Transcription
CONGENITAL HEART DEFECTS 18AGING WITH HIV 25LIVING DONOR 32edicineFA L L 2 0 1 5“It felt personal,that the Ebola viruscould still bein my eye withoutmy knowing it.” — Dr. Ian Crozier
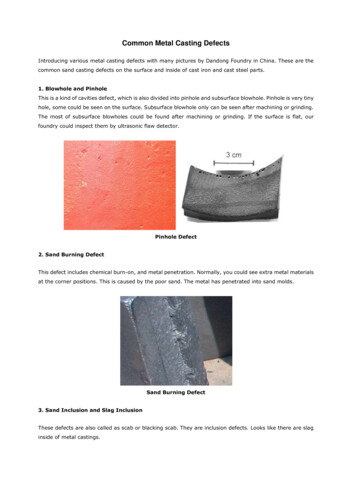
Continuity of CareIn past generations, when babies were born with hearts that didn’t form properly—with leaky or narrow valves, holes in the wall between the chambers, or muscleDownload our iPad app (search underabnormalities—parents were not offered much hope.Emory Health magazines.) Bonus features areEven if the child survived, it was expected thatthey would have an abbreviated, curtailed life.Today, for the first time, there are more adultsthan children living with congenital heart defects(CHDs). They are going to college, having childrenthemselves, and becoming scientists and researchers and musicians and teachers (see p. 18).That’s why medical homes like Emory’s AdultCongenital Heart Center—the only one in the stateand one of the largest in the country—are important. They provide a continuity of care vital forpatients with lifelong conditions like CHD.Emory’s center follows more than 3,000 CHDpatients,with about 2,000 patient visits and 100Christian Larsenheart surgeries yearly. Multidisciplinary teamsDean, Emory School of MedicinePresident, Emory Healthcareinclude adult and pediatric cardiologists, congenitalPhysicians Groupcardiac surgeons, electrophysiologists, interventional cardiologists, nurse practitioners, nurses,social workers, and echocardiographers. The center also provides genetic counselingand partners with our ob/gyn staff to provide high-risk pregnancy counseling andmanagement.“As these children grow into adults, they need ongoing specialty cardiac care,”says center director and cardiologist Wendy Book. “Yet this high-risk group oftenexperiences lapses in care because of the perception that they are ‘fixed’ or becausethey aren’t experiencing symptoms. CHDs are so closely associated with infancy andchildhood that people often think the conditions just don’t affect adults.”We are also helping to provide continuous care and support for adults withanother disease once thought to be a death sentence—HIV. Now, people who areHIV-positive are routinely living long enough to become senior citizens, grandparents, and retirees (see p. 25).At the Ponce de Leon Center, part of the Grady Health System, Emory doctorsand researchers, under the direction of Wendy Armstrong, serve more than 5,200people in the greater Atlanta area with HIV/AIDS. Many of the center’s patients volunteer to participate in research because they want to give back, Armstrong says.Patients have told her: “I was planning my death. I never expected to be able toplan my life.” A growing number of these patients are older than 50. The Atlanta VAMedical Center is also experiencing this “graying of an epidemic”—of its 1,600 HIVpositive patients, the median age is 52.The medical and research communities have done a great job of keeping patientswith these conditions alive. Now we need to keep them active and healthy so they canmake the most of their additional hard-won years.online at emorymedicinemagazine.emory.edu.Emory MedicineEditor Mary LoftusArt Director Peta WestmaasDirector of Photography Jack KearseGraphic Designer Linda DobsonProduction Manager Carol PintoWeb Specialist Wendy DarlingExec Dir, Health Sciences Creative Services Karon SchindlerAssociate VP, Health Sciences Communications Vincent DollardEditorial Intern Aspen Ono 18CEmory Medicine summer intern AspenOno, an Emory College sophomore, at anelephant sanctuary in Thailand.EDITORIAL ADVISORY BOARDChair Ray Dingledine, PhD, Professor and Chair of Pharmacology,Emory School of MedicineCharles Craig, Consultant and former President, Georgia BioA simple saliva test can help you plan for a healthy family.Robert Goddard III, Chair and CEO, Goddard InvestmentLucky Jain, MD, Professor of Pediatrics, EmoryClaire Perdue James, philanthropistMichael M.E. Johns, Exec VP for Health Affairs, EmoryJeff Koplan, MD, MPH, VP, Global Health, EmoryBased out of Emory University, the JScreen programoffers affordable, at-home genetic testing 24/7 across the U.S.Kimberly Manning MD, Associate Professor of Medicine, EmoryMargery McKay, VP, Health Sciences DevelopmentPaul Pendergrass, Independent Communications