Transcription
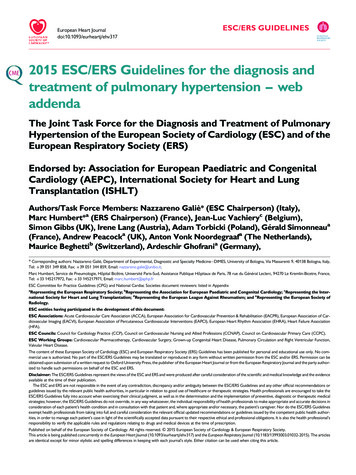
European Heart Journaldoi:10.1093/eurheartj/ehv317ESC/ERS GUIDELINES2015 ESC/ERS Guidelines for the diagnosis andtreatment of pulmonary hypertension – webaddendaThe Joint Task Force for the Diagnosis and Treatment of PulmonaryHypertension of the European Society of Cardiology (ESC) and of theEuropean Respiratory Society (ERS)Endorsed by: Association for European Paediatric and CongenitalCardiology (AEPC), International Society for Heart and LungTransplantation (ISHLT)Authors/Task Force Members: Nazzareno Galiè* (ESC Chairperson) (Italy),Marc Humbert*a (ERS Chairperson) (France), Jean-Luc Vachieryc (Belgium),Simon Gibbs (UK), Irene Lang (Austria), Adam Torbicki (Poland), Gérald Simonneaua(France), Andrew Peacocka (UK), Anton Vonk Noordegraafa (The Netherlands),Maurice Beghettib (Switzerland), Ardeschir Ghofrania (Germany),* Corresponding authors: Nazzareno Galiè, Department of Experimental, Diagnostic and Specialty Medicine –DIMES, University of Bologna, Via Massarenti 9, 40138 Bologna, Italy,Tel: 39 051 349 858, Fax: 39 051 344 859, Email: nazzareno.galie@unibo.it.Marc Humbert, Service de Pneumologie, Hôpital Bicêtre, Université Paris-Sud, Assistance Publique Hôpitaux de Paris, 78 rue du Général Leclerc, 94270 Le Kremlin-Bicetre, France,Tel: 33 145217972, Fax: 33 145217971, Email: marc.humbert@aphp.frESC Committee for Practice Guidelines (CPG) and National Cardiac Societies document reviewers: listed in AppendixaRepresenting the European Respiratory Society; bRepresenting the Association for European Paediatric and Congenital Cardiology; cRepresenting the International Society for Heart and Lung Transplantation; dRepresenting the European League Against Rheumatism; and eRepresenting the European Society ofRadiology.ESC entities having participated in the development of this document:ESC Associations: Acute Cardiovascular Care Association (ACCA), European Association for Cardiovascular Prevention & Rehabilitation (EACPR), European Association of Cardiovascular Imaging (EACVI), European Association of Percutaneous Cardiovascular Interventions (EAPCI), European Heart Rhythm Association (EHRA), Heart Failure Association(HFA).ESC Councils: Council for Cardiology Practice (CCP), Council on Cardiovascular Nursing and Allied Professions (CCNAP), Council on Cardiovascular Primary Care (CCPC).ESC Working Groups: Cardiovascular Pharmacotherapy, Cardiovascular Surgery, Grown-up Congenital Heart Disease, Pulmonary Circulation and Right Ventricular Function,Valvular Heart Disease.The content of these European Society of Cardiology (ESC) and European Respiratory Society (ERS) Guidelines has been published for personal and educational use only. No commercial use is authorized. No part of the ESC/ERS Guidelines may be translated or reproduced in any form without written permission from the ESC and/or ERS. Permission can beobtained upon submission of a written request to Oxford University Press, the publisher of the European Heart Journal or from the European Respiratory Journal and the party authorized to handle such permissions on behalf of the ESC and ERS.Disclaimer: The ESC/ERS Guidelines represent the views of the ESC and ERS and were produced after careful consideration of the scientific and medical knowledge and the evidenceavailable at the time of their publication.The ESC and ERS are not responsible in the event of any contradiction, discrepancy and/or ambiguity between the ESC/ERS Guidelines and any other official recommendations orguidelines issued by the relevant public health authorities, in particular in relation to good use of healthcare or therapeutic strategies. Health