Transcription
Peer ReviewedPRACTICAL ONCOLOGYCANINE INSULINOMA:DIAGNOSIS, TREATMENT, &STAGINGEliza Reiss Grant, DVM, and Kristine E. Burgess, DVM, Diplomate ACVIM (Oncology)Tufts UniversityAn insulinoma is a malignant pancreatic tumor thatinappropriately secretes excessive insulin, resulting inprofound hypoglycemia.1Pancreatic tumors are classified as: Exocrine, which includes adenocarcinomas ofductular or acinar origin Endocrine, which arise from the islets ofLangerhans.Insulinomas are functional neuroendocrinetumors that originate in the beta cells of the isletsof Langerhans.1PRESENTATIONSignalmentAny breed of dog can be affected, but largebreeds tend to be overrepresented.1 While, inhumans, insulinomas affect females far morefrequently than males, there is no apparent sexpredilection in dogs.1-3 Dogs also commonlypresent with a malignant variant, while humansoften have a benign adenoma (80%).1 Insulinoma is rare in cats.4Clinical SignsMost affected dogs do not have abnormalities onphysical examination, and early clinical signs relatedto the disease can be sporadic and vague.Classically, dogs present with signs attributableto hypoglycemia, such as weakness, ataxia, extremefatigue after exercise, and collapsing episodes.Seizures can occur later in the disease process andincrease progressively in frequency and intensityover time.1Hypoglycemic episodes are often precipitatedby exercise or fasting (increased glucose utilization)as well as by the ingestion of food (stimulation ofinsulin release). Intravenous or oral administrationof glucose alleviates clinical signs. If prolongedseizure activity occurs, cerebral laminar necrosis canensue.60DIAGNOSISAside from a histologic confirmation of insulinoma,no currently available diagnostic test provides a definitive diagnosis of insulinoma. Existing techniquesmay help increase suspicion for an insulin-secretingtumor but, with most diagnostic testing, it is imperative to interpret all results in the context of thecoexisting clinical signs.Differential DiagnosisA complete work-up, including careful patienthistory, physical examination, bloodwork, anddiagnostic imaging tests, should be performed torule out other causes of hypoglycemia, such assepsis, hepatic failure, adrenal cortical insufficiency,toxin ingestion, and other forms of neoplasia.Laboratory TestsBlood GlucoseA simple fasting blood glucose level of less than40 mg/dL can suggest hyperinsulinemia, althoughcareful monitoring of a fasted dog with suspectedinsulinoma is strongly recommended due to highrisk for seizure activity.Insulin-to-Glucose RatioAdditional blood analysis evaluating the amendedinsulin-to-glucose ratio (AIGR) may be warranted. This assay capitalizes on the lack of response tophysiologic negative feedback inhibitory loopsthat decrease insulin secretion in the face of hypoglycemia in dogs with an insulinoma. A positive insulin-to-glucose ratio demonstratesan inappropriately elevated insulin level in thesetting of hypoglycemia.1 Nevertheless, an elevated AIGR is neither sensitive nor specific for the diagnosis of insulinoma.The AIGR can be elevated from insulin-producing tumors other than insulinoma or normal indogs with insulinoma.TODAY’S VETERINARY PRACTICE An Official Journal of the NAVC November/December 2016 tvpjournal.com
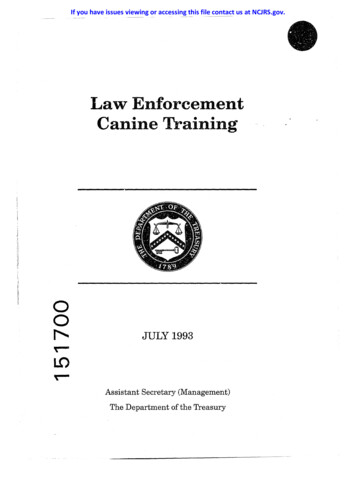
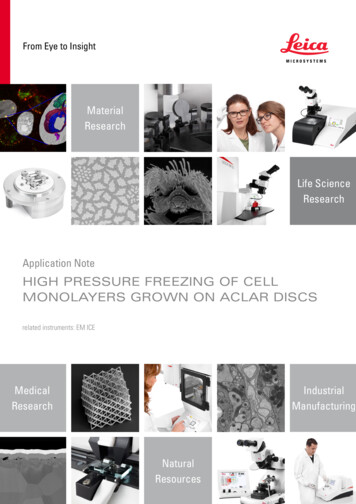
PRACTICAL ONCOLOGY This test can be performed on serum samples andsubmitted to most large commercial laboratories.Serum FructomsamineSerum fructosamine can indicate insulinoma as itmay be low in dogs with chronic or episodichypoglycemia. However, this assay is not specificand should never be considered a confirmatory test.ImagingRadiography & UltrasoundThoracic radiography and abdominal ultrasoundare recommended to assess for the presence of apossible pancreatic mass and associated metastaticdisease (eg, lymph nodes, liver, lungs). Althoughabdominal ultrasound is considered a relativelyinsensitive and nonspecific assessment for insuli-FIGURE 1. Ultrasound image of masslesion within the left wing of the pancreas.Approximately 50% of insulinomas are notvisualized by this technique.Peer Reviewednoma, it is recommended to rule out other causesof hypoglycemia. In addition, some insulinomasare large enough to be detected on ultrasound(Figure 1).Advanced