ConsultantJulie Ralston, Director of Communications, Atlanta RegionalCommissionWalker Ray, MD, Retired pediatrician, former presidentof the Emory Alumni AssociationBill Todd, Exec Director for Health Care Initiatives, College of Management, Georgia Institute of TechnologyPlease visit our website to request your kit today!Or purchase a gift card and give the gift they’llbe talking about for generations.info@jscreen.org 800.684.36082EMORY MEDICINEEmory Medicine is published three times a year forSchool of Medicine alumni, faculty, and staff, as well aspatients, donors, neighbors, and other friends of EmoryMedicine. Produced by the Woodruff Health Sciences CenterCommunications Office, the magazine is made possibleby support from the medical school dean and the Robert W.Woodruff Health Sciences Center Fund. Emory UniversityPlease send correspondence to Emory Medicine, 1762 CliftonRoad, Suite 1000, Atlanta, GA 30322; call 404-727-0161 oremail mary.loftus@emory.edu.Emory University is an equal opportunity/equal access/affirmativeaction employer fully committed to achieving a diverse workforceand complies with all federal and Georgia state laws, regulations, andexecutive orders regarding nondiscrimination and affirmative action.Emory University does not discriminate on the basis of race, age, color,religion, national origin or ancestry, sex, gender, disability, veteranstatus, genetic information, sexual orientation, or gender identity orexpression.
FALL 20151221FEATURESAND MOREHiding in Plain Sight 12Investing in Discovery 30Dr. Ian Crozier survived Ebola after30 Windows of Opportunityof Note40 days of intensive care in Emory’sSerious Communicable Diseases Unit.Months later, after very nearly taking hislife, Ebola tried to steal his sight.NEW AND NOTEWORTHY4 It’s not what you think.People are talking5 Adultswith autismpractice life skills 5 Sleep 101 5 EmoryPediatric Urban Health Program’s schoolbased clinics 6 Emory to lead EbolaThis cross section of a five-day-old mouse’s spinal cord highlights developingTraining Centerimages such as this, which won the Best Image contest at the Emory PostdoctoralStand up! 8 High-techheart help 8 Heart scan can predict premature death 8 You have the power toResearch Symposium, help researchers find out more about metabolic processes andfortsmolecular interactions, advancing knowledge that can save lives.HIV’s long tailinhibitory neurons, which control movement, in red and green. Vibrant microscopic7 prevent heart disease10 9 Secondary com-Easing phantom limb pain11 You Be the Doctor: TheCase of the Waxing Moon Face(Emory postdoctoral fellow JoAnna Anderson with Andre Rivard, Francisco Alvarez’s lab.)10 For the first time, there are more adultsthan children living with congenitalheart defects (CHDs), and they’re leading GiftsFrom the Executive VP 31Wright Caughman weighs in from theLast Word: The First Link 32Why a television medical reporter volunteered to be a kidney donor.By Beth Galvin (above with surgeon Nicole Turgeon).full, active lives. But this doesn’t meanthey’re cured.Down Syndrome andCongenital Heart Defects 21Aging with HIV 25About half of adults with HIV arenow 50 and older. They’re retiring, becoming grandparents, anddeveloping age-related diseases—things they never thought they’dlive long enough to experience.15-SOM-DEAN-009631Woodruff Health Sciences CenterBalancing Act 18On Our Radar 432“I sit here, alive first of all, and lookingthrough two eyes, which is absolutely remarkable for me personally, but there are10,000 to 15,000 Ebola survivorsin West Africa whoare grappling with these types ofailments as well.”12Visit us online at emorymedicinemagazine.emory.edu for bonus content. Send letters to the editor to mary.loftus@emory.edu.Spring 20153