professionals are encouraged to take theESC/ERS Guidelines fully into account when exercising their clinical judgment, as well as in the determination and the implementation of preventive, diagnostic or therapeutic medicalstrategies; however, the ESC/ERS Guidelines do not override, in any way whatsoever, the individual responsibility of health professionals to make appropriate and accurate decisions inconsideration of each patient’s health condition and in consultation with that patient and, where appropriate and/or necessary, the patient’s caregiver. Nor do the ESC/ERS Guidelinesexempt health professionals from taking into full and careful consideration the relevant official updated recommendations or guidelines issued by the competent public health authorities, in order to manage each patient’s case in light of the scientifically accepted data pursuant to their respective ethical and professional obligations. It is also the health professional’sresponsibility to verify the applicable rules and regulations relating to drugs and medical devices at the time of prescription.Published on behalf of the European Society of Cardiology. All rights reserved. & 2015 European Society of Cardiology & European Respiratory Society.This article is being published concurrently in the European Heart Journal (10.1093/eurheartj/ehv317) and the European Respiratory Journal (10.1183/13993003.01032-2015). The articlesare identical except for minor stylistic and spelling differences in keeping with each journal’s style. Either citation can be used when citing this article.
Page 2 of 13ESC/ERS GuidelinesMiguel Angel Gomez Sanchez (Spain), Georg Hansmannb (Germany),Walter Klepetkoc (Austria), Patrizio Lancellotti (Belgium), Marco Matuccid (Italy),Theresa McDonagh (UK), Luc A. Pierard (Belgium), Pedro T. Trindade (Switzerland),Maurizio Zompatorie (Italy), and Marius Hoepera (Germany)Document Reviewers: Victor Aboyans (CPG Review Coordinator) (France), Antonio Vaz Carneiro (CPG ReviewCoordinator) (Portugal), Stephan Achenbach (Germany), Stefan Agewall (Norway), Yannick Allanored (France),Riccardo Asteggiano (Italy), Luigi Paolo Badano (Italy), Joan Albert Barberàa (Spain), Hélène Bouvaist (France),Héctor Bueno (Spain), Robert A. Byrne (Germany), Scipione Carerj (Italy), Graça Castro (Portugal), Çetin Erol(Turkey), Volkmar Falk (Germany), Christian Funck-Brentano (France), Matthias Gorenflob (Germany),John Grantonc (Canada), Bernard Iung (France), David G. Kiely (UK), Paulus Kirchhof (Germany/UK),Barbro Kjellstrom (Sweden), Ulf Landmesser (Switzerland), John Lekakis (Greece), Christos Lionis (Greece),Gregory Y. H. Lip (UK), Stylianos E. Orfanosa (Greece), Myung H. Parkc (USA), Massimo F. Piepoli (Italy),Piotr Ponikowski (Poland), Marie-Pierre Revele (France), David Rigaua (ERS methodologist) (Switzerland),Stephan Rosenkranz (Germany), Heinz Völler (Germany), and Jose Luis Zamorano (Spain)The disclosure forms of all experts involved in the development of these guidelines are available on the ESC websitehttp://www.escardio.org/guidelines- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - KeywordsGuidelines † Pulmonary hypertension † Pulmonary arterial hypertension † Chronic thromboembolicpulmonary hypertension † Congenital heart disease † Connective tissue disease † Heart failure † Respiratoryfailure † Endothelin receptor antagonists † Phosphodiesterase type 5 inhibitors † Prostacyclin analogues †Lung disease † Left heart diseaseList of Web TablesWeb addenda . . . . . . . . . . . . . . . . . . . . . . . . . . .Pathology of pulmonary hypertension . . . . . . . . . . .Pathobiology of pulmonary hypertension . . . . . . . . .Pulmonary arterial hypertension screening programmeQuality of life measurements . . . . . . . . . . . . . . . . .References . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2235811††Web addendaPathology of pulmonary hypertension†Different pathological features characterise the diverse clinical pulmonary hypertension (PH) groups.51,52† Group 1, pulmonary arterial hypertension (PAH): pathologicalchanges predominantly affect the distal pulmonary arteries(,500 mm) with medial hypertrophy, intimal proliferative andfibrotic changes, adventitial thickening with mild to moderateperivascular inflammatory infiltrates and lymphoid neogenesis,complex lesions (plexiform, dilated lesions) and thromboticlesions. Pulmonary veins are classically unaffected.† Group 1′ : includes mainly pulmonary veno-occlusive disease(PVOD) involving septal veins and pre-septal venules with occlusive fibrotic lesions, venous muscularization, patchy capillary proliferation with pulmonary capillary haemangiomatosis (PCH),pulmonary oedema, occult alveolar haemorrhage, lymphatic†dilatation, lymph node enlargement (vascular transformation ofthe sinus) and inflammatory infiltrates. Distal pulmonary arteriesare affected by medial hypertrophy and intimal fibrosis.Group 1′′ : persistent pulmonary hypertension of the newborn(PPHN) is characterized by changes in vasoreactivity and wallstructure and decreases in pulmonary vascular density with reduced alveolarisation.Group 2: PH due to left heart disease (LHD) is characterised byenlarged and thickened pulmonary veins, pulmonary capillarydilatation, interstitial oedema, alveolar haemorrhage and lymphatic vessel and lymph node enlargement. Distal PA may beaffected by medial hypertrophy and intimal fibrosis.Group 3: PH due to lung diseases and/or hypoxaemia is characterized by medial hypertrophy, intimal obstructive proliferationof the distal pulmonary artery (PA) and muscularisation of arterioles. A variable degree of destruction of the vascular bed in emphysematous or fibrotic areas may also be present.Group 4: PH due to chronic PA obstruction: chronic thromboembolic pulmonary hypertension (CTEPH) lesions include organized thrombi tightly attached to the medial layer in theelastic PA, replacing the normal intima. These may occludethe lumen or form different grades of stenosis, webs andbands.53 A pulmonary microvascular disease can develop inthe non-occluded and occluded areas that has similarities withPAH (with the exception of uncommon plexiform lesions inCTEPH) and patchy post-capillary remodelling related tobronchial-to-pulmonary venous shunting.54,55 Collateral vesselsfrom the systemic circulation (from bronchial, costal,
Page 3 of 13ESC/ERS GuidelinesWeb Table I Condensed clinical classification ofpulmonary hypertension (updated from Simonneauet al.1)Web Table II Anatomical-pathophysiologicalclassification of congenital systemic-to-pulmonaryshunts associated with pulmonary arterial hypertension(adapted from Simmoneau et al.2)1. Pulmonary arterial hypertension (PAH)1. Type1.1 Idiopathic1.2 Heritable1.2.1 BMPR2 mutation1.2.2 Other mutations1.3 Drugs and toxins induced1.4 Associated with:1.4.1 Connective tissue disease1.4.2 HIV infection1.4.3 Portal hypertension1.4.4 Congenital heart disease (Table 6)1.4.5 Schistosomiasis1.1 Simple pre-tricuspid shunts1.1.1 Atrial septal defect (ASD)1.1.1.1 Ostium secundum1.1.1.2 Sinus venosus1.1.1.3 Ostium primum1.1.2 Total or partial unobstructed anomalous pulmonary venousreturn1.2 Simple post-tricuspid shunts1.2.1 Ventricular septal defect (VSD)1.2.2 Patent ductus arteriosus1.3 Combined shuntsedominant defect1.4 Complex congenital heart disease1.4.1 Complete atrioventricular septal defect1.4.2 Truncus arteriosus1.4.3 Single ventricle physiology with unobstructed pulmonaryw1.4.4 Transposition of the great arteries with VSD (withoutpulmonary stenosis) and/or patent ductus arteriosus1.4.5 Other1’. Pulmonary veno-occlusive disease and/or pulmonarycapillary haemangiomatosis1”. Persistent pulmonary hypertension of the newborn2. Pulmonary hypertension due to left heart disease2.1 Left ventricular systolic dysfunction2.2 Left ventricular diastolic dysfunction2.3 Valvular diseaseobstruction and congenital cardiomyopathies2.5 Other2. Dimension (specify for each defect if more than onecongenital heart defect exists)3. Pulmonary hypertension due to lung diseases and/orhypoxia2.1 Haemodynamic (specify Qp/Qs) a2.1.1 Restrictive (pressure gradient across the defect)2.1.2 Non-restrictive2.2 Anatomicb2.2.1 Small to moderate (ASD 2.0 cm and VSD 1.0 cm)2.2.2 Large (ASD 2.0 cm and VSD 1.0 cm)3.1 Chronic obstructive pulmonary disease3.2 Interstitial lung disease3.3 Other pulmonary diseases with mixed restrictive andobstructive pattern3.4 Sleep-disordered breathing3.5 Alveolar hypoventilation disorders3.6 Chronic exposure to high altitude3.7 Developmental lung diseases (Web Table III)3. Direction of shunt3.1 Predominantly systemic-to-pulmonary3.2 Predominantly pulmonary-to-systemic3.3 Bidirectional4. Chronic thromboembolic pulmonary hypertensionand other pulmonary artery obstructions4. Associated cardiac and extracardiac abnormalities4.1 Chronic thromboembolic pulmonary hypertension4.2 Other pulmonary artery obstructions5. Repair status5.1 Unoperated5.2 Palliated (specify type of operation/s, age at surgery)5.3 Repaired (specify type of operation/s, age at surgery)5. Pulmonary hypertension with unclear and/ormultifactorial mechanisms5.1 Haematological disorders5.2 Systemic disorders5.3 Metabolic disorders5.4 Othersdiaphragmatic and coronary arteries) can grow to reperfuseareas distal to complete obstructions.† Group 5: PH with unclear and/or multifactorial mechanismsincludes heterogeneous conditions with different pathologicalpictures.Pathobiology of pulmonary hypertensionDifferent pathobiological features56 – 58 characterise the diverseclinical PH groups.† Group 1: PAH has a multifactorial pathobiology. Excessive vasoconstriction has been related to abnormal function or expressionaRatio of pulmonary (Qp) to systemic (Qs) blood flow.The size applies to adult patients.bof potassium channels in the smooth muscle cells and to endothelial dysfunction leading to chronically impaired productionof vasodilator and antiproliferative agents such as nitric oxide(NO) and prostacyclin, along with overexpression of vasoconstrictor and proliferative substances such as thromboxane A2and endothelin-1. Many of these abnormalities both elevate vascular tone and promote vascular remodelling by proliferativechanges involving endothelial and smooth muscle cells as wellas fibroblasts and pericytes. Growth factors such as plateletderived growth factor, fibroblast growth factor, transforminggrowth factor b (TGFb) and bone morphogenic proteins play arole in the remodelling process. Reduced bone morphogenetic
Page 4 of 13ESC/ERS Guidelines† Group 1′′ : In PPHN, endothelial cell dysfunction (with decreasedNO production and activity) and impaired angiogenic mechanisms underlie abnormalities of lung vascular growth.