Transcription
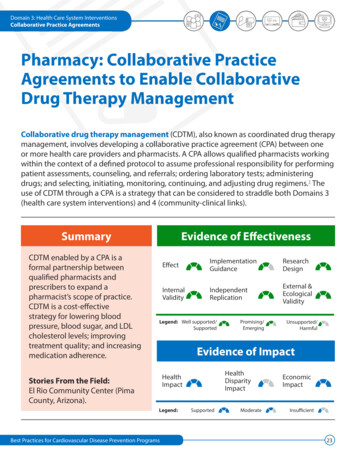
Domain 3: Health Care System InterventionsCollaborative Practice AgreementsPharmacy: Collaborative PracticeAgreements to Enable CollaborativeDrug Therapy ManagementCollaborative drug therapy management (CDTM), also known as coordinated drug therapymanagement, involves developing a collaborative practice agreement (CPA) between oneor more health care providers and pharmacists. A CPA allows qualified pharmacists workingwithin the context of a defined protocol to assume professional responsibility for performingpatient assessments, counseling, and referrals; ordering laboratory tests; administeringdrugs; and selecting, initiating, monitoring, continuing, and adjusting drug regimens.1 Theuse of CDTM through a CPA is a strategy that can be considered to straddle both Domains 3(health care system interventions) and 4 (community-clinical links).SummaryCDTM enabled by a CPA is aformal partnership betweenqualified pharmacists andprescribers to expand apharmacist’s scope of practice.CDTM is a cost-effectivestrategy for lowering bloodpressure, blood sugar, and LDLcholesterol levels; improvingtreatment quality; and increasingmedication adherence.Evidence of l &EcologicalValidityLegend: Well armfulEvidence of ImpactHealthDisparityImpactHealthImpactStories From the Field:El Rio Community Center (PimaCounty, Arizona).Legend:Best Practices for Cardiovascular Disease Prevention t23
Domain 3: Health Care System InterventionsCollaborative Practice AgreementsEvidence of EffectivenessStrong evidence exists that CDTM enabled by a CPA is effective. Solid evidence exists that this strategy achieves desired outcomes,with studies demonstrating internal and external validity. This strategy has also been independently replicated, and systematicreviews assessing the use of CDTM have confirmed reliability of impact. Implementation guidance on CPAs to enable CDTM wasfound to be lacking in comprehensiveness.Evidence of ImpactHealth ImpactHealth Disparity ImpactEconomic ImpactCDTM, enabled by CPAs betweenpharmacists and other health careproviders, has been shown effective inimproving clinical and behavioral healthindicators, including lowering bloodpressure, HbA1c, and LDL cholesterollevels; improving treatment qualitythrough pharmacist compliance withclinical guidelines; and increasingpatient knowledge and adherence tomedication regimens.2The goals of reaching populations atrisk and reducing health disparitieshave been taken into account in thedevelopment and implementationof CPAs, particularly by pharmacyorganizations (e.g., the AmericanPharmacists Association), state medicaland pharmacy boards, and statepharmacy organizations. However, nostudies have directly examined theimpact of CPAs between pharmacistsand providers serving low-incomepopulations. Because pharmacistsoften work directly with the public incommunity settings, they are oftenconsidered the public’s most accessiblehealth care providers. CPAs canauthorize pharmacists to make changesto a patient’s medication or dosage,which can reduce the number of visitsa patient has to make and lower costs,while also making it easier for patientsto adhere to their medications.Research suggests that clinicalpharmacy services like CDTM canbe cost-saving to the health caresystem, primarily through avoidedhospitalizations and emergency room(ER) visits.3 For example, in 2006,Missouri’s Pharmacy-Assisted CDTMprogram resulted in a 12% decreasein any-cause hospitalizations, a 25%reduction in ER visits, and a decreasein drug-related problems amongbeneficiaries after 1 year. This programwas also found to have a 2.5 to 1 ROI tothe state, with an estimated savings of 518.10 per patient per month.3Best Practices for Cardiovascular Disease Prevention ProgramsStrong evidence exists that CDTMenabled by a CPA is effective.24
Stories from the FieldCollaborative Practice AgreementsCPAs at El Rio Community CenterEl Rio Community Health Center serves over 75,000 people inPima County, Arizona. In 2011, 20% of El Rio’s adult patients (8,954of 44,952) had diagnosed hypertension, but only 67% of thosediagnosed had the condition under control. Pharmacists at ElRio were encouraged to establish CPAs with the center’s medicalproviders. These agreements enable pharmacists to work directlywith patients to help them manage their hypertension and otherchronic conditions, such as diabetes and hyperlipidemia. Withinthe scope of the CPA, pharmacists have the discretion to changepatient medications. After CDTM was implemented, El Rio reportedimproved clinical outcomes (e.g., lower cholesterol and bloodpressure levels), increased use of recommended screenings, andreduced ER visits. The El Rio case study highlights several importantconsiderations for CDTM implementation. These considerationsinclude instilling mission-driven values through training andorientation, accepting pharmacy student interns, and using broadstrategies and networks to improve patient care and increasepotential partnerships that may extend the use of CPAs.For more information:Phone: 520-670-3909Website: www.elrio.org
Domain 3: Health Care System InterventionsCollaborative Practice AgreementsFour Considerations for Implementation1SettingsEnabling CDTM through CPAs has been found to be effective in several clinical and community settings,including federally qualified health centers (FQHC), patient-centered medical homes, managed care healthsystems, community pharmacies, hospital pharmacies, and primary care clinics.2Policy and Law-Related ConsiderationsCPAs are typically authorized through state scope-of-practice laws that may or may not allow for theiruse within pharmacist scope-of-practice laws. Challenges associated with billing for services exist, evenat the federal level.12,13 When a CPA is developed, the pharmacist and the prescriber work together todevelop the terms of the CPA. They may use recommendations and model language available from variousorganizations.5,6,143Implementation GuidanceCDC has recently developed a CPA tool kit that provides implementation guidance: Advancing Team-Based Care Through Collaborative Practice Agreements: A Resource andImplementation Guide for Adding Pharmacists to the Care Team.4Guidance from the state level comes from the following sources: National Association of State Pharmacy Associations.5 American Pharmacy Association.64ResourcesSeveral guides and examples are available to educate and guide health care providers, decision makers,insurers, and pharmacists about how pharmacists and other health care providers can better servepatients through CPAs and CDTM. Examples include the following: Collaborative Practice Agreements and Pharmacists’ Patient Care Services: A Resource for Pharmacists.7 A Resource for Nurses, Physician Assistants, and Other Providers.8 A Resource for Government and Private Payers.9 A Program Guide for Public Health: Partnering with Pharmacists.10 Agency for Healthcare Research and Quality, Pharmacy Quality Alliance.11Best Practices for Cardiovascular Disease Prevention Programs26
Domain 3: Health Care System InterventionsCollaborative Practice AgreementsReferences1. Hammond RW, Schwartz AH, CampbellMJ, et al. Collaborative drug therapymanagement by pharmacists—2003.Pharmacotherapy. 2003;23:1210–1225.2. Chisholm-Burns MA, Kim Lee J, SpiveyCA, et al. US pharmacists’ effect as teammembers on patient care: systematicreview and meta-analyses. Med Care.2010;48(10):923–933.3. US Department of Health and HumanServices. Special Report to the SenateAppropriations Committee on AdvancingClinical Pharmacy Services in ProgramsFunded by the Health Resources andServices Administration and Its Safety-NetPartners. Washington, DC: US Departmentof Health and Human Services; 2008.4. Centers for Disease Control andPrevention. Advancing Team-Based CareThrough Collaborative Practice Agreements:A Resource and Implementation Guidefor Adding Pharmacists to the Care Team.Atlanta, GA: Centers for Disease Controland Prevention, US Dept of Health andHuman Services; 2017.5. Weaver K. Pharmacist CollaborativeAgreