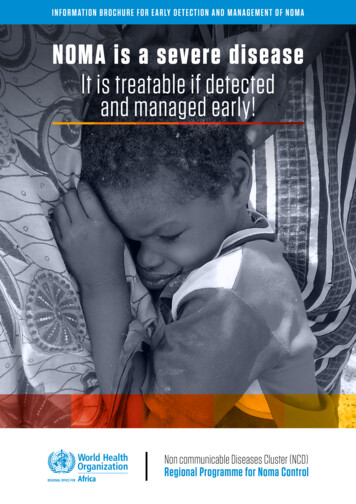
Information brochure for early detection and management of nomaNOMA is a severe diseaseIt is treatable if detectedand managed early!Non communicable Diseases Cluster (NCD)Regional Programme for Noma Control
WHO/AFRO Library Cataloguing-in-Publication DataNoma is a severe disease, which is treatable if it is managed at its early stages: informationbrochure for early detection and management of noma.1.2.3.4.5.I.Noma – etiology – prevention and control – complicationsMouth diseases – prevention and controlOral healthTraining materialHealth promotionWorld Health Organization. Regional Office for Africa II. TitleISBN: 978-929023354-1(NLM Classification: WU 140) WHO Regional Office for Africa, 2016All rights reserved.Publications of the World Health Organization enjoy copyright protection in accordance with theprovisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. Copies of thispublication may be obtained from the Library, WHO Regional Office for Africa, P.O. Box 6, Brazzaville,Republic of Congo (Tel: 47 241 39100; Fax: 47 241 39507; E-mail: afrgoafrobooks@who.int). Requestsfor permission to reproduce or translate this publication – whether for sale or for non-commercialdistribution – should be sent to the same address.The designations employed and the presentation of the material in this publication do not imply theexpression of any opinion whatsoever on the part of the World Health Organization concerning thelegal status of any country, territory, city or area or of its authorities, or concerning the delimitationof its frontiers or boundaries. Dotted lines on maps represent approximate border lines for whichthere may not yet be full agreement.The mention of specific companies or of certain manufacturers’ products does not imply that theyare endorsed or recommended by the World Health Organization in preference to others of a similarnature that are not mentioned.Errors and omissions excepted, the names of proprietary products are distinguished by initialcapital letters.All reasonable precautions have been taken by the World Health Organization to verify theinformation contained in this publication. However, the published material is being distributedwithout warranty of any kind, either express or implied. The responsibility for the interpretation anduse of the material lies with the reader. On no account shall the World Health Organization or itsRegional Office for Africa be liable for damages arising from its use.2
AcknowledgementsThe development of this brochure was coordinated by Dr Benoit Varenne, Regional Adviser for OralHealth, WHO Regional Office for Africa, with the technical support of Dr Khady Kâ of the Universityof Montréal, Canada.Dr Abdikamal Alisalad, Acting Director, Noncommunicable Diseases Cluster (NCD) of the WHORegional Office for Africa, provided general guidance for the preparation of this brochure.The WHO Regional Office for Africa would like to thank all persons who contributed in the draftingof this document and provided photographs.Special thanks are due to the experts who participated in the Delphi study to reach a consensus onnoma staging and management:Mr Mamoudou Amadou, NGO Hilfsaktion Noma e.V., Niger; Dr Denise Baratti-Mayer, GenevaUniversity Hospitals, GESNOMA, Switzerland; Dr Priscilla Benner, NGO MAMA Project, UnitedStates; Dr Marie-Claude Bottineau, Médecins Sans Frontières, Switzerland; Dr SouleymaneBougoum, Ministry of Health, Burkina Faso; Professor Denis Bourgeois, Université Lyon 1, France;Dr Eric Comte, Médecins Sans Frontières, Switzerland; Professor Emmanuel Crezoit, Ministry ofHigher Education and Scientific Research, Côte d’Ivoire; Dr Elizabeth Dimba, University of Nairobi,Kenya; Dr Oumarou Djibo, Ministry of Health, Niger; Dr Yvette Dossou, Université Libre de Bruxelles,Belgium; Dr Charlotte Faty Ndiaye, WHO, Cameroon; Dr Almoustapha Illo, Ministry of Health, Niger;M. Patrick Joly, Fondation Sentinelles, Switzerland; Dr Mamane Kaka, Hôpital national Lamorde,Niger; Dr Midion Mapfumo Chidzonga, University of Zimbabwe, Zimbabwe; Dr Klaas Marck, DutchNoma Foundation, Netherlands; Professor Andrea Mombelli, Université de Genève, GESNOMA,Switzerland; Professor Denys Montandon, formerly of Geneva University Hospitals, GESNOMA,Switzerland; Professor Sudeshni Naidoo, WHO Collaborating Centre for Oral Health, University ofWestern Cape, South Africa; Dr Emmanuel Otoh, The Regional Centre for Oral Health Researchand Training Initiatives for Africa, Nigeria; Professor Dieudonné Ouedraogo, Centre hospitalierUniversitaire Yalgado Ouedraogo, Burkina Faso; Dr Reshma Phillips, Maryland Dental ActionCoalition, United States; Professor Brigitte Pittet-Cuénod, Geneva University Hospitals, GESNOMA,Switzerland; Dr Will Rodgers, NGO Facing Africa, United Kingdom; Dr Leila Srour, NGO HealthFrontiers, Lao People’s Democratic Republic; Dr Lassara Zala, Director, Centre Persis, Burkina Faso.Heartfelt thanks also go to Cyril O. Enwonwu, Professor Emeritus of the University of Maryland(USA) for his consistent support.Representatives of the target readership including WHO staff in 10 countries in the Region(Benin, Burkina Faso, Côte d’Ivoire, Guinea-Bissau, Mali, Niger, Nigeria, Democratic Republic ofthe Congo, Senegal and Togo) kindly reviewed the brochure and provided input. We thank themfor their input. The WHO Regional Office for Africa warmly acknowledges the financial supportprovided for this project by the NGO, Hilfsaktion Noma e.V. and thanks Ms Ute Winkler-Stumpf,Chairperson of the NGO Hilfsaktion Noma e.V. for her encouragement.Photo credit: WHO/Julie Pudlowski, NGO Hilfsaktion, Professor Sudeshni Naidoo, Dr DimbaElizabeth, Dr Benoit Varenne, Professor Emmanuel Crezoit, Dr Lassara Zala, Dr Will Rodgersand Dr Priscilla Benner, Dr Adeniyi Semiyu Adetunji. Layout and typesetting: Agence Panacee(www.panacee.fr)3
Why this document?In countries contending with noma, and in spite of numerous initiatives, families,community health workers and primary health care professionals are still LARGELYunder-informed about this disease. To help bridge the knowledge gap on noma andimprove early case diagnosis, detection and treatment, WHO has taken the initiativeto update the staging of the disease and to provide, for each stage identified,recommendations for enhanced management.This brochure is designed as a training tool and is intended for all stakeholders atthe primary health care level: health workers, community health care workers andopinion leaders who are in contact with the population groups at risk of contractingthe disease.What is noma?Noma (from Greek: to “devour”) is a necrotizing disease that destroys the mouth andthe face. Noma starts as a lesion (a sore) of the gums, inside the mouth. The initial gum lesion thendevelops into an ulcerative, necrotizing gingivitis that progresses rapidly, destroyingthe soft tissues and bones of the mouth and further progressing to perforate the hardtissues and skin of the face. In the absence of any form of treatment, noma is fatal in 90% of cases. Where nomais detected early, its progression can be rapidly halted, either through basic hygienerules or with antibiotics. Such early detection helps to prevent suffering, disabilityand death. It mostly affects young children between the ages of 2 and 6 years suffering frommalnutrition, living in extreme poverty and with weakened immune systems. Noma isoften described as “the face of poverty”. Owing to the rapid progression of the disease and the high mortality rate associatedwith its acute phase, numerous cases of noma remain undetected.“Noma is a disease that progressesvery rapidly. Without rapid treatment,in a few days, the patient’s conditionbecomes life-threatening.”4
Mostly affectschildren agedbetweenDisease known for over1 000years1994,WHO declared nomaa public health problem26andyearsNow mostly prevalent in sub-Saharan AfricaRare cases reported in Latin America and Asia90As much asmortality rate140 000%estimatednew cases/yearly Sepsis Dehydration Malnutrition(Source WHO 1998)Without treatment,noma results in: A s much as 90% mortality rate. Affected persons die of sepsis or severedehydration and malnutrition. Survivors suffer from severe facial disfigurement, have difficulty speaking andeating and face social stigma.5
What is the causativeagent of noma?The causative agent of noma remains unknown. It seems unlikely that a single infectiousagent (virus or bacteria) is responsible for the disease. It would be more appropriateto speak of factors that contribute to the onset of the disease, or its determinants. N oma is the result of complex interactions in immunosuppressed children living inextreme poverty. The validation of a hypothesis pointing to a causative sequenceresponsible for the disease is ongoing. I n addition to known factors such as malnutrition, coinfections - measles and malaria- and poor oral hygiene, a number of social and environmental factors such asmaternal malnutrition and closely-spaced pregnancies that result in offspring withincreasingly weakened immune systems, could be strongly related to the onset ofthe disease (Source: GESNOMA Group. University of Geneva and Geneva UniversityHospitals).Who are the persons at riskand what social, health and economic factorsare associated with the onset of the disease? C hildren aged between 2 and 6years who are highly immunocompromised The period following the weaningof the child Extreme poverty P oor living conditions Living in resource-constrainedcountries oor oral hygieneP Malnutrition Malaria Kwashiorkor Measles HIV infection Immunocompromised adolescentsor adults6
Noma can be avoidedthrough simple actions thatcan be performed by everyone!Early detection followed by prompt treatment is crucial in improving thehealth of the affected child and can save his/her life. Treatment can beprovided at home in the early stages of the disease.First action: open andexamine your child’s mouth!Regular oral examination of childrenat home or during medical visits isan indispensable action that helpsidentify gum lesions that may developinto noma in at-risk subjects.Combatingmisconceptions Noma is not transmitted from one person toanother; noma is not a contagious disease! Noma is not caused by witchcraft or acurse on the child’s parents7
Know the stages of the diseWARNING SIGNALSimple gingivitisBleeding when touchedor during brushing; red orpurplish red gum, swellinggum.Acutenecrotizinggingivitis stageSpontaneous bleedinggum, onset of painfululceration of the gums;ulceration involving one ormore interdental papillae,fetid breath or halitosis,excessive salivation.OedemastageRapid extension of thegingival ulceration andthe mucosal tissue, fetidbreath or halitosis, facialswelling or oedema,painful cheek, high fever,excessive salivation,mouth soreness, difficultyeating, anorexia,lymphadenopathy.Progression timeline:1 to 2 weeksIndefinite duration TAKE THE PATITHIS IS A MAJOR EMERGENCY: ORHOSPITAL FTHE PATIENT’S LIFE IS IN DANGEREMERGENCY TREATD-DayD-Day 3REVERSIBLE STAGESOF THE DISEASE8D-Day 9
ase in order to act quickly!GangrenousstageExtensive destruction of intraoral softand hard tissue; lesion with a welldemarcated perimeter surroundinga blackened necrotic centre,separation of the slough, leaving ahole in the face, often around thecheeks or lips; difficulty eating; rapidperforation of the cheek; expositionof the teeth and denuded bones,progressive drying of the facialgangrene; anorexia; apathy.Progression timeline:1 to 2 weeksScarringstageTrismus may occur,depending on thelocation of the lesions,sequestration of teeth andexposure of bones andbeginning of scarring.SequelaestageThe child is disfigured.Trismus may occur,depending on the locationof the lesions; thereis teeth loss, feedingdifficulties, speechproblems, salivary leak,teeth displacement, dentalanarchy, fusion of maxillaand mandible bones, nasalregurgitation.Progression timeline:1 to 2 weeksENT IMMEDIATELY TO THE NEAREST DISPENSARYOR APPROPRIATE TREATMENTDANGER ACUTE PHASE OF NOMAMENT REQUIREDD-Day 15D-Day 30D-Day 45IRREVERSIBLE STAGESOF THE DISEASE9D-Day 5 months
WARNING SIGNALSimple gingivitisThis is a sign of poor oral hygiene.It is a major predisposing factor that mustbe diagnosed and treated.It occurs mostly in malnourished childrenwith weakened immune systems.The main signs and symptomsthat should alert you are: Red or purplish red gums B leeding gums when touched or duringbrushing of teeth Swelling gumsT here is no external sign at this stageof the disease.FIRST ACTION: OPEN AND EXAMINETHE CHILD’S MOUTHHealthy gums vs gingivitisManagement by health workers Conduct an intraoral examination of the child Provide advice on daily oral hygiene U se warm salted water (which must havebeen boiled before) to disinfect the mouth Where available, use disinfectant mouthwash Advise and/or apply a high-protein daily diet10All casesof simple gingivitisdo not develop into noma,but they constitutea sign that must betreated quickly
