Transcription
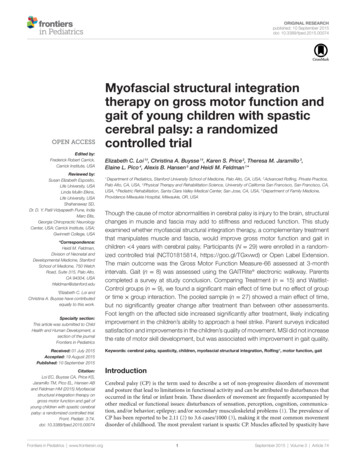
Should Dry Needling for MyofascialPain be Within the Scope of Practicefor Physical Therapists?Sinéad A. FitzGibbon, PT, MSDoctoral Student, graduate program in Orthopedic and Sports Physical Therapy, Rocky Mountain University of Health Professions, Provo, UT &Co-owner Manual and Sports Physical Therapy, Sag Harbor, NYINTRODUCTIONHealth care expenditure in the UnitedStates reached 2.2 trillion in 2007, increasing 6.2% from the previous year, andamounted to 16.2 % of the gross domesticproduct.1 Professional services, includingphysical therapy, accounted for 62 billionof this cost.1 Myofascial pain is one of theleading complaints of patients presenting ingeneral medical practice, with reported prevalence of 20% to 93% in general practice2,3thus imposing significant financial burdenson state and national health care budgets.3With high prevalence and associated costs,there is unrelenting pressure on insurers,clinicians, and researchers to reduce costswhile optimizing outcomes. The physicaltherapy profession is at the forefront of costcontainment by promoting comparisons ofthe effectiveness of different interventionsin management of musculoskeletal pain.4Physical therapists use nonsurgical, nonpharmaceutical modalities in the prevention and treatment of disability.5 Moreover,the 2020 vision statement of the American Physical Therapy Association (APTA)reflects the emerging priorities of the profession by emphasizing the provision of expertcare using evidence-based practice.6 With44 states allowing direct access to physicaltherapists (PTs) at a lower cost than physical therapy via physician referral,7 PTs are apart of the vanguard of cost containment inhealth care.Physiotherapists began musculoskeletalcare in 1894 as a group of nurses practicingremedial massage in the United Kingdom(UK), and evolved into established professional organizations on both sides of theAtlantic. Today there are 170,000 practicingPTs in the United States and 36,000 chartered physiotherapists in the United Kingdom, with therapists recognized as expertclinicians in management of musculoskeletal and myofascial pain.8,9Physiotherapists practicing internationally in the United Kingdom, Australia, NewZealand, and throughout Europe use dryneedling alongside traditional modalitiesin management of myofascial pain.10-12 Themultimodal, direct access practice modelis beneficial to both the consumer and theclinical practitioner, as well as cost effectivefor all involved parties.7 There are growing numbers of national and internationalcourses in dry needling for physical therapists,13-15 with 5,500 physiotherapists in theUK16 and over a thousand such therapists inAustralia17 now licensed to use needling inphysical therapy practice.Direct access to physical therapy givespatients suffering from myofascial paina gateway into a broad spectrum of painmanagement techniques. Physical therapyprofessionals are expert first-line cliniciansin delivery of pain management modalities. With inclusion of dry needling in thebattery of techniques available to skilledclinicians, cost-effective nonsurgical painmanagement options could improve patientoutcomes and contribute to containinghealth care costs. In order to understandhow dry needling by physical therapistscan enhance pain management, knowledgeof its history and current use is warranted.This paper will outline the background ofthe trigger point theory and describe dryneedling as used in management of myofascial pain. It will then compare and contrastthe educational processes of acupuncturistsand physical therapists with regard to use ofneedling. Finally, the case will be made forbroadening the physical therapist’s scope ofpractice to include dry needling, with specialreference to use of evidence-based practicein the current fiscally challenging medicalenvironment.DRY NEEDLING: BACKGROUNDDry needling, generally understoodas the insertion of filiform (fine filament)needles without use of saline or other liquidsubstances, has its roots in ancient practiceof acupuncture. Nearly 3,000 years of Chinese acupuncture has resulted in regionalAsian variations in technique and ideology.18,19 Development of modern Chinesemedical and therapeutic practices has com212bined with western empirical medical practices to result in the practice of dry needling.This is the use of filiform needles to treatmyofascial trigger points without referenceto oriental medicine philosophy and principles of practice. Dr. Janet Travell developedand popularized the treatment of myofascialtrigger points (MTrP) using dry needlingtechniques.20,21 This method of myofascial pain management has become popular among physical therapists and medicaldoctors worldwide, especially over the past3 decades. Histopathology, electrical activity, neurophysiology and clinical features ofMTrPs have been studied since the 1940s,and though this body of knowledge continues to grow, the mode of efficacy of needlingMTrPs remains poorly understood.Myofascial Trigger Points, Definitions,and Mode of EfficacyA MTrP is defined as a highly localized and hyper-irritable spot in a palpabletaut band of skeletal muscle tissue.22 Themain criteria used for diagnosis of MTrPsare the following: a tender spot in a tautband of contractile skeletal muscle, patientpain