ON OUR RADARLetters New and noteworthyPeople are talking.I am a quadrilateral amputee. In 2008, I contracted a Group A strep infection of theblood that caused toxic shock syndrome and necessitated the amputation of my hands belowthe elbow and my feet below the knee. Becoming independent has been my goal, just asAimee Copeland expressed in Emory Medicine magazine (Spring 2015). I first learned to feedmyself with body-powered prosthetics. I flipped many a forkful of food on the floor, but withpractice I have learned to eat at restaurants. I have learned to walk unaided and try to get inmy 10,000 steps each day (I’m a bit obsessed by the Fitbit). I love Aimee’s idea of planning anoutdoor area accessible to all. My husband and I have visitedseveral national parks and have found them surprisinglyaccessible. Like Aimee and her physical therapist, I also lovemy “torturer,” my personal trainer. I protest but I knowit’s good for me.Cheryl DouglassChevy Chase, Md.My husband, Donald Page, is a 1983 graduate of theSchool of Medicine and also did six years of post-gradFind the Spring 2015 issue onlineemorymedicinemagazine.emory.edutraining through Emory, which is why we receive your great publication: Emory Medicine.The article in your Spring 2015 issue about Aimee Copeland moved me. Aimee’s life taughtme so much about stepping up and choosing to be brave.Joan Walker Page“There is no sciencefiction anymore. Everything I read about as akid, we’re either doingit or we’re trying to doit. . Synthetic biology,for instance, actuallygenetically engineersanimals who createour drugs in theirblood or milk.”-Paul Root Wolpe,BEINGS Summit,May 17-19.http://bit.ly/beingswolpeMarietta, Ga.My husband, George Wallace, had to get two polyps removed after a colonoscopy, andthey later proved to be cancerous. Dr. Patrick Sullivan did TAMIS (transanal minimally invasivesurgery) on him. We both feel it saved his life. We spent one night at Emory Midtown, and thenursing staff and everyone else was just wonderful. The experience was with a culture I had notbeen exposed to in other hospitals with other doctors. I felt like Dr. Sullivan was treating uslike he would treat someone in his own family. My husband is an artist and gave him one of hispaintings in return. More people should be aware of this fairly new procedure, and that it cansave a lot of pain and recovery time.Sandy WallaceConyers, Ga.My wife was recently receiving four weeks of intense physical therapy for Parkinson’sat the Emory Rehab Hospital under the direction of Dr. Stewart Factor. I picked up a copy ofEmory Medicine and, as a former health care administrator, I found the articles very intellectually stimulating. Our son is enrolled in the Emory School of Nursing and is completing his MSNin the Family Practice NP Program. Emory has been a wonderful experience for my wife, ourson, and myself (I experienced a top-notch neurological workup there several years ago.)Bernie GaydosRoswell, Ga.We like to hear from you. Send us your comments, questions, suggestions, and castigations. Addresscorrespondence to Emory Medicine magazine, 1762 Clifton Road, Suite 1000, Atlanta, GA 30322;call 404-727-0161; or email mary.loftus@emory.edu.4EMORY MEDICINE“Our finding of similarity in clinical progression between humanpatients and Huntington’s disease monkeyssuggests monkeys couldbecome a preclinical,large animal modelfor the development ofnew treatments.Rightnow, we can address thesymptoms but we wantto do more.”-Anthony Chanhttp://bit.ly/huntingtonsmonkeysMyLife: Adults with autism practice life skills on campusDAMON MEHARGWorking out at the gym, swimming, riding the shuttles,where they can practice cooking healthy foods, cleaning,sharing a meal all are part of myLife, an Emory Autismdoing laundry, or just hanging out with friends. Activities likeCenter pilot program that uses the Emory campus as awoodworking and gardening are included to introduce hobbiesbehavioral training ground for adults with autism. Participantsor potential job skills.are paired with peer volunteers, many of whom are Emorystudents.“They need guidance, patience, and repetition,” saysDoing activities together allows counselors and peervolunteers to give feedback. For example, if a participant sitsright next to a stranger on the shuttle, even when there areCatherine Rice, director of the center, “in terms of helping toseveral other seats available, they can be reminded aboutpractice life skills.”personal space and that this sometimes makes the otherThese skills, selected to foster independence, includeinteracting with others, communicating needs, participatingperson feel uncomfortable.