ImagingConventional computed tomography (CT) withcontrast has an improved sensitivity of 71% forpancreatic lesions.5 Most recently, dual-phase CT angiography has been reported to successfully localizepancreatic lesions and stage patients before surgery(Figure 2).6Further DiagnosticsSome insulinomas are challenging to localize evenon advanced imaging, and a lack of definitive identification of the tumor on preoperative imagingshould not discredit a working diagnosis of insulinoma. In some instances, an exploratory laparotomy may be recommended when there is a strongclinical suspicion for insulinoma in the absence ofvisible disease.TREATMENTSurgical ManagementIn patients with hypoglycemia and inappropriateinsulin production, exploratory abdominal surgeryis the recommended treatment. Surgical removal ofthe tumor: Provides the best chance for relief of clinical signsand the best survival times1,2,7 Allows complete staging via biopsy of regionallymph nodes and liver to determine the extent ofsuspected metastatic disease.Metastatic DiseaseBecause dogs commonly have a malignant form ofinsulinoma, approximately half will have metastaticdisease detected before or at the time of surgery.Nevertheless, surgery is still indicated in patientswith suspected or confirmed metastatic diseasebecause removal of metastatic disease reduces theextent of aberrant insulin secretion and may improve clinical signs.1,3 RFIGURE 2. Arterial phase dorsal obliquecomputed tomography (CT) reconstruction (softtissue algorithm) of a pancreatic mass (arrow).CT angiography is a more sensitive imagingmodality for insulinoma.Surgical ApproachMost insulinomas are solitary masses that can bedetected intraoperatively with gentle palpation ofthe pancreas. Intraoperative ultrasound with IV1% methylene blue has been used for additionalvisualization of the pancreatic lesion but is of questionable value.tvpjournal.com November/December 2016 An Official Journal of the NAVC TODAY’S VETERINARY PRACTICE61
Peer ReviewedPRACTICAL ONCOLOGYPartial pancreatectomy is the preferredprocedure, with pancreatitis as a possiblepostoperative complication. Other complicationsinclude ongoing hypoglycemia, diabetesmellitus causing hyperglycemia, and neurologiccomplications from historic neuroglycopenia.Those with persistent hyperglycemia after surgeryshould be treated as diabetic until they are nolonger insulin dependent.StabilizationHypoglycemic patients should be stabilized withIV dextrose supplementation. In a crisis situation,IV dextrose should be given slowly so that furtherinsulin release is not stimulated. Glucagon, a peptidehormone produced by the pancreas, opposes the effects of insulin by raising blood glucose. It has beenused to stabilize hypoglycemia in a crisis settingwhen given as a constant rate infusion at approximately 10 to 15 ng/kg per minute.8Medical ManagementMedical management of insulinoma is possiblein patients: That are not good surgical candidates Whose owners are not interested in pursuingsurgery That have persistent hypoglycemia after surgery.This approach includes dietary management aswell as medications, such as prednisone, diazoxide,and octreotide.1,2,7Dietary ManagementThe goal of dietary management is to maintainappropriate blood glucose levels throughout the dayand avoid foods that may incite a spike in insulinrelease. This is achieved by feeding multiple smallmeals throughout the day and using foods that arehigh in protein, fat, and complex carbohydrates.Oral prednisone can be used as an adjunctivetherapy because glucocorticoids decrease insulinsensitivity and increase endogenous (hepatic)glucose production. Prednisone can be dosed toeffect in the range of 0.5 to 4 mg/kg Q 24 H.1,2DiazoxideDiazoxide is used in the medical management ofhypoglycemia to inhibit the intracellular release ofionized calcium, thereby preventing the exocytosisrelease of insulin by the beta cells. It also contributesto hyperglycemia through its ability to stimulatethe release of epinephrine. Diazoxide is commonlyinstituted in patients that do not respond to dietarymanagement and prednisone.INSULINOMA: Staging & PrognosisInsulinoma is classified as: Stage I: Insulinoma confined to pancreas Stage II: Insulinoma with regional lymph node metastasis Stage III: Insulinoma with distant metastasis.Reported insulinoma survival times are