report upon palpation of this point,a predictable pattern of referred pain frompalpation of this point, and a local twitchresponse elicited upon palpation.3 Despitewidespread use of these criteria, there havebeen few studies that have examined interexaminer reliability and diagnostic sensitivity and specificity,3,23-24 nor has there beenstandardization of the manner in which theexamination is conducted.21TRIGGER POINT THEORY ANDNEEDLING RESPONSETrigger points are known to occur andto be maintained at the level of a spinal segmental reflex.2 It is thought that excessivelocal release of acetylcholine2 or calcium22at the neuro-motor endplate results inspontaneous electrical activity (SEA), withsustained depolarization and shortening ofsarcomeres.21 The resultant prolonged localmuscle spasm is thought to impair bloodOrthopaedic Practice Vol. 23;4:11
flow, cause tissue damage, and perpetuatean inflammatory cycle.2,21,22 To date, therapyhas been aimed at inhibiting muscle spasmand reducing the pain of MTrPs using manymodalities, including spraying with ethylchloride followed by specific stretching, deepmassage, injection of various substances, anddry needling.2,21,25 Elicitation of local twitchresponse has been demonstrated to occurwith needle insertion into active MTrPs.2,21,26Pain relief is associated with reduced electrical activity following needle insertion intoan MTrP in which a twitch response isobserved.21,22,26,27 Activation of spinal endogenous opioids is a likely factor in the effectiveness of many therapeutic interventionsin pain management. Direct stimulation ofperipheral nociceptors by needling may actto desensitize the central nervous systemvia SEA endplate inhibition and enhancestimulation of opioid activity within spinalwide-range dynamic neurons.22,28 Whileacupuncture and dry needling are theorizedto have similar mechanisms of action, theeducation, philosophy of practice, and techniques are quite dissimilar.COMPARING ACUPUNCTURE ANDDRY NEEDLINGAcupuncture is one of the oldest forms oftherapy, and is based on Chinese philosophy,namely that disease is an outward manifestation of internal imbalance of Yin and Yangenergetic forces.18 Although filiform needlesare used in both dry needling and acupuncture, the similarities are limited. Whereasacupuncture is used to diagnose and managesystemic conditions, dry needling of myofascial trigger points purportedly targetsspecific tissue responses without reference toenergetic systems.22, 27 Acupuncture education entails 3 years of study with mentoredresidency and competency examinations.Dry needling certification is adjunctive to amedical degree, or a physical therapy masters or doctoral qualification, which takes5 to 7 years of study. Certification for dryneedling in the United States occurs after 50hours of post-graduate coursework and 200to 400 documented interventions. Competency examination is required in the UnitedKingdom, Europe, and Australia with someprograms demanding rigorous dissertationsat the culmination of a full academic year ofacupuncture related physiotherapy.29 Suchcompetency exams are similar in depth toAPTA board certification areas such as orthopaedic sports, and women’s health physicaltherapy certifications. Medical doctors andOrthopaedic Practice Vol. 23;4:11physical therapists practice dry needlingwhen it is determined to be within the scopeof practice by their relevant states. Availableevidence for efficacy of acupuncture anddry needling in myofascial pain is limited,and conclusive results are few.18,19,25,30 Moststudies have been limited by small samplesize, nonstandardization of techniques andpoor research design, with few high qualitystudies or systematic reviews. The majority of published manuscripts investigatingthe effects of acupuncture and needlingunderscore the need for high quality clinicalresearch in this area.18,30-32Dry Needling Within the Scope ofPhysical Therapy PracticeCanada, the United Kingdom, Ireland,the Netherlands, Norway, Switzerland, Belgium, Spain, Chile, South Africa, Australia,and New Zealand, among other nations,and some 18 states in the United States havedetermined that dry needling techniques fallwithin the scope of physical therapy practice.33,34 Other states such as California, NewYork, North Carolina, Hawaii, and Tennessee have proscribed the practice outright.35In order to understand the potential benefitsand risks of amending state practice acts, thearguments of the stakeholders on both sidesneed to be addressed.ACUPUNCTURISTSAcupuncturists have been licensed topractice in the US since 197336 and manyprograms obtained national certification in1982,37 culminating in 16,000 acupuncturists currently in practice38 nationwide.Forty-three states require certification forlicensure.39 Acupuncture practitionershave been opposed to the inclusion of dryneedling in physical therapy practice actsin Virginia and Colorado40,41 and otherstates.35 Their objections are based on theduration of the needling certification programs, concerns for the safety of patientsand encroachment on professional territoryby physical therapists.35,40,41 with resultantspecific criteria changes to the practice actsin these states. Acupuncture professionalassociations claim that physical therapistscan become certified in dry needling techniques with a course of only 