Transcription
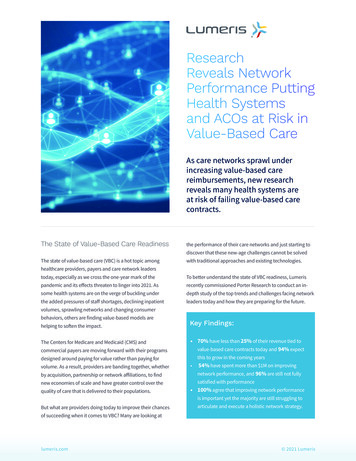
ResearchReveals NetworkPerformance PuttingHealth Systemsand ACOs at Risk inValue-Based CareAs care networks sprawl underincreasing value-based carereimbursements, new researchreveals many health systems areat risk of failing value-based carecontracts.The State of Value-Based Care Readinessthe performance of their care networks and just starting todiscover that these new-age challenges cannot be solvedThe state of value-based care (VBC) is a hot topic amongwith traditional approaches and existing technologies.healthcare providers, payers and care network leaderstoday, especially as we cross the one-year mark of theTo better understand the state of VBC readiness, Lumerispandemic and its effects threaten to linger into 2021. Asrecently commissioned Porter Research to conduct an in-some health systems are on the verge of buckling underdepth study of the top trends and challenges facing networkthe added pressures of staff shortages, declining inpatientleaders today and how they are preparing for the future.volumes, sprawling networks and changing consumerbehaviors, others are finding value-based models arehelping to soften the impact.The Centers for Medicare and Medicaid (CMS) andcommercial payers are moving forward with their programsKey Findings: 70% have less than 25% of their revenue tied tovalue-based care contracts today and 94% expectthis to grow in the coming yearsdesigned around paying for value rather than paying forby acquisition, partnership or network affiliations, to find54% have spent more than 1M on improvingnetwork performance, and 96% are still not fullynew economies of scale and have greater control over thesatisfied with performancevolume. As a result, providers are banding together, whetherquality of care that is delivered to their populations. 100% agree that improving network performanceis important yet the majority are still struggling toBut what are providers doing today to improve their chancesarticulate and execute a holistic network strategy.of succeeding when it comes to VBC? Many are looking atlumeris.com 2021 Lumeris
The State of Network Performancefor care networks, particularly when the entire network isThe shift toward value-based care is accelerating in partdesigned to address shared savings models or the uniquedue to the pandemic, as health system leaders look for newdemands of accountable care organizations (ACOs) thatways to reduce the cost of care and share the responsibilitystretch across populations, care settings and providerof keeping patients healthier. This is evident not only in theentities.not on the same EHR platform. These platforms were notPorter Research findings, with 94% expecting an increase inthe percentage of their revenue that will be tied to value-A chief operating officer of a regional health system in Newbased contracts; but also, as described in a March 2021York shared his perspective on these challenges: “We are stillModern Healthcare CEO Power Panel survey where three-evolving when it comes to building a cohesive strategy forquarters of CEOs plan to take on more value-based contractsinfluence network performance. We’ve been trying to buildas a result of the COVID-19 crisis.better tools to help us monitor the network, but it is difficult1given the fact that we have practices and hospitals thatAs the percentage of value-based revenue grows, so doesaren’t on the same EHR system. Without having a commonthe importance of the network performance. Value-basedplatform, it is extremely challenging.”contracts only work if all participants clearly understand thegoals, are aligned around common incentives and are ableto share both clinical and performance data to optimize theTop Challengesnetwork.Despite their best efforts and the millions of dollars beinginvested in network performance and interoperability, 96%Among Porter Research surveyrespondents who are participatingin some form of value-based carearrangements today, the majorityhave signed population-basedshared savings (70%) and shared/loss (66%) contracts.of survey respondents are still not fully satisfied with theircurrent network performance.“The ability to get the big picture and also be able to drilldown to see current practice-level specifics of their networkis the ultimate challenge facing organizations today”observed Amanda Surber, Lumeris Vice President ProductStrategy and New Markets, “and becomes even more criticalas they look to shift into value.”From a technology standpoint, data is often locked away inWhile many organizations are still early in theirsiloed systems, requiring massive investments of money andtransformation to VBC, their current approaches do nottime to access. This makes it nearly impossible for networkappear to be working as they try to overcome the initialleaders to have timely access to the data to help themchallenges that are sure to grow as VBC-based revenuesmeasure and monitor network performance. Unfortunately,grow. So, what are most providers doing today?many health systems are turning to existing technologysolutions, such as their EHR systems and standard reportingAccording to the survey, many networks (60%) havemodules, to get access to what they need. And they’reintroduced provider incentives that align with performancecoming up short.goals, and 52% have created special onboarding andtraining programs to ensure their providers understandProviders are also spending millions of dollars trying towhat is expected.get these traditional tools to talk to each other under thepremise of interoperability. But as budgets tighten due to2The vast majority (88%) are turning to traditional tools,the massive disruption COVID-19 has brought to our healthlike their electronic health record (EHR) systems, for datasystems, IT integration budgets and projects are often thereporting and analytics. This introduces significant riskfirst line items to be cut. 2021 Lumerislumeris.com