listed in the Table.TABLE.Insulinoma Survival Times Reported in the Literature: 1993 – on et al (2007)2MST: Stage I: 785 dStage II: 547 dStage III: 217 dPolton et al (2007)2Polton et al (2007)2Tobin et al (1999)7Tobin et al (1999)7Trifonidou et al (1998)3MST: 258 dMDFI: 244 dMST: 196 dMST: 74 dMST: 785 dMST: 381 dDunn et al (1993)16MST: 14 moADJUVANTTHERAPY(STREPTOZOTOCIN)Northrup et al (2013)12(all stages):MPFS: 196 dMST: 308 dMoore et al (2002)11(stage II or III)MTN: 163 dMDFI median disease free interval; MPFS median progression free survival; MST mediansurvival time; MTN median time of normoglycemia62TODAY’S VETERINARY PRACTICE An Official Journal of the NAVC November/December 2016 tvpjournal.com
PRACTICAL ONCOLOGYThe dose of diazoxide for dogs with insulinomaand refractory hypoglycemia has been reported tobe 5 to 10 mg/kg PO Q 12 H.1,7 The ideal dose fora clinical patient can be determined on the basis ofsuccessful management of clinical signs.OctreotideOctreotide is also used to manage hypoglycemiain both humans and dogs with insulinoma. Thissomatostatin analog can be given as an SC, IM, orIV injection. Inhibition of insulin release is one ofsomatostatin’s many physiologic actions, and scattered reports of efficacy in dogs exist in the veterinary literature.9One study of 10 dogs with insulinomademonstrated an increase in plasma glucose anddecrease in plasma insulin after SC administrationof octreotide, with successful binding of the caninesomatostatin receptor.10 However, in a controlledstudy of 3 dogs that received octreotide and aplacebo (physiologic saline), no significant differencein insulin or glucose concentrations was noted.9 Onedog in the group did experience an improved bloodglucose compared with placebo at 8 hours afteradministration of octreotide, suggesting that somepatients may have a clinical benefit.9Management of Metastatic DiseaseStreptozotocinThe veterinary oncology literature has reported onstreptozotocin as the adjuvant therapy for recurrent or metastatic insulinoma. Streptozotocin is analkylating agent that is structurally similar to glucoseand is selectively taken up by the GLUT2 transporter. This transporter is found in high levels onpancreatic beta cells, causing cytotoxicity.While streptozotocin has not provided astatistically significant longer survival in caninepatients, objective responses have been documented;in 2 patients with paraneoplastic peripheralneuropathy, neurologic signs resolved with thistreatment.11ELIZA REISS GRANTEliza Reiss Grant, DVM, is amedical oncology resident at TuftsCummings School of VeterinaryMedicine. She received herveterinary degree from TuftsUniversity and completed aninternship at Angell AnimalMedicine Center. Her interestsinclude canine lymphoma andtumor genomics.Peer ReviewedStreptozotocin can be given to dogs at a dosageof 500 mg/m2 every 2 to 3 weeks. Due to anelevated risk for renal tubular necrosis, salinediureses for 7 hours (3 hours before administeringthe drug and 2 hours after discontinuation of thedrug) is recommended.Other adverse effects of streptozotocin reported inthe veterinary literature include vomiting, reversibleelevations in alanine aminotransferase (withdiscontinuation of the drug), and diabetes mellitus.In a recent study of biweekly streptozotocin, 6 of 19dogs developed diabetes mellitus, resulting in deathor euthanasia.12Tyrosine Kinase InhibitorsRecently, there has been interest in evaluating theefficacy of tyrosine kinase inhibitors, such as toceranib phosphate (Palladia, pfizer.com), for dogswith insulinoma. This interest is based on studiesevaluating sunitinib, a human multitargeted tyrosine kinase inhibitor, which has proven efficacy inphase II trials of humans with pancreatic neuroendocrine tumors.13,14 Anecdotally, we have experienced antitumor activity with toceranib phosphatein dogs with insulinomas in the measurable diseasesetting.Toceranib phosphate is well tolerated at a doseof 2.75 mg/kg PO Q 48 H. The most commonadverse effects are gastrointestinal (diarrhea,decreased appetite, nausea), with myelosuppressionand proteinuria15 being less common but welldocumented adverse effects.IN SUMMARYInsulinoma is an uncommon malignant neoplasiain dogs that can result in significant illness, seizures,and death. Patients often present with clinical signs attributable to