Medication Mouthwash with chlorhexidine 0,2%, 10 ml /3 times daily M outhwash with betadine /2 times daily can be used for children aged 0 to6 years: clean the inflamed area with a compress Vitamin A supplementsManagement by family and friends ADVICE ON HYGIENE AND DIET- H elp the child to maintain proper oral hygiene on a daily basis: use fluoridetoothpaste where possible to brush or clean their teeth each day after meals,rinse their mouth with warm salted water (which must have been boiledbefore) or with a commercial disinfectant mouthwash- Use safe drinking water- Provide a high-protein diet (beans, peas, milk, eggs, meat, fish) DOING THE RIGHT THINGS- G o to the nearest health centre if there is no improvement in the event ofspontaneous bleeding gums and if the child has trouble eating- U se your fingers or a short stick to open and examine the child’s moutheverydayNotes .11
STAGE 1 Acutenecrotizing gingivitisAcute necrotizing gingivitis is anaggravation of simple gingivitis.It is considered the first stageof noma disease.At this stage,noma can stillbe haltedThe main signs and symptomsthat should alert you are: Fetid breath or halitosis Painful ulceration of the gums Spontaneous bleeding of the gums Ulceration involving one or more interdental papillae Excessive salivation atch out when a child’s mouth is closed and he/sheWhypersalivates and emits fetid breath with a putrid smell,regardless of whether they have fever or not Be even more vigilant when the child is malnourishedwith a case history of spotted fever (chickenpox, measles)in the preceding months or even weeksManagement by health workers Nutrient supplementation High-protein daily diet AntibioticsNotes .12
Medication A moxicillin PO 100 mg/ kg every 12 hours for 14 days metronidazolePO 15 mg/ kg every 12 hours for 14 days M outhwash with Chlorhexidine 0,2%, 10 ml /3 times daily A spirin or paracetamol U se compresses soaked in hydrogen peroxide 20 volumes to cleanthe gum lesions V itamin A supplements N utritional rehabilitation: high-energy, ready to use paste,3 sachets/dailyManagement by family and friends TREATMENT TO BE PROVIDED- H elp the child to maintain proper oral hygiene on a daily basis: use fluoridetoothpaste where possible to brush or clean their teeth each day aftermeals, rinse their mouth with warm salted water (which must have beenboiled before) or with a commercial disinfectant mouthwash- Give the child appropriate soft, high-calorie foods prepared withclean water- Strictly follow the antibiotics prescriptions, dosage and timelines- Give the child food supplements: Vitamins DOING THE RIGHT THINGS- T ake the child as soon as possible to the nearest health centre- Examine the inside of the child’s mouth every day- Consult a health professional if the lesions persist, or if the child has fever,has difficulty breathing, has a swelling on his/her cheek or feels pain- Request follow up by a health professional once a week until the lesioncompletely disappears- Go to a dental clinic for an examination to be undertaken by an oralhealth care professional13
STAGE 2OedemaAt the oedema stage, the patient entersinto the acute phase of the disease. It isabsolutely essentially to act quickly to avoidany aggravation that may prove irreversible.At this stage,noma canstill be haltedThe main signs and symptomsthat should alert you are:Facial swelling or oedemaDifficulty eatingFetid breath or halitosis Rapid extension of the gingivalulceration and the mucosal tissue Soreness of lips or cheeks Facial swelling Pains that prevent the childfrom eating High feverExcessive salivationMouth sorenessAnorexiaSoft lips or cheeksFetid breathHigh feverManagement by health professionalsThe priority is to stabilize the patient and to quickly improve their general healthsituation through rehydration, nutritional rehabilitation, administration of vitamins(especially Vitamin A) and treatment with antibiotics. Correction of dehydration and Use of strong doses of antibiotics:electrolyte imbalancepenicillin and metronidazole Nutritional rehabilitation Use of disinfectant mouthwashes Treatment of conditions that Correction of anaemia with folicfoster the development ofacid, iron, ascorbic acid andmeasles, diarrhoea, malaria,Vitamin Btuberculosis, HIV Notes .14
