Transcription
Critical Congenital Heart Disease Screening with PulseOximetry in the Neonatal Intensive Care UnitSatyan Lakshminrusimha MD1, Stephen Turkovich MD1, Veena Manja MD2, JayasreeNair MD1, Vasanth H.S. Kumar MD11Division of Neonatology, Department of Pediatrics, Women and Children’s Hospital of Buffalo, University atBuffalo, Buffalo, NY2Division of Cardiology, Department of Pediatrics, University at Buffalo, Buffalo, NYAuthor Correspondence:Satyan Lakshminrusimha, MDDivision of NeonatologyWomen and Children’s Hospital of Buffalo219 Bryant StBuffalo NY 14222Phone: (716) 878-7673Email: slakshmi@buffalo.eduAuthor Disclosure: The authors have nothing to disclose.ABSTRACTA case study of an infant with interrupted aortic arch who was discharged from the newborn nursery is presented forroot cause analysis and implementation of a modified pulse oximetry screening program at the parent institutionwhere it was described. A rationale for modification of the American Academy of Pediatrics policy statementsupporting universal pulse oximetry screening for congenital heart disease in the newborn is made.Key Words: Pulse oximetry, congenital heart disease, neonate, screeningINTRODUCTIONPulse oximetry has been shown to aid in thedetection of critical congenital heart disease(CCHD) in newborn infants.1-7 TheSecretary of Health and Human Services(HHS) recently suggested addition ofscreening for CCHD to the recommendeduniform screening panel currently inpractice on discharge of a newborn infant.The American Academy of Pediatrics hasalso issued a policy statement stronglysupportingtheSecretary’srecommendation.8 This policy statement istargeted toward healthy newborn infants inthe well-baby nursery. Currently, there aree-Journal of Neonatology Researchno national guidelines for the neonatalintensive care unit (NICU) population.However, screening protocols in the uniformscreening panel such as hearing screen,blood spot test for metabolic, endocrinedisorders and hemoglobinopathy have to beperformed on all infant population includingthe NICU. We present a brief case reporthighlighting the importance of oximetryscreening in the NICU. In the absence ofstandard established protocol for pretermand term infants discharged from the NICU,we suggest a modification to the algorithmrecommended by the AAP,9 for use in theVolume 2, Issue 2, Spring 201296
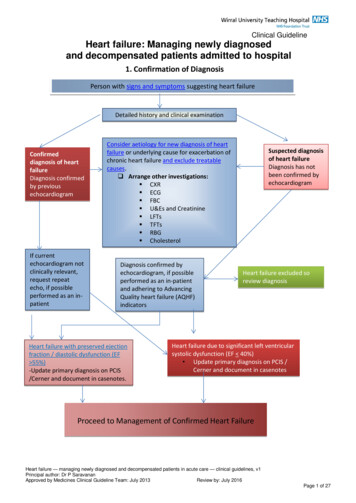
CCHD Screening with Pulse OximetryLakshminrusimha S, et alNICU. This algorithm is currently beingpracticed in our NICU.CASEA 38 week gestation infant was delivered bya repeat cesarean section. The neonate hadrespiratory distress in the delivery roomrequiring intubation. On admission to theNICU, normal blood pressures in all fourextremities (55/39 mmHg in the right upperlimb, 58/44 mmHg in the right lower limb,47/37 mmHg in the left upper limb and56/26 mmHg in the left lower limb) weredocumented. Femoral pulses were normal. Apulse oximeter probe placed on the rightupper limb was 95-98% with 21-25%oxygen requirement. This infant’s first chestX-ray demonstrated bilateral hazy lungfields and is shown in Figure 1. Within 24 h,the baby was extubated and a subsequentchest X-ray showed marked improvement(Figure 2). She was discharged home inroom air with pulse oximeter reading in 98100% in the right upper limb.Two weeks after discharge, she came to thepediatrician’s office for a routine visit andwas noted to have absent femoral pulses. Anechocardiogram demonstrated interruptedaortic arch with an aberrant left subclavianartery arising from the patent ductusarteriosus – PDA (Figure 3). The rightcommon carotid artery, right subclavian andleft common carotid artery came off theproximal part of the aortic arch prior tointerruption (Figure 3).The infantunderwent corrective surgery and wasdischarged home at four weeks of life.Given the fact that the left upper extremityand the lower half of the body were suppliedby the pulmonary artery through the ductus,it is likely that SpO2 obtained from the lefte-Journal of Neonatology Researchupper limb or any lower limb would havedemonstrated a lower SpO2 compared to theright hand. During her stay in the NICU, allSpO2 readings were obtained from the righthand.Volume 2, Issue 2, Spring 201297