54 hours, whilethe majority of acupuncture certificationprograms have requirements of 1,90542 to3,000 hours of education from some 57accredited programs.35,43 This claim disguisesthe fact that dry needling certification is apostgraduate course following graduation213from one of 200 masters or doctoral physical therapy programs that receive accreditation from the Commission on Accreditationin Physical Therapy Education (CAPTE).44Entry-level DPT programs typically comprise 2,676 hours of education33,45 and amore extensive anatomy component thanacupuncture programs.33Concern for patient safety is not withoutmerit, since skin penetration carries risk ofinfection, disease transmission, and potential injury to soft tissue, nerve, and bloodvessels. However, there is no documentedevidence of increased litigation involvingtherapists practicing dry needling or otherskin penetration techniques in states wherethis is allowed.46,47 Regarding the territorial concerns, acupuncture practitionersare concerned that the use of dry needlingby physical therapists encroaches on theirprofessional practice grounds. Dry needling has been identified as a componentof acupuncture practice, with acupuncturists invited to participate and teach on dryneedling courses.14,46 However, dry needlingpractitioners limit their practice to management of MTrPs, with no claim to diagnosisor management of systemic disease processes. Diagnosis and treatment of conditions using oriental medicine techniquesremains the domain of the acupuncture andoriental medicine professions, and this isaffirmed by physical therapy practitionersteaching courses in the United States andinternationally.46PHYSICIANSPhysicians in particular, have been concerned about skin penetration by physicaltherapists, objecting to the use of electromyography (EMG) by physical therapistsdespite the inclusion of such procedures inmany state physical therapy practice acts fordecades.33,46,48 Several states license physicaltherapists to use skin penetration in EMGtesting,33 and to date there has been nodocumentation of any injuries or healthhazards for such therapists.33,46 Insurancecompanies providing liability coverage forphysical therapists practicing dry needlingimpose no additional requirements, otherthan that they practice in a state that permitsthe technique.47CHIROPRACTORSThe Maryland chiropractic professiontook an interesting position towards dryneedling, initially opposing dry needling,determining that it fell within the regulatory
practices of the state board of Acupuncture.However, the Maryland Chiropractic Boardreversed its position in 2007 and allowedchiropractors to use dry needling under theirphysical therapy privileges, since the physical therapists in the state had been licensedto do so since 1987. As in other states andinternational communities, acupuncture isdetermined to be “the use of oriental medical therapies for the purpose of normalizingenergetic physiological functions includingpain control, and for the promotion, maintenance, and restoration of health.36,41,49The Maryland Chiropractic Board rulingwas based on the fact that acupuncture usesneedle insertion into fixed points and isbased on pre-scientific philosophies, whereasdry needling into myofascial trigger points issolely a local soft-tissue technique. Thus dryneedling is not based on Chinese philosophy of energetic systems, does not constituteacupuncture, and is therefore not subject tothe regulation of the acupuncture licensingboards.49PHYSICAL THERAPISTSThe APTA is the national professionalorganization of 72,000 physical therapists inthe United States.8 The APTA does not yethave an official position on dry needling byphysical therapists, but recognizes that it isa technique being used by some of its members.50 The APTA acknowledges that statelicensing boards, which have jurisdictionover administration of each state’s PT act,have been consulted regarding whether dryneedling falls within the scope of practice.The answer across the states is mixed, with5 states explicitly proscribing dry needling(NV, NY, NC, ID, TN), stating that it isnot in the scope of practice. Fifteen boardshave interpretive opinions that it is withinthe scope of practice in states allowing it,and there have been no definitive statementsby the remaining 32. Arizona and Pennsylvania are legally prohibited from issuingan interpretive statement. Statements byphysical therapy boards in the 18 states thathave amended the scope of PT practice toinclude dry needling include language stipulating that neither the state medical boardnor the acupuncture board could rule on theeligibility of appropriately trained physicaltherapists to practice dry needling.51,52 Somestates issue contradictory statements. Forexample, Florida proscribes “skin penetration” in dry needling by physical therapists,but allows them to perform and analyzeEMGs, which by definition involves skinpenetration. Tennessee takes the positionthat since no academic institutions in thatstate teach dry needling to physical therapystudents, it should remain outside of thescope of PT practice.33 This introduces thedilemma of what to do once dry needlingis part of entry-level DPT programs, as itis currently at Georgia State University,53for example. It may be time to encouragea national review of the scope of