“You want real life to happen,” says Toni Thomas, programin community events, exercising, and getting around onmanager for adult services at the Emory Autism Center. “Youpublic transportation. There is even an apartment on campusdon’t get that in a clinic room.” nSleep 101Want to improve your sleep? David Rye, ofEmory’s sleep medicine program, says it’s allabout the basics. For good sleep hygiene youshould:W Keep a regular scheduleWG o to bed near the same time every nightW Wake up earlyW Get exposure to the sunW D on’t take your cell phone or laptop to bedW Try not to take long napsBack to SchoolRemember school nurses? While the workload for schoolbased clinics has skyrocketed, fewer than half of publicschools in the country now have a nurse on staff, accordingto the National Association of School Nurses. EmoryPediatric Urban Health Program’s school-based clinics aredesigned to help close those gaps in Georgia. They offerregular checkups and dental care along with more urgentcare services. Many offer mental health counselors.“Our primary goal has always been toincrease access to health care in many of ourunderserved areas,” says Veda Johnson,assistant professor of pediatrics, whooversees the program’s Georgiaexpansion efforts. “Nursesare at the core of theseprograms. They are the oneswho know the children anddevelop trust.” nFall 20155
ON OUR RADARNew and noteworthyEmory to lead National Ebola Training and Education CenterNurses Crystal Johnson and Jason Slabachpractice donning and doffing personal protective equipment in Emory University Hopsital’sSerious Communicable Diseases Unit.Because of its experience in helpingfour patients recover from Ebola, Emorywas named by the U.S. Department ofHealth & Human Services to be leadcoordinating center of the National EbolaTraining and Education Center.Emory will collaborate with theUniversity of NebraskaMedical Center,the New York CityHealth and HospitalsCorporation (BellevueHospital), the HHS’sAssistant Secretaryfor Preparedness andResponse, and theCenters for DiseaseControl and Prevention(CDC).The center will supporttraining of health careproviders and facilities on strategies tomanage Ebola virus and other emerginginfectious diseases and will receive 12 million over the next five years.“Based on the knowledge we havegained from caring for patients with Ebolavirus disease, we will develop and teachbest practices to other health care workerswho could be faced with caring for similarpatients in the future,” says Bruce Ribner,medical director of Emory UniversityHospital’s Serious Communicable DiseasesUnit. Ribner will be principal investigatorof the center.Since December 2014, Emory, theUniversity of Nebraska, and the CDC havetrained more than 460 health care workersfrom 87 health care systems on all aspectsof Ebola infection control and patient care.Emory is part of a national network of 55Ebola treatment centers. nStand up!Sitting can be hazardous to your health. That’s right, what you areprobably doing now, even as you read this article, may be increasingyour risk for developing diseases like cancer.Between working at a desk, watching TV, and driving, the averageAmerican spends more than eight hours a day sitting.Alpa Patel, who has an MPH from Emory and is the strategic director ofthe Cancer Prevention Study (CPS)-3 for the American Cancer Society, hasfocused her research on the role of physical activity in cancer preventionand obesity as a risk factor for cancer.Studies have found that people who sit a lot, particularly women,tend to die earlier. Women who sat for more than six hours a day were37 percent more likely to die during the 13 years of the study than thosewho sat for less than three hours a day. Men who sat more than six hoursa day were 18 percent more likely to die than those who sat less than threehours. Researchers estimate that two years of life can be gained by reducingsitting to less than three hours a day.Surprisingly, this level of risk applied even to people who regularly wentto the gym but sat at desk jobs the rest of the day—a group Patel calls “activecouch potatoes.” —Martha McKenzieThe perfect homedeserves theperfect mortgage!PFederally insured by NCUAEM 1214 2.indd 16EMORY MEDICINEEmory Alliance Credit Unionoffers free pre-approvals online24/7 on first mortgages. Comeinto a branch today or visit usonline at emoryacu.com.1237 Clairmont Rd.Decatur, GA 30030404.329.641512/11/14 11:20 AMFall 20157