CCHD Screening with Pulse OximetryLakshminrusimha S, et alreported prenatal detection rates 50% forfunctional single ventricle lesions, althoughthe detection rate is generally 30% forCCHD with two-ventricle circulation and/orabnormal outflow view (such as totalanomalous pulmonary venous return,transposition of great vessels and aortic archabnormalities).11-15 In a study from UK,Brown et al reported that recognition ofCHD was antenatal in 20%, postnatal ward(before discharge) in 55% and afterdischarge to home in 25%.16 Cardiovascularcompromise and end organ dysfunctionwere least likely when recognition wasantenatal and most common whenpresentation followed discharge to home.The detection of co-arctation of the aorta bypulse oximetry screening is only 53% (3075% – 95% confidence interval)10 but theprecise detection rate for interrupted aorticarch is not known. The accuracy of thisscreening is variable with high specificitybut low sensitivity.6 Currently most units donot offer CCHD screenings for all infantsadmitted to the NICU. There always existsa potential for a positive screen, such as in apatient described above, provided all NICUpatients are screened for CCHD. We havedeveloped a modified algorithm, for allpatients admitted to the NICU. Hospitalslocated at high altitude have to come up withprotocols to compensate for low SpO2readings secondary to reduced barometricpressure.Critical congenital heart disease (CCHD) isdefined as CHD requiring surgery orcatheter intervention in the first year of lifeand accounts for approximately one quarterof all children with CHD.10 Timelyrecognition of CCHD by pulse oximetrycould improve outcomes. In the US, manycongenital surgery referral centers havee-Journal of Neonatology ResearchThe establishment of a cutoff threshold foran abnormal SpO2 must be associated withhigh sensitivity and specificity. Setting ahigh SpO2 cutoff value closer to the normallevel will decrease the number of falsenegative screening results at the cost ofincreasing the number of false-positiveresults. Conversely, a lower SpO2 thresholdwill lower sensitivity and raise specificity.10The screening protocol as recommended bythe AAP working group considers a positivescreening result as (1) any oxygen saturationmeasure 90%, (2) oxygen saturation 95% in both extremities on three measures,each separated by one hour, or (3) anabsolute 3% difference in oxygensaturation between the right hand and footon three measures, each separated by onehour. Any screening that is 95% in eitherextremity with 3% absolute difference inoxygen saturation between the upper andlower extremity would be considered a“pass” result and screening would end.9In general, the mean difference between theoxygen saturation in the upper and lowerextremities is 1% after the first 24h of life;however, some newborns with CCHD, suchas aortic arch abnormalities may have moreVolume 2, Issue 2, Spring 201298
CCHD Screening with Pulse Oximetrye-Journal of Neonatology ResearchLakshminrusimha S, et alVolume 2, Issue 2, Spring 201299
CCHD Screening with Pulse OximetryLakshminrusimha S, et alprofound difference in saturation as theductus arteriosus supplies part of thesystemic flow (Figure 3). Adding adifference of 3% between right hand andfoot oxygen saturation enhanced thesensitivity of screening using a cutoff of 95%3 from 89.4% to 92.4%. The work grouprecommended that screening be performedwith motion-tolerant pulse oximeters thatreport functional oxygen saturation, havebeen validated in low-perfusion conditions,have been cleared by FDA for use innewborns, and have a 2% root-mean-squareaccuracy.9The modified algorithm presented in Figure4 suggests that neonates requiring oxygensupplementation during their NICU stay beweaned to room air for at least 24 h prior toscreening. Infants who are being dischargedon home oxygen need to undergo anechocardiogram (if one was not obtainedduring their neonatal course).CONCLUSIONWe used a root cause analysis to