practicefor physical therapists. A recent report bythe Federation of State Boards of PhysicalTherapy (FSBPT) outlines that there is ahistoric basis, education and training, anda scientific basis for use of dry needling byphysical therapists, provided competencyis determined to ensure safe practice.54 TheFSBPT conducts an analysis every 5 yearsto determine actual practices within the profession. Also, the highly respected AmericanAcademy of Orthopedic Manual Therapistssupports dry needling in the PT scope ofpractice and indicates that research supports its use.55 As with any policy or practicechange, the process is likely to be slow andpiecemeal in nature, but gradual implementation of such changes can facilitate reflection and necessary critical analysis. In orderto reflect on the possibility of changing thescope of practice of physical therapists, itis important to understand the process bywhich practice guidelines are determined.Determining the Scope of Practice forthe Physical TherapistsIn the United States, state physicaltherapy boards determine the legal scope ofphysical therapy practice in each state. TheFederation of State Boards of Physical Therapy (FSBPT) Model Practice Act provideslanguage to states for reference and consideration in the development of their individualpractice acts. In evaluating the current climate of health care practice and education,the FSBPT recognizes the overlap of manyskills and procedures among professions,stating that it is “no longer reasonable toexpect each profession to have a completelyunique scope of practice.”54 Devised with thecollaboration of the medical, nursing, socialwork, pharmacist, occupational and physical therapy professional communities, theFSBPT document provides a protocol forstate boards to use in decision making aboutwhether an intervention should be includedin the scope of practice. This protocol assistsin decision-making when considering practice act changes, with the primary focus onwhether the proposed changes “will better214protect and enhance consumers’ access tocompetent health care services.”54 Proposedchanges to the scope of practice shouldevaluate 4 critical areas: established historyof specific practices, adequate training, adequate evidence of benefit to public health,and appropriate regulation. The FSBPTmaintains that adequate evidence in eachof these areas suggests that scope of practicechanges would be in the public’s best interest.54 This position echoes that of the Federation of State Medical Boards (FSMB), anallied, parallel organization for physiciansand osteopaths. This group outlines themultifactorial nature of scope of practicedecisions, including workforce needs andavailability, financial motivations, economiccircumstances, and consumer demand, withthe ultimate goal of protecting public healthand safety.56 In order for there to be a rational, useful approach to broadening the scopeof practice of a health care practitioner, theremust be judicious use of the guidelines thathave been developed for this purpose.Guidelines for Changes to the Scope ofPracticeAccording to the FSBPT and the FSMB,scope of practice should be reviewed whenthe following factors have been considered:where there exists a need for the proposedscope of practice; when the existing scopesof practice, if altered, will result in a positive change in public health and safety;where there exists formal education, training, and accreditation processes for thechange in scope of practice; where appropriate evaluation and disciplinary proceduresare established; where accountability andliability issues have been clarified and wherethe effects on other practitioners have beenreviewed.54,56 Using these criteria, the broadening of the scope of practice for physicaltherapists to include dry needling, would beapproved. First, more than a third of the USphysical therapy boards have issued interpretations that dry needling is within the PTscope of practice. Such changes in physical therapy state practice acts parallel thepractices of Canada and many countries inEurope, Asia, and South America. Second,there has been no increased incidence ofinjury to the health of patients when managed by physical therapists who use techniques that puncture the skin. Third, thereare 3 main US programs for accredited needling education programs, and reciprocityalready exists among the international programs for dry needling certification. Fourth,Orthopaedic Practice Vol. 23;4:11
physical therapists practicing dry needlingare accountable under standard rules ofpractice, and have the same requirements tocarry malpractice and liability insurance asthose who do not practice needling. Finally,there is no documented adverse financialeffect on other practitioners when physicaltherapists are licensed to practice dry needling. In fact, there may be an opportunityfor both acupuncturists and physical therapists to improve their position in the marketif both groups could market their nonsurgical, nonpharmaceutical approach to painmanagement.Planning or Policy Strategies that MightMitigate DifferencesIn negotiations, success results from collaborative efforts to resolve any impasse.57The APTA and the American Associationof Acupuncture and Oriental Medicine(AAAOM) could collaborate on combinedstatements, with a unified marketing campaign for consumer education to differentiate between acupuncture and dry needling.University programs for dry needling couldbe developed in collaboration with all interested parties.33,58 Combined physical therapist and acupuncturist lobbying for thirdparty payor reimbursement could be moresuccessful than the current situation whereeach professional community struggles forreimbursement independently.59,60 Benefits could include improved teamwork ofmedical doctors, physical therapists, andacupuncturists to optimize patient care.Reduced costs for the consumer could resultas all providers compete in the open marketfor myofascial pain management services. Ascontinued research would determine bestpractices, collaborating professionals wouldbe quick in adjusting their practice to reflectnew knowledge. The concept of an extendedscope of practice for physical therapists is notan expansion of physical therapists interestin needling therapy, but is a component of aglobal shift in health care service utilization.Extended Scope of Practice in HealthCare ProfessionsAn international summit on advancedscope of practice and direct access to physical therapy was held in Washington in October 2009 to examine current internationaldemands and practices, and to determinethe implications of increased practice scopeon interprofessional relationships, professional boundaries, and role definitions.61National and international developmentsOrthopaedic Practice Vol. 23;4:11to alter the scope of practice of physicaltherapists and other medical professionalsare underway, in order to mitigate the current stresses on the health care system.54,56,61These scope of practice changes follow thedevelopment of the nurse practitioner andphysician assistant professions, whose origins as legitimate medical professionals grew,in the past 50 years, out of the financial andworkforce constraints on the general physician and medical community.62,63 Physical therapists are currently being trained injoint injections,64 musculoskeletal triage inemergency rooms,65 and first-line health caremanagement.66 The changing tide of clinicalpractice is not likely to reverse, as increasing demands on finite financial resourcescontinue.1SUMMARYCurrent US and International Practice,Recommendations for the FutureDry needling is already within the scopeof physical therapy practice in many areas(18 US states34); skin penetration by physical therapists for EMG is allowed in manyUS states, and Canada, South America,Europe, Asia, Australia, and New Zealand.With minimal risk and increased benefits tothe majority of stakeholders, dry needlingpracticed within an increased scope of PTprofessionals will be of benefit to the public,bringing American clinicians in-line withtheir international colleagues.The APTA’s “2020 vision” for physical therapy includes a commitment to lifelong learning with use of evidence-basedpractice.6 Articles published in respected,peer-reviewed journals underscore the continued need for expert clinicians to critically appraise and conduct research. Thecurrent emphasis in physical therapy education is on research to support and challenge clinical practices. With increasinguse of dry needling by physical therapists,the research emphasis should include dryneedling within efficacy and comparativeeffectiveness studies. Doctoral level physicaltherapists who acquire these skills as part oftheir core curricula67 are well suited for such215analysis and research, and their dissertationscould explore the comparative effectivenessof dry needling and other manual therapytechniques.Many techniques are not unique to a specific profession. There are ongoing battles forterritory between chiropractors and physical therapists over manipulation and jointmobilization,68,69 between athletic trainersand physical therapists over manual therapytechniques,70 with physicians and physicaltherapists performing EMG tests,71,72 andphysicians referral to in-house physical therapy practices.73,74 The global trends in healthcare management are to look broadly acrossthe professional spectrum to determinewhere patients can benefit from skilled careprovided by appropriately trained clinicians,at the lowest cost. The future objective willbe to use best practices for best outcomesand for the best financial value. The territorial battles are likely to continue, but willdiminish in intensity as adversaries competeto demonstrate optimization of outcomesand not compete over ownership of specifictechniques.CONCLUSIONSPhysical therapists are positioned asexpert clinicians in the health care community with a broad spectrum of techniquesfor nonsurgical management of musculoskeletal pain and dysfunction. Inclusion ofdry needling within the scope of PT practice will ensure further high-quality researchand clinical practice with better outcomes inthis field. Use of dry needling by qualified,licensed physical therapists will bring American physical therapy professionals in linewith current international standards of practice, and provide patients with more optionsfor management of musculoskeletal pain.In the costly arena of arthritis, movementdysfunction, and pain management, extending the physical therapy scope of practice toinclude dry needling will improve in consumer choice, increase evidence-based practice, and facilitate cost-containment.