† Group 2: PH due to LHD: The mechanisms responsible for theincrease in pulmonary arterial pressure (PAP) include passivebackward transmission of the pressure elevation (isolated postcapillary PH, Table 3). In these cases pulmonary vascular resistance (PVR) is within the normal range. In other circumstancesthe elevation of PAP is greater than that of the pulmonary arterywedge pressure (PAWP), leading to an increase in PVR (combined post-capillary and pre-capillary PH, Table 3). The elevationof PVR is due to an increase in PA vasomotor tone and/or to fixedstructural obstructive remodelling of the PA resistance vessels;59the former component of reactive PH is reversible under acutepharmacological testing, while the latter, characterized by medialhypertrophy and intimal proliferation of the pulmonary arteriole,does not respond to the acute challenge.60† Group 3: PH due to lung diseases and/or hypoxia: The mechanisms involved include hypoxic vasoconstriction, mechanical stressof hyperinflated lungs, loss of capillaries, inflammation and toxiceffects of cigarette smoke. There are also data supporting anendothelium-derived vasoconstrictor– vasodilator imbalance.† Group 4: PH due to chronic PA obstruction: Non-resolutionof acute embolic masses that later undergo fibrosis leading tomechanical obstruction of pulmonary arteries is believed to bean important pathobiological process in CTEPH. However, amechanistic view of CTEPH as a disease exclusively caused by obliteration of central pulmonary arteries by pulmonary emboli istoo simplistic. Pulmonary embolism (PE) could be followed bya pulmonary vascular remodelling process modified by infection,immune phenomena, inflammation and circulating and vascularresident progenitor cells. Only a few specific thrombophilic factors, such as antiphospholipid antibodies, lupus anticoagulant andelevated factor VIII, have been statistically associated withCTEPH, and no abnormalities of fibrinolysis have beenprotein receptor 2 (BMPR2) expression contributes to thepathobiology of heritable and other forms of PAH. Other celltypes (inflammatory cells and platelets) and mediators (cytokines,chemokines, serotonin, etc.) play a role in PAH. Prothromboticabnormalities have been demonstrated in PAH patients andthrombi are present in both the small distal pulmonary arteriesand in proximal elastic pulmonary arteries. Autoimmunity is present in subgroups of PAH patients, as suggested by circulatingautoantibody recognizing pulmonary vascular cells and detectionof lymphoid neogenesis in the lungs of idiopathic PAH (IPAH)patients.† Group 1′ : In PVOD, bi-allelic EIF2AK4 mutations, inflammationand exposure to toxic agents induce oxidative and inflammatoryinjuries.Web Table III Developmental lung disease associatedwith pulmonary hypertension (adapted from Ivy et al.3)1. Congenital diaphragmatic hernia2. Bronchopulmonary dysplasia3. Alveolar capillary dysplasia (ACD)4. ACD with misalignment of veins5. Lung hypoplasia (“primary” or “secondary”)6. Surfactant protein abnormalitiesa. Surfactant prb. Surfactant prc. ATP-binding cassette A3 mutationd. Thyroid transcription factor 1/Nkx2.1 homeobox mutation7. Pulmonary interstitial glycogenosis8. Pulmonary alveolar proteinosis9. Pulmonary lymphangiectasiaWeb Table IV Route of administration, half-life, dose ranges, increments, and duration of administration of the mostcommonly used agents for pulmonary vasoreactivity testsDrugRouteHalf-lifeDose rangedIncrementseDurationfClass aLevelbRef cNitric oxideInh15–30 sec10–20 ppm-5 mingIC4, 5Epoprostenoli.v.3 min2–12 ng/kg/min2 ng/kg/min10 minIC4, 6Adenosinei.v.5–10 sec50–350 µg/kg/min50 µg/kg/min2 minIIaC7IloprostInh30 min5–20 µg-15 minIIbC8Inh ¼ inhaled; i.v. ¼ intravenous; NO ¼ nitric oxide; ppm ¼ parts per million.aClass of recommendation.bLevel of evidence.cReference(s) supporting recommendations.dInitial dose and maximal dose suggested.eIncrements of dose by each step.fDuration of administration on each step.gFor NO a single step within the dose range is suggested.