Medication Antibiotic treatment- Option 1: Amoxicillin & clavulanicacid, 50 mg/ kg intravenously every6 hours for 14 days slowintravenous administration ofgentamycin, 5 mg /kg every 24 hoursfor 5 to 7 days slow intravenousadministration of metronidazole,15 mg/ kg every 12 hours for 14 days- O ption 2: Ampicillin intravenously,100 mg/ kg every 6 hours for 14 days slow intravenous administration ofgentamycin, 5 mg/ kg every 24 hoursfor 5 to 7 days slow intravenousadministration of metronidazole,15 mg /kg every 12 hours for 14 days Mouthwash with Chlorhexidine 0,2%, 10 ml 3 times dailyTHIS IS A MAJOR EMERGENCY:THE PATIENT’S LIFE IS IN DANGERDO NOT DELAY! REFER THE PATIENT IMMEDIATELYTO THE NEAREST HOSPITAL OR HEALTH CENTREManagement by family and friends T ake the child as soon as possible to the hospital or health centre for propertreatment Do not hide the child at home Fully and strictly follow the instructions given by health professionals15
STAGE 3GangrenousThe gangrene stage is a majoremergency; the child’s life is in danger.Sequelae will inevitably set in.There is still timeto savethe child’s lifeThe main signs and symptoms E xtensive destruction of intraoral softand hard tissue Presence of a lesion with a welldemarcated perimeter surrounding ablackened necrotic centre Bluish-black discoloration at thecorresponding external facial surface ofthe cheek or lips Separation of the slough, leaving a hole inthe face D ifficulty eating R apid perforation of the cheek, expositionof the teeth and denuded bones More extensive destruction of the coneshaped tissues below the intraoral conethan those at the top of the cone locatedon the surface of the face Progressive drying of the facial gangrene AnorexiaManagement by health professionalsThe priority is to stabilize the patient and quickly improve their general health situationthrough rehydration, nutritional rehabilitation, administration of vitamins (especiallyVitamin A) and treatment with antibiotics. Treatment of lesions: regularly bathe If the patient’s condition permits, rinsethe lesions with an antiseptic, cover theout his/her mouth daily with chlorhexidinecavities with gauze compresses soakeddigluconate solutionin antiseptic, keep the compresses Correction of anaemia with folic acid, iron,moistened by further dousing theirascorbic acid and vitamin Bexternal layers with solution Treatment of conditions that foster the Correction of dehydration and electrolytedevelopment of measles, diarrhoea,imbalancemalaria, tuberculosis and HIV Nutritional rehabilitation, preferably orally Administration of high doses of antibiotics:penicillin and metronidazoleor by parenteral administration, or by Dewormingnasogastric intubation if the patient is Management of secondary haemorrhageseverely weakenedNotes .16
Medication Antibiotic treatment- O ption 1: Amoxicillin & clavulanicacid intravenously, 50 mg/ kg every6 hours for 14 days gentamycin byslow intravenous administration, 5mg /kg every 24 hours for 5 to 7 days metronidazole by slow intravenousadministration, 15 mg/ kg every 12hours for 14 days- O ption 2: Ampicillin intravenously,100 mg/ kg every 6 hours for 14 days gentamycin by slow intravenousadministration, 5 mg/ kg every24 hours for 5 to 7 days metronidazole by slow intravenousadministration, 15 mg /kg every12 hours for 14 days Mouthwash with Chlorhexidine 0,2%, 10 ml 3 times daily Use honey for local dressing and for anti-bacterial action and regeneration Use intramuscular ketamine for treatment of lesions and for dressingTHIS IS A MAJOR EMERGENCY:THE PATIENT’S LIFE IS IN DANGERDO NOT DELAY! REFER THE PATIENT IMMEDIATELYTO THE NEAREST HOSPITAL OR HEALTH CENTREManagement by family and friends T ake the child as soon as possible to the hospital or health centre for propertreatment Do not hide the child at home Fully and strictly follow the instructions given by health professionals17
STAGE 4ScarringAt this stage, the acute phase is over.However, it is still important to treat the childto limit the sequelae as much as possibleand to ensure the child’s well-being.Treat the child tolimit the sequelaeand ensurehis well-beingMain signs and symptoms T rismus may occur, depending on the locationof the lesions Sequestration of teeth and exposed bones Beginning of scar formationManagement by health workersThe scarring process at this stage is highly retractile and the formationof extremely fibrous scar tissue may induce trismus and a permanentshrinkage of the mouth. Physiotherapy may preserve the mouth opening Removal of all the scabs and exeresis of necrotic tissue Extraction of all loose teethNotes .18