modify theAAP guidelines for pulse oximetryscreening in order to improve its specificityand sensitivity for aortic arch abnormality inour NICU. These recommendations areempirical, not evidence based and needcritical evaluation by prospective studies.Collaborative studies among neonatalintensive care units conducting routine pulseoximetry should analyze pooled data andreport detection, false positive rates, falsenegative rates, and cost-effectiveness ofthese screening measures for CCHD.REFERENCES1.Koppel RI, Druschel CM, Carter T, GoldbergBE, Mehta PN, Talwar R, et al. Effectiveness ofpulse oximetry screening for congenital heartdisease in asymptomatic newborns. Pediatrics2003; 111(3):451-5.2.Bakr AF, Habib HS. Combining pulse oximetryand clinical examination in screening forcongenital heart disease. Pediatr Cardiol 2005;26(6):832-5.3.de Wahl Granelli A, Mellander M, Sunnegardh J,Sandberg K, Ostman-Smith I. Screening forduct-dependant congenital heart disease withpulse oximetry: a critical evaluation of strategiesto maximize sensitivity. Acta Paediatr2005;94(11):1590-1596.4.Rosati E, Chitano G, Dipaola L, De Felice C,Latini G. Indications and limitations for aneonatal pulse oximetry screening of criticalcongenital heart disease. J Perinat Med 2005;33(5):455-7.5.Ruangritnamchai C, Bunjapamai W, PongpanichB. Pulse oximetry screening for clinicallyunrecognized critical congenital heart disease inthe newborns. Images Paediatr Cardiol 2007;9(1):10-5.e-Journal of Neonatology Research6.Thangaratinam S, Daniels J, Ewer AK, ZamoraJ, Khan KS. Accuracy of pulse oximetry inscreening for congenital heart disease inasymptomatic newborns: a systematic review.Arch Dis Child Fetal Neonatal Ed 2007;92(3):F176-80.7.Mahle W, Koppel R. Screening with pulseoximetry for congenital heart disease. Lancet2011; 378(9793):749-50.8.Mahle WT, Martin GR, Beekman RH 3rd,Morrow WR. Endorsement of Health andHuman Services recommendation for pulseoximetry screening for critical congenital heartdisease. Pediatrics 2012; 129(1):190-2.9.Kemper AR, Mahle WT, Martin GR, CooleyWC, Kumar P, Morrow WR, et al. Strategies forimplementing screening for critical congenitalheart disease. Pediatrics 2011; 128(5):e1259-67.10. Mahle WT, Newburger JW, Matherne GP, SmithFC, Hoke TR, Koppel R, et al. Role of pulseoximetry in examining newborns for congenitalheart disease: a scientific statement from theAmerican Heart Association and AmericanAcademy of Pediatrics. Circulation 2009;120(5):447-58.Volume 2, Issue 2, Spring 2012100
CCHD Screening with Pulse OximetryLakshminrusimha S, et al11. Hancock Friesen CL, Zurakowski D, ThiagarajanRR, Forbess JM, del Nido PJ, Mayer JE, et al.Total anomalous pulmonary venous connection:an analysis of current management strategies in asingle institution. Ann Thorac Surg 2005;79(2):596-606; discussion 596-606.12. Brown JW, Park HJ, Turrentine MW. Arterialswitch operation: factors impacting survival inthe current era. Ann Thorac Surg 2001;71(6):1978-84.13. Sharland G. Fetal cardiac screening and variationin prenatal detection rates of congenital heartdisease: why bother with screening at all? FutureCardiol 2012; 8(2):189-202.14. Pinto NM, Keenan HT, Minich LL, PuchalskiMD, Heywood M, Botto LD. Barriers to prenataldetection of congenital heart disease: Apopulation based study. Ultrasound ObstetGynecol 2011 Oct 13, [Epub ahead of print].15. Friedberg MK, Silverman NH, Moon-Grady AJ,et al. Prenatal detection of congenital heartdisease. J Pediatr 2009; 155(1):26-31, e21.16. Brown KL, Ridout DA, Hoskote A, Verhulst L,Ricci M, Bull C. Delayed diagnosis of congenitalheart disease worsens preoperative condition andoutcome of surgery in neonates. Heart 2006;92(9):1298-302.e-Journal of Neonatology ResearchVolume 2, Issue 2, Spring 2012101
Key Words: Pulse oximetry, congenital heart disease, neonate, screening . INTRODUCTION. Pulse oximetry has been shown to aid in the detection of critical congenital heart disease (CCHD) in newborn infants. 1-7. The . "pass" result and screening would end. 9 . In general, the mean difference between the oxygen saturation in the upper and lower