ESC/ERS GuidelinesWeb Table V Functional classification of pulmonaryhypertension modified after the NYHA functionalclassification according to the WHO 1998.9Class I – Patients with pulmonary hypertension but without resultinglimitation of physical activity. Ordinary physical activity does not causeundue dyspnoea or fatigue, chest pain or near syncope.Class II – Patients with pulmonary hypertension resulting in slightlimitation of physical activity. They are comfortable at rest. Ordinaryphysical activity causes undue dyspnoea or fatigue, chest pain or nearsyncope.Class III – Patients with pulmonary hypertension resulting in markedlimitation of physical activity. They are comfortable at rest. Less thanordinary activity causes undue dyspnoea or fatigue, chest pain or nearsyncope.Class IV – Patients with pulmonary hypertension with inability tocarry out any physical activity without symptoms. These patientsmanifest signs of right heart failure. Dyspnoea and/or fatigue may evenbe present at rest. Discomfort is increased by any physical activity.NYHA ¼ New York Heart Association; WHO ¼ World Health Organization.consistently demonstrated. Microvascular disease may be relatedto shear stress in non-obstructed areas, post-capillary remodelling related to bronchial-to-pulmonary venous shunting, pressure, inflammation and release of cytokines and vasculotrophicmediators.55† Group 5: By definition, the pathobiology in this group is unclearor multifactorial.Pulmonary arterial hypertensionscreening programmeThe prognosis of PAH is significantly worse in patients with advanced disease.61,62 PAH therapies delay clinical worsening63 anddata are accumulating suggesting that early treatment improveslong-term outcome.13,63,64 Screening is the systematic applicationof a test to identify individuals at sufficient risk of a specific disorderto warrant further investigation or direct preventive action amongpersons who have not sought medical attention on account ofsymptoms of that disorder.65 Therefore screening for PH/PAH applies to asymptomatic individuals belonging to groups in which PH/PAH is highly prevalent, such as patients with systemic sclerosis(SSc),66,67 BMPR2 mutation carriers or relatives of patients with heritable PAH (HPAH),68 patients with sickle cell disease (SCD) and patients with portal hypertension referred for liver transplantation.69A screening method should use tools that are non-invasive, reproducible, associated with a high negative predictive value for thecondition and cost effective.61 In PH/PAH, these tools include pulmonary function tests (PFTs), circulating biomarkers and echocardiography. In SSc, PFTs have long been used as a screening tool,especially changes in diffusing capacity of the lung for carbon monoxide (DLCO).70,71 An increased risk of PAH has been shown inadult SSc patients with a DLCO ,60% of predicted.67 There isnow additional evidence suggesting that biomarkers [N-terminalpro-brain natriuretic peptide (NT-proBNP)], alone72,73 or inPage 5 of 13combination with PFTs,74 may identify patients at higher risk to present SSc-PAH. Finally, a recent study in patients undergoing rightheart catheterization (RHC) as part of the evaluation of SSc suggested that, in the absence of PH, an increase in the transpulmonarypressure gradient (TPG) was associated with a higher risk of subsequently developing pre-capillary PH.75 Echocardiography at rest remains the best way to estimate elevated pulmonary pressures. It hasbeen used in large SSc-PAH screening programmes67,76 by stratifying patients according to the level of PAPs estimated by the tricuspidregurgitant velocity (TRV). The recommendations for diagnosticmanagement according to echocardiographic probability of PH inasymptomatic patients with or without risk factors for PAH orCTEPH are reported in Online Table IX. Conversely, exercise echocardiography has technical and methodological limitations and is notrecommended for PH/PAH screening.77 – 81Recent studies in SSc and SCD have demonstrated that asymptomatic PAH patients detected by screening can be missed by Doppler echocardiography (false negative), emphasizing the need for amultitest approach. In SSc, a composite measure has been proposedin the DETECT study.67 In