ON OUR RADARNew and noteworthySecondary comfortsHigh-tech heart helpTwo lifesaving devices havemade it through clinical trialsand are on their way intomore patients’ hearts.The CardioMEMS HF System is the first FDA-approvedheart failure monitoring deviceshown to reduce hospital admissions.The device, invented atGeorgia Tech using jet-enginetechnology, is delivered tothe heart with a catheter andimplanted in the pulmonaryartery, where its paper-clipsized sensor measures interiorpressure. An increase in thispressure can indicate worseningheart failure.Once implanted, thewireless sensor sends regular8pressure readings to an externalelectronic system. “We’re able todetect changes from a distanceand, if needed, adjust a patient’smedication regimen to stabilizepulmonary artery pressures,”says Emory cardiologist RobCole. Cole and colleaguesrecently implanted metroAtlanta’s first FDA-approvedCardioMEMS device, althoughEmory Healthcare has beenoffering the device for years aspart of a clinical trial. The sensor is designed to last a lifetimeand does not require batteries.Also, patients with nonvalvular atrial fibrillation (AFib)now have an alternative tolong-term warfarin medicationwith the Watchman Left AtrialAppendage Closure Implant.During a minimally invasiveprocedure, the implant is delivered to the heart via a catheter,closing off the left atrial appendage (LAA). The LAA is a thin,sack-like appendage attachedto the heart and is thought tobe the source of the majority ofstroke-causing blood clots inpeople with non-valvular AFib.Cardiologist David DeLurgio, director of electrophysiology at Emory Saint Joseph’sHospital, and an Emory teamhave been implanting the devicefor the past seven years in clinical trials, testing the new technology. He recently implantedthe region’s first FDA-approveddevice in the Southeast. nAnd the heart scan shows.You have the powerA simple heart scan can predict early death. The coronaryartery calcification (CAC) scan, an X-ray test that looks forspecks of calcium in the walls of coronary arteries, is helpingphysicians identify patients at risk. These specks, or calcifications,are an early indicator of coronary heart disease. Led by cardiologistLeslee Shaw, researchers from Emory’s Schoolof Medicine collected CAC scores and risk factordata from more than 9,700 volunteers between1996 and 1999. All participants were scanned aspart of a community-outreach screening programat an outpatient clinic in Nashville. None showedsymptoms of coronary artery disease at the time.The findings, published inthe July 7 online issue ofAnnals of Internal Medicine, showed thatCAC scores accurately predicted prematuredeath from all causes up to 15 years inadvance, in patients without any symptoms.“This gives us a better understanding ofthe importance of coronary calcium scans,”Dr. Leslee ShawShaw says. “Patients with high calciumscores might be advised by their physicians to adopt healthierlifestyles, which could lead to better outcomes and help lengthentheir lives.” nPreventable risk factors, such as obesity and smoking,continue to account for half of all heart disease deaths,found Emory researchers. A team led by Shivani Patel, aresearcher in the Hubert Department of Global Health at RollinsSchool of Public Health, studied data from the Behavioral RiskFactor Surveillance System national surveysfrom 2009 to 2010. The goal: to find out howmuch national cardiovascular mortality mightdecrease if all states reduced risk factor levelsto target levels. The top five preventablerisk factors for heart disease are elevatedcholesterol, diabetes, hypertension, obesity,and smoking. The fraction of cardiovasculardeaths that could have been prevented werereported under two scenarios: completely eliminating riskfactors, and the more realistic goal of reducing risk factors torival the best in the US. The findings, published in the June 30issue of Annals of Internal Medicine, suggest that about half ofdeaths could be prevented if the modifiable risk factors werecompletely eliminated. About 10 percent of cardiovasculardeaths could be prevented if all states were to achieve risk factorlevels observed in the best-performing states. “All states couldbenefit from more aggressive policies and programs to helpreduce risk of death from heart disease,” Patel says nEMORY MEDICINEaccess allows the family members to see changes in the patient’shealth status, to be present for bedside shift reports, and to join inopen