Current Investments to Improve Network Performance96%1007560%60%5036%24%25Analytics andmonitoringIT integrationservicesOperationalsupportReferral workflowsolutionsConsultingservicesAccording to one SVP of Finance at a large academic medicalgrowing expense in 2021.2 This one-dimensional, manual-center in the Midwest, “We’ve made major investments inintensive strategy flies in the face of the goal of movinganalytics tools, and we were on the cusp of turning thosetoward electronic, more efficient means of delivering higheron when COVID hit. A lot of things have been sidetrackedquality healthcare.because of COVID, and our efforts have now stalled. I’d sayAs organizations seek a “silver bullet” to help improvewe are now about a year and a half behind on starting to getnetwork performance, the current solutions they arethe insights we need to more actively manage our network.”applying are disconnected and are not able to answerfundamental questions such as, “Why are patients receivingAnother chief medical officer from a mid-sized health systemcare outside of the network? Why are my care costs soin Tennessee commented, “We had plans to purchase moreinconsistent? What types of providers do we need to add topurpose-built technologies to help us optimize our network,the network?”but all of our financial spending right now is on a freeze dueto the pandemic. We hope to get back on track soon so wecan have access to the data we need to make better networkdecisions.”Lack of access to data also makes it challenging for providersunderstand where and why network leakage is occurring.This not only results in lost revenue opportunities, but alsoinhibits the system’s ability to control care costs and qualityas patients move through alternate care sites.Other providers are throwing people at the problem, tryingto onboard, educate and incent providers at record speeds.While the onboarding process is important, constantattention to each provider can require a massive investmentin human resources – both clinical and non-clinical. In fact,according to the Modern Healthcare CEO Power Panel, 63%of the panel expects staffing and labor to be their fastest-lumeris.com“We’ve made major investmentsin analytics tools, and we were onthe cusp of turning those on whenCOVID hit. A lot of things have beensidetracked because of COVID,and our efforts have now stalled.I’d say we are now about a yearand a half behind on starting toget the insights we need to moreactively manage our network.” SVP of Finance at a large academicmedical center in the Midwest 2021 Lumeris3
Biggest Network Performance Challenges67%Lack timely/accurate datato track network performance67%High levels of network leakage40%47%Unable to effectively managethe referral process/policiesProvider incentives not alignedto performanceTo build a sustainable network, leaders must focus on allthree main areas of network performance:PeopleProcessTechnologyThis three-pillar approach can also promote multipledividends. Lumeris enables health systems to optimizenetwork performance through best practices, governanceand communication frameworks and fit-for purposetechnology. While designed to increase care retentionand network integrity, these integrated components canalso help enhance patient access and foster safer morecoordinated care priming the organization for a future shiftto value-based care.4 2021 Lumeris47%Inability to measure/monitornetwork performance20%Lack of network integrity/coveragePositive Impact For Patients andProvidersImproved brand perception in the community and growthin the number of patients receiving care in the network arealso biproducts of a high-performing care network. Thisnot only helps those providers who have more revenuetied to value-based contracts, but it also helps participatingnetwork partners who are still heavily dependent on fee-forservice revenue, such as post-acute care providers.Addressing issues such as network leakage and careretention can provide both short and long term benefitsfor these providers. It can spark an immediate revenuebump by increasing care contained within the network andimproving care coordination, and foster high-performancein value-based contracts by reducing cost and improvingcare quality.lumeris.com