hypoglycemia. Diagnostics should include baseline bloodworkand imaging tests to rule out other causes ofhypoglycemia.KRISTINE E. BURGESSKristine E. Burgess, DVM, Diplomate ACVIM(Oncology), is an assistant professor in oncologyat Tufts University Cummings School ofVeterinary Medicine. She received her veterinarydegree from Tufts University, and completedan internship at VCA West Los Angeles AnimalHospital and residency in oncology at Universityof Wisconsin—Madison. Dr. Burgess’ interestsinclude comparative oncology with a specialinterest in canine lymphoma.tvpjournal.com November/December 2016 An Official Journal of the NAVC TODAY’S VETERINARY PRACTICE63
PRACTICAL ONCOLOGY Thoracic radiography and abdominal ultrasound are recommended but arefrequently unrewarding. Dual-phase CT angiography may be the best imaging study to diagnose insulinoma. Surgery is recommended and provides the best reported survival times. Medical management with dietary change, prednisone, diazoxide, and octreotideis possible. Streptozotocin is a reasonable adjuvant chemotherapy for patients with metastatic or recurrent insulinoma but is nephrotoxic, causes diabetes mellitus insome patients, and should be used with caution. Toceranib phosphate has not been formally studied in dogs with insulinoma but,on the basis of data in human studies, it may be an effective and well-toleratedtreatment option.AIGR amended insulin-to-glucose ratio; CT computed 14.15.16.64Goutal CM, Brugmann BL, Ryan KA. Insulinoma in dogs: A review. JAAHA 2012; 48:151-163.Polton GA, White RN, Brearley MJ, Eastwood JM. Improved survival in a retrospective cohort of28 dogs with insulinoma. J Sm Anim Prac 2007; 48(3):151-156.Trifonidou MA, Kirpensteijn J, Robben JH. A retrospective evaluation of 51 dogs with insulinoma.Vet Q 1998; 20(1):S114-S115.Elie MS, Zerbe CA. Insulinoma in dogs, cats and ferrets. Comp Cont Edu Pract Vet 1995; 17(1):5159.Robben JH, Pollak YW, Kirpensteijn J, et al. Comparison of ultrasonography, computedtomography, and single-photon emission computed tomography for the detection and localizationof canine insulinoma. J Vet Intern Med 2005; 19:15-22.Mai W, Caceres AV. Dual-phase computed tomographic angiography in three dogs with pancreaticinsulinoma. Vet Rad US 2008; 49(2):141-148.Tobin RL, Nelson RW, Lucroy MD, et al. Outcome of surgical versus medical treatment of dogswith beta cell neoplasia: 39 cases (1990-1997). JAVMA 1999; 215(2):226-230.Fischer JR, Smith SA, Harkin KR. Glucagon constant-rate infusion: A novel strategy for themanagement of hyperinsulinemic-hypoglycemic crisis in the dog. JAAHA 2000; 36(1):27-32.Simpson KW, Stepien RL, Elwood CM, et al. Evaluation of the long-acting somatostatin analogueocretotide in the management of insulinoma in three dogs. J Sm Anim Prac 1995; 36:161-165.Robben JH, Visser-Wisselaar HA, Rutterman GR, et al. In vitro and in vivo detection of functionalsomatostatin receptors in canine insulinomas. J Nuc Med 1997; 38(7):1036-1042.Moore AS, Nelson RW, Henry CJ, et al. Streptozocin for treatment of pancreatic islet cell tumors indogs: 17 cases (1989-1999). JAVMA 2002; 221(6):811-818.Northrup NC, Rassnick KM, Gieger TL, et al. Prospective evaluation of biweekly streptozotocin in19 dogs with insulinoma. J Vet Intern Med 2013; 27(3):483-490.Fjallskog MLH, Lejonklou MH, Oberg KE, et al. Expression of molecular targets for tyrosinekinase receptor antagonists in malignant endocrine pancreatic tumors. Clin Canc Res 2003; 9:14691473.Papaetis GS, Syrigos KN. Sunitinib: A multitargeted receptor tyrosine kinase inhibitor in the era ofmolecular cancer therapies. BioDrugs 2009; 23(6):377-389.Tjostheim SS, Stepien RL, Markovic LE, et al. Effects of toceranib phosphate on systolic bloodpressure and proteinuria in dogs. J Vet Intern Med 2016 [epub ahead of print].Dunn JK, Bostock DE, Herrtage ME, et al. Insulin-secreting tumours of the canine pancreas:Clinical and pathological features of 11 cases. J Sm Anim Prac 1993; 34:325-331.November/December 2016 tvpjournal.com
A positive insulin-to-glucose ratio demonstrates an inappropriately elevated insulin level in the setting of hypoglycemia.1 Nevertheless, an elevated AIGR is neither sensi-tive nor specific for the diagnosis of insulinoma. The AIGR can be elevated from insulin-produc-ing tumors other than insulinoma or normal in dogs with insulinoma.