communication regardingthe patient’s health goals withstaff.Actually, the most importantIn addition to Emory’s unreneeds identified by such familiesstricted visitation policy, the unitwere those that revolved aroundalso provides amenities like apatient information.washer and dryer, sleep rooms forIn a recent survey of 45 familyfamilies staying overnight, familymembers of patients by Emorycounselors, and mentors who areUniversity Hospital’s Neuro-ICU,family members of former ICUthe top-rated needs includedpatients. “Everyone has been greatunrestricted visitation, talkingto us. They answer all questionswith a doctor each day, beingand provide information needed,”assured that the best care is beingsaid one family.provided to the patient, and being Emory University Hospital’s 2D Neuroscience ICU Research TeamThe study found that althoughgiven hope and encouragement.families loved the amenities andEmory’s Neuro-ICU allows continuous family member visitaservices, their main concerns were being kept up to date and welltion in the patient’s room. Having the family present is beneficialinformed about the care provided to their family member, and thefor the patient, the family themselves, and the health care providers, ability to stay with the patient, says Carmen Frobos, the unit’s famsays unit research committee chair Mini Jacob. Unrestricted familyily coordinator. —Aspen Ono 18CYou might think it would be the amenities—like a comfortablereclining chair to sleep in or a washer and dryer to use—thatwould be most appreciated byfamily members of a patient inan intensive care unit.A ClinicalStudy toHelp TreatRecurrentProstateCancerFor more information about the trial, visitwinshipcancer.emory.edu/FACBCinfo.Ashesh Jani, MDPhone: 404-778-3827Email: abjani@emory.eduFall 20159
ON OUR RADARNew and noteworthyEasing Phantom Limb PainAmputees sometimes experienceshooting pains or burning sensations in limbs that are no longerthere. These sensations seem tooriginate in the spinal cord and brain,perhaps because neural pathways arereceiving mixed signals that somethingis not right. A clinical trial by EmorySaint Joseph’s Hospital interventionalradiologist J. David Prologo is studying a minimally invasive treatment, cryoablation therapy, to see if it helps relieve symptoms.Prologo is using CT imaging guidance to position a probe near thenerve responsible for the residual phantom pain. Once the probe isplaced, the temperature is dropped for 25 minutes to create an ablation zone, and the signals the nerve was previously carrying are shutdown. The outpatient procedure takes about one hour, and somepatients have reported significantly decreased pain and improvedfunction. Norma Jean Robinson was one of the first patients to complete the cryoablation therapy at Emory Saint Joseph’s. “On a scale ofone to 10, my [phantom] pain had reached the highest level—a 10,”says Robinson, whose leg had been amputated six months before.“This procedure dramatically changed the quality of my life.” nWhy HIV’s cloak has a long tailEmory virologists have uncovered a critical detailexplaining how HIV assembles its infectious yet stealthyclothing. For HIV to spread from cell to cell, the viral envelopeprotein needs to become incorporated into viral particlesas they emerge from an infected cell. Researchers led byPaul Spearman, Nahmias-Schinazi Professor and vice chairof research in Emory Pediatrics, found that a small sectionof the envelope protein, located on its cytoplasmic “tail,” isnecessary for it to be sorted into viral particles. “Many viralenvelope proteins have very short tails,” Spearman says.“Why HIV envelope has such a long tail has been a mystery.Now we are beginning to understand that HIV uses specifichost cell factors to deliver its envelope protein onto the viralparticle. Not only can this help us design better vaccines,it provides a new target for drugs to inhibit HIV.” The tail isrequired for HIV to infect and replicate in the cellsit prefers: macrophages and T cells. Thelong tail is also thought to help HIV avoidthe immune system, says Eric Hunter,co-director of Emory’s Center for AIDSResearch. nCT cytoplasmic tailFigure modified from image of HIV virion created by Atuhani Burnett.Extraordinary Ebola carecarlos.emory.eduWHERE DISCOVERY BEGINSFree admission for Emory students, staff, and faculty.Emory University Hospital’s Serious CommunicableDiseases Unit team received the National PatientSafety Foundation’s DAISY (Diseases Attacking theImmune System) Award for Extraordinary Nurses.Members of “Team Ebola” were selected for theircare and successful treatment of four critically illEbola patients atEmory last summerand fall. nResearch dollars Researchers in Emory’s WoodruffHealth Sciences Center received nearly 483 million infunding last year, 93 percent of the university total, withnearly 325 million in federal funding, including morethan 288 million from the NIH. n10EMORY MEDICINEThe Case of the Waxing Moon FaceAfter a peripatetic electronic journey, a photo ofa middle-aged schoolteacher found its way tothe cell phone of Clyde Partin, director of Emory’sSpecial Diagnostic Services clinic.“Face is swollen” was the only information thataccompanied the picture.The woman’s head was tilted back, reminiscentof a Vesalius drawing, Partin says, and her neck waserythematous—abnormally red, perhaps from inflammation or infection.Her facial features appeared normal, but she hada tired appearance. Partinagreed to examine her in theSpecial Diagnostic clinic.In his office, he encountered a seemingly exhausted45-year-old woman, slightlyoverweight.She showed him a photoof herself taken at a party. Shewas wearing a college footballjersey, her face thin andyouthful, exceedingly healthyin appearance.“I wondered why she wasshowing me a photo of her college days but she reassured me the photo was taken only five months prior,”he says. “The contrast between her then and now wasstriking and disconcerting. The bloated face was nowfully obvious to me.”She told him that she was, indeed, exhausted andhad gained twenty pounds. “My legs feel so heavy, Ican hardly get up steps,” she said. “And my sideburnsare growing.”Her past medical history included migraine headaches, which were worsening, and neck and back pain.The rest of her exam was mostly unrevealing. Nopurple striae—stretch marks that could be causedby rapid weight gain or certain diseases. No buffalohump, which could indicate certain conditions. Someterminal facial hairs were noted.Neck and facial erythema in a butterfly pattern wasobserved but multiple ANA (antinuclear antibody) labtest results were negative, suggesting lupus was not theculprit. Electrolytes demonstrated a subtle metabolicalkalosis.“How are your neck andback doing?” Partin asked.“Better after the shots,”she replied.“What kind of shots?”“I’m not sure.”“Epidural steroid shots?”“Yes, I think so.”She recalled perhaps10 such shots in the past13 months. And that, carefulreader, was the culprit.Her plethoric, if not fullydeveloped, moon face wasdue to excessive exogenoussteroids. Further lab testingrevealed the presence of synthetic corticosteroids,even though it had been months since her last steroidshot, and suppressed adrenal glands causing a lowendogenous cortisol level.She had received so much steroid her proximal legmuscles were weak from steroid myopathy, explainingher trouble with steps.Her symptoms could be attributed to the steroids,which had produced Cushing’s syndrome. The cure?Mostly time, letting her adrenal glands recover, and atouch of hydrocortisone when needed. nFall 201511
Dr. Steven Yeh checks Ian Crozier’s left eye at afollow-up appointment in June. Crozier developedsevere vision loss months after he recovered froma near-fatal Ebola infection. During testing, liveEbola virus was found inside Crozier’s eyeHiding in Plain SightA lot remains unknown about Dr. Ian Crozier’s left eye. Does it stillharbor the Ebola virus? Is that what made his iris turn fromblue to green? Was Crozier an outlier, or do manyEbola survivors have remaining live virus in their eyes?All that is known, definitively, is that after very nearly takinghis life, Ebola then tried to steal his sight.When his visionSlowly, Crozier hadDr. Ian Crozier survived Ebola but months later,started to deteriorate, itcome back t
at the Emory Rehab Hospital under the direction of Dr. Stewart Factor. I picked up a copy of Emory Medicine and, as a former health care administrator, I found the articles very intellectu-ally stimulating. Our son is enrolled in the Emory School of Nursing and is completing his MSN in the Family Practice NP Program. Emory has been a wonderful .