Top Positive Impact Points for Value-Based Care70%7556%50%50%Increasing the diversificationof your organization’scontract portfolioIncreasing themarketability of yourorganization’s network5025Revenue supportCorporate strategicinitiativesWhen networks are optimized, everyone wins. PatientsTaking a holistic approach is the secret to sustainableget greater access to quality care services and providersnetwork success:reap the financial benefits of positive performance. Surveyrespondents have big aspirations for the role that valuebased care will play in their future success.1People/Strategy Advisory: As many networks are atthe beginning of their value-based care journeys,now is the time to establish a flexible approachand partnerships that can help them navigateThree Things Every Network LeaderMust Consider in 2021the rapidly changing market dynamics. LumerisHealthcare consumer preferences and behaviors areperforms a deep dive assessment that looks at thechanging at never-before-thought-of speeds due toCOVID-19, which in turn is driving the expansion of carenetworks. As these networks expand, so do the complexitiesof trying to optimize performance. New providers requireeducation and onboarding and introduce more risks ofnetwork leakage if not handled properly. More entities withdifferent EHR systems and varying degrees of maturity comeworks as collaborative operating partner withhealth systems. As part of its solutions, Lumerisnetwork holistically- from the system level downto the practice and provider level. Lumeris workswith the health system to define a strategic planfor optimizing their network performance that ismanaged on an ongoing basis to stay in step withthe organization, with Lumeris working side-by-sidewith the health system.into the fold.lumeris.com 2021 Lumeris5
2Process/operational expertise: CIOs, CMOs, CFOs,COOs and CEOs must work together more closelythan ever before to ensure network performance,contract performance and clinical best practicesare aligned properly. This can be complicated asgovernance structures are constantly evolving asthe network expands. Aligning with an organizationwho has deep domain expertise and works withmany other care networks can give leaders valuableinsight into best practices for running complex carenetworks. Leveraging over a decade of practicalexperience in managing value-based care contracts,“Organizations need to movebeyond traditional tools designedfor volume and incorporate a moreholistic approach that can scalewith the network performancedemands of risk-based strategies.”- Amanda Surber, Lumeris VicePresident Product Strategy andNew Markets.including running a high-performing MedicareAdvantage plan, Lumeris helps organizations buildtheir contracting strategy, optimize utilizationA Step in the Right Directionand implement network design and governancestructures designed to enhance their networkProviders must consider a more modern approach toperformance. In doing so, Lumeris enables healthaddressing these emerging challenges or risk failing whensystems to deliver high-performance today and beit comes to value-based care contracts. The precariouspositioned for future success in risk-based contracts.position that our US healthcare system is in due to COVID-19requires leaders to think more holistically and leverage3Technology and Services: Major technologyinnovations are taking place to address the newexperienced resources to help guide them through theseunchartered territories.challenges triggered by the COVID-19 crisis, andproviders should not depend on traditional tools,such as their EHR systems, alone. Lumeris enterprisesolutions enable organizations to utilize theirexisting systems and provide an EHR-agnosticcentralized platform for managing their value-basedcare. The Lumeris platform enables health systemsto integrate information from across the network,including employed and independent providers andspecialists.For any solution to be most effective, empoweringpeople with the knowledge of how to properly usethe technology and data to optimize the networkperformance also must be considered. Lumerisutilizes a physician-led, patient-centered approachbased on insights and experience gained over 15years of managing value-based contracts. Togetherwith a proven model for VBC, Lumeris arms healthsystems with the tools, best practices and know-howto build a sustainable framework for managing ahigh-performance network and improving patientoutcomes.6 2021 Lumerislumeris.com
MethodologyThe research involved a quantitative survey ofapproximately 50 clinical and business executives,including CEOs, CMOs, CFOs, COOs, from healthsystems and ACOs as well as a series of qualitativephone interviews conducted by Porter Research. Thefindings have been incorporated into this paper toenable network governance teams to be more preparedwhile leading their organizations into the future of VBC.About LumerisLumeris enables a new model for Value-Based Care. As the trusted partner for next-generation health systems, Lumeris helpsproviders deliver extraordinary clinical and financial outcomes. With health systems partners across the country, we alignproviders and payers with a proven model that coordinates operational processes, resources and technology to achieve highquality, cost-effective care with very satisfied consumers and engaged physicians. Lumeris is a proven operating partner forhealth systems moving toward Value-Based Care and total cost of care management. Lumeris brings a broad set of best-inindustry operating capabilities, deep expertise in managing insurance risk, and a highly aligned business model to its healthsystems partners. Lumeris is focused on enabling health systems to create sustainable, scalable, high-performing healthcaredelivery systems in local communities across the country. To learn more, visit: https://www.lumeris.com.For more information go tolumeris.comEnd lumeris.com 2021 Lumeris7
Biggest Network Performance Challenges To build a sustainable network, leaders must focus on all three main areas of network performance: People Process Technology This three-pillar approach can also promote multiple dividends. Lumeris enables health systems to optimize network performance through best practices, governance