REFERENCES1. US Department of Health and HumanServices: National health expenditurehighlights 2007. wnloads/highlights.pdf. Accessed October1, 2009.2. Wheeler AH. Myofascial pain disorders: theory to therapy. Drugs.2004;64(1):45-62.3. Tough EAM, White ARMD, Richards SP, Campbell JMD. Variabilityof Criteria Used to Diagnose Myofascial Trigger Point Pain Syndrome-Evidence From a Review of the Literature.Clinical Journal of Pain March/April.2007;23(3):278-286.4. American Physical Therapy Association. Federal Coordinating Council onComparative Effectiveness Research:Priorities for Comparative Effectiveness Research in Physical n Advocacy&Template /MembersOnly.cfm&ContentID 57765&Navmenuid 3218&Directlistcomboind D. Accessed October 1, 2009.5. New York State Education Department: Office of the Professions: Physical Therapy http://www.op.nysed.gov/article136.htm6. American Physical Therapy Association:Vision Statement for Physical Therapy 2020. http://www.apta.org/AM/Template.cfm?Section Vision 20201&Template /TaggedPage/TaggedPageDisplay. cfm&TPLID 285&ContentID 32061. Accessed October 20, 2009.7. Mitchell J, Lissovoy G. A comparisonof resourse use and cost in direct accessversus physician referral episodes ofphysical therapy. Phys Ther. 1997;77:9.8. American Physical Therapy Association: About APTA. http://www.apta.org/AM/Template.cfm?Section AboutA P T A & Te m p l a t e / Ta g g e d P a g e / Ta g g e d P a g e D i s p l a y.cfm&TPLID 41&ContentID 23725.Accessed October 1, 2009.9. Careers Research: articles/physiotherapist.htm. AccessedOctober 1, 2009.10. Australian Physiotherapy Association:Acupuncture and Dry Needling oups/acupuncture-and-dry-needling. Accessed October 1, 2009.11. New Zealand Society of : Physiotherapy Acupuncture Association of New Zealand. http://www.physiotherapy.org.nz/. Accessed October 12 2009.Acupuncture Association of CharteredPhysiotherapists: Comment of new“N.I.C.E.” guidelines for eports/PressRelease.pdf.AccessedOctober 20, 2009.Global Education of Manual TherapistsGEMt: Advancing the art and science ofphysical therapy: courses. http://www.gemtinfo.com/. Accessed October 20,2009.Myopain Seminars: setting the standards for myofascial trigger pointeducation worldwide. ml. Accessed October 12, 2009.Institute for the Study and Treatment ofPain: iSTOP: courses. http://www.istop.org/training.html. Accessed October 12,2009.Acupuncture Association of Chartered Physiotherapists: Clinical InterestGroup of the Chartered Society of Physiotherapists. http://www.aacp.org.uk/.Accessed October 12, 2009.Australian Physiotherapy Association:Acupuncture and Dry Needling Group(ADNG). cupunctureand-dry-needling Accessed September29, 2009.Furlan ADMD, van Tulder MP, CherkinDP, et al. Acupuncture and Dry-Needling for Low Back Pain: An UpdatedSystematic Review Within the Framework of the Cochrane Collaboration.Spine. 2005;30(8):944-963.World Health Organization: Acupuncture; Review and analysis
physical therapists practice dry needling when it is determined to be within the scope of practice by their relevant states. Available evidence for efficacy of acupuncture and dry needling in myofascial pain is limited, and conclusive results are few.18,19,25,30 Most studies have been limited by small sample