Medication Antibiotic treatment- O ption 1: Amoxicillin & clavulanicacid intravenously, 50 mg/ kg every6 hours for 14 days gentamycin byslow intravenous administration,5 mg /kg every 24 hours for 5 to7 days metronidazole by slowintravenous administration,15 mg/ kg every 12 hours for 14 days- O ption 2: Ampicillin intravenously,100 mg/ kg every 6 hours for 14 days gentamycin by slow intravenousadministration, 5 mg/ kg every24 hours for 5 to 7 days metronidazole by slow intravenousadministration, 15 mg /kg every12 hours for 14 days Mouthwash with Chlorhexidine 0,2%, 10 ml 3 times daily Use honey for local dressing and for anti-bacterial action and regeneration Use intramuscular ketamine for treatment of lesions and for dressingTHIS IS A EMERGENCY:THE PATIENT’S LIFE IS IN DANGERDO NOT DELAY! REFER THE PATIENT IMMEDIATELYTO THE NEAREST HOSPITAL OR HEALTH CENTREManagement by family and friends T ake the child as soon as possible to the hospital or health centre for propertreatment Do not hide the child at home Fully and strictly follow the instructions given by health professionals19
STAGE 5SequelaeAt this stage, the irreversible sequelae are present.Management here consists in improving the child’squality of life and ensuring that they live in anenvironment that is conducive to their well-being.This is the timefor reconstruction:physical,psychologicaland socialMain signs and symptoms Disfigurement Speech problems T rismus may occur, dependingon the location of the lesions Salivary leak Teeth displacement Teeth loss Dental anarchy Feeding difficultiesManagement by health workersAt the sequelae stage, reconstructive surgery in view of functionaland aesthetic rehabilitation is strongly recommended U ndertake postoperative physiotherapy to prevent the recurrenceof trismus Provide psychosocial assistance to promote social reintegration U ndertake major reconstructive surgery only when the acutephase of noma is completely over and the progression of thedisease has been definitively halted F irst ensure that the patient recovers his/her functional capacitiesand is free of trismus before embarking on aesthetic rehabilitationMedication No antibiotics if the acute phase is over20
BEFOREAFTERBEFOREAFTERProper follow-up and keeping of appointments in the course of multiple surgeries andfunctional and aesthetic rehabilitation sessions are crucial factors for the success ofsurgical treatment.Management by family and friends Go to the health centre and seek referral to a centre specializedin reconstructive surgery of noma sequelae Several surgeries may be necessary; it is therefore important to strictlyfollow the treatment plan Keep the follow-up appointments for reconstructive surgery and physiotherapysessions After returning home, continue with the physiotherapy exercises learned at thehealth centre Ensure proper nutrition and practice sound oral hygiene Provide an environment that is conducive to the child’s well-being, where he/shefeels loved, is able to make friends and can receive a proper educationBEFOREAFTERBEFOREAFTERNotes .21
In addition to this information brochure, the following poster wasdesigned to be posted in health centresNOMA is a severe diseaseIt can be treated if detected early!noma is not a contagiousdisease, is not transmitted fromone person to another is not caused by witchcraftfirst action:or a curse on parentsopen and examinechildren’s mouthsPersonsat-risk: mostlySigns and symptomsat the very beginningof the diseasechildren aged 2 to 6 yearsliving in conditionsof malnutritionand extreme poverty Reddened, swollengums that bleedspontaneously orwhen touchedWhat are thewarning signs Fetid breath Excessive salivation Sore, lesion insidethe mouththe 5 stages of the diseasefor early detection? Watch out when a child’s mouth isclosed and he/she hypersalivatesand emits fetid breath with a putridsmell, regardless of whether he/shehas fever or not1Acute necrotizinggingivitis stage4The electronic version of the poster is available at thefollowing URL: a stageScarring stageNon communicable Diseases Cluster (NCD)regional Programme for noma control53Gangrenous stageSequelae stageWith the support of WHO Regional Office for Africa, 2016. All rights reserved.The electronic version of the poster is available atthe following URL: http://apps.who.int/iris/handle/10665/25458022
Notes .
Republic of Congo (Tel: 47 241 39100; Fax: 47 241 39507; E-mail: afrgoafrobooks@who.int). Requests . without warranty of any kind, either express or implied. The responsibility for the interpretation and . noma is not transmitted from one person to another; noma is not a contagious disease!