this study, adult SSc patients with.3-years disease duration and a DLCO ,60% of predicted underwent non-invasive testing and RHC. A stepwise detection approachhas been proposed with six simple clinical and biological assessments in step 1 of the algorithm determining referral to echocardiography. In step 2, the step 1 prediction score and twoechocardiographic variables determined referral to RHC. The DETECT algorithm recommended RHC in 62% of patients (referralrate) and missed 4% of PAH patients (false negatives). Of those,19% had RHC-confirmed PAH.67 This screening approach is interesting, but there is currently no information on long-term outcomesin asymptomatic SSc-PAH patients screened thanks to the DETECTalgorithm. Of note, the DETECT study did not provide recommendations regarding patients with a DLCO 60% and its findings needto be validated in another cohort. Beyond initial screening, the frequency of non-invasive tests is unclear in asymptomatic subjectswith a high risk of developing incident PAH. Annual screeningwith echocardiography, DLCO and NT-proBNP has been proposedin SSc patients.66,82Pre-capillary PH is a known complication of SCD, but the prevalence SCD-PH has been overestimated in echocardiography basedstudies.83 Two recent studies84,85 employed similar methodologiesand referred all patients with a screening TRV 2.5 m/s on echocardiography for confirmatory RHC. The prevalence of PH rangedfrom 6.2 to 10% (post-capillary PH in 3.3 and 6.2%, and pre-capillaryPH in 2.9 and 3.8%, respectively). An exploratory post-hoc analysisfound that calibrating TRV to 2.9 m/s or TRV between 2.5 and2.8 m/s plus either NT-proBNP .164.5 pg/ml or a 6-minute walkdistance (6MWD) ,333 m reduced the number of RHC referralscompared with a single TRV threshold 2.5 m/s.84BMPR2 mutation carriers have a lifetime risk of developing PAH ofapproximately 20%.68,86 It is currently not possible to predict thosewho will ultimately develop PAH, although women are at increasedrisk compared with men.86 In patients carrying a BMPR2 mutation,the frequency of screening is unknown. At present, asymptomaticindividuals who test positive for PAH-causing mutations and firstdegree relatives of HPAH patients in whom no causal mutationshave been identified are offered yearly screening echocardiography.
Page 6 of 13ESC/ERS GuidelinesWeb Table VIA Characteristics of randomised controlled trials with pulmonary arterial hypertension drugs interferingwith the endothelin pathway (Endothelin receptors antagonists)Drug(s)testedStudyNumber ndpointMain ResultsARIES-11020212No6MWD6MWD improvedTTCW not improvedARIES-21019212No6MWD6MWD improvedTTCW improvedStudy-351113212No6MWD6MWD improvedTTCW improvedBREATHE-11221316No6MWD6MWD improvedTTCW improvedEARLY1318524No, orPVR,6MWDPVR improvedTTCW improved6MWD not improvedBREATHE-5145412SaO2,PVRPVR improved6MWD improvedCOMPASS-21533499TTCWTTCW not improved6MWD improvedNT-proBNP improvedSERAPHIN16742115TTCWTTCW improved inmonotherapy andcombinationAmbrisentanBosentanNoNo, orMacitentanInh iloprost6MWD ¼ 6-minute walking distance; PVR ¼ pulmonary vascular resistance; SaO2 ¼ finger oxygen saturation; TTCW ¼ time to clinical worsening.Web Table VIB Characteristics of randomised controlled trials with pulmonary arterial hypertension drugs interferingwith the nitric oxide pathway (Soluble guanylate cyclase stimulators, Phosphodiesterase type-5 inhibitors)Drug(s)testedStudyNumber ndpointMain resultsPATENT1744312No, orbosentan, or prostanoids6MWD6MWD improvedHaemodynamics improvedPATENT plus183018Supine SBPTerminated for excess of SAEin the treated groupSUPER-11927712No6MWD6MWD improvedTTCW not improvedSastry202212NoTTTT improved21Singh206No6MWD6MWD improvedPACES2226416Epoprostenol6MWD6MWD improvedTTCW andhaemodynamics improvedIversen232012Bosentan6MWD6MWD not improved10312Bosentan6MWD6MWD not improvedPHIRST2440516No, orbosentan (54%)6MWD6MWD improved(In bosentan treated patients 23 m, 95% CI -2 to 48 m)TTCW improvedEVALUATION256612No6MWD6MWD improvedTTCW improvedRiociguatA1481243a6MWD ¼ 6-minute walking distance; SAE ¼ serious adverse events; TTCW ¼ time to clinical worsening; TT ¼ treadmill test.aThis drug is not approved by the EMA at the time of publication of these guidelines.
Page 7 of 13ESC/ERS GuidelinesWeb Table VIC Characteristics of randomised controlled trials with pulmonary arterial hypertension drugs interferingwith the prostacyclin pathway (Prostacyclin analogues and prostacyclin receptors agonists)Drug(s)testedStudyNumber ndpointALPHABET2613012No6MWD6MWD improvedHaemodynamics not improvedBarst2711652NoCWCW not improvedRubin282312No6MWD6MWD improvedHaemodynamics improvedBarst298112No6MWD6MWD improvedHaemodynamics improvedSurvival improvedBadesch3011112No6MWD6MWD improvedBeraprostaEpoprostenolInhaled IloprostMain resultsAIR3120312No6MWD & FC6MWD & WHO-FC improvedHaemodynamics improvedat peakSTEP326712Bosentan6MWD6MWD improved (P 0.051)TTCW improvedCOMBI334012Bosentan6MWDTerminated for futility6MWD not improvedNo clinical improvementSC – Pivotalstudy3447012No6MWD6MWD improvedHaemodynamics improvedPain at infusion siteInhala TRIUMPH35235126MWD6MWD improvement ( 20 mat peak, 12 m at trough)TTCW not improvedPOa- Freedom M3618516No6MWD6MWD improvement ( 26 mat peak, 17 m at trough)TTCW not improvedPOa- Freedom C13735416ERA and/or PDE-5i6MWD6MWD not improvedTTCW not improvedPOa- Freedom C23831016ERA and/or PDE-5i6MWD6MWD not improvedTTCW not improvedPhase - 2394317ERA and/or PDE-5iPVRPVR improved6MWD not improvedGRIPHON40115674ERA and/or PDE-5iTTCWTTCW improvedBosentanTreprostinilSelexipaga6MWD ¼ six minute walking distance; CW ¼ clinical worsening; PVR ¼ pulmonary vascular resistance; TT ¼ treadmill test; TTCW ¼ time to clinical worsening.aThis drug is not approved by the EMA at the time of publication of these guidelines.Web Table VID Characteristics of randomised controlled trials with pulmonary arterial hypertension drugs testinginitial combination therapyDrug(s)testedEpoprostenol vsepoprostenol bosentanStudyNumber ndpointMain resultsBREATHE-2413312NoPVRPVR not improved6MWD not improvedAMBITION4250078NoTTCFTTCF improved6MWD improvedAmbrisentanambrisentan 6MWD ¼ 6-minute walking distance; TTCF ¼ time to clinical failure; PVR ¼ pulmonary vascular resistance.
Page 8 of 13ESC/ERS GuidelinesWeb Table VII Potentially significant drug interactions with pulmonary arterial hypertension drugsaPAH drugAmbrisentanBosentanMechanism of interaction?Interacting drugCyclosporineKetoconazoleCYP3A4 inducerInteractionCaution is required in the co-administration of ambrisentan withketoconazole and cyclosporine.adjustments of either drug.CYP3A4 substrateCyclosporineCyclosporine levels fall 50%; bosentan levels increase 4-fold. Combinationcontraindicated.CYP3A4 substrateErythromycinBosentan levels increase. May not re
Web addenda Pathology of pulmonary hypertension Different pathological features characterise the diverse clinical pul-monary hypertension (PH) groups.51,52 † Group 1, pulmonary arterial hypertension (PAH): pathological changes predominantly affect the distal pulmonary arteries (,500 mm) with medial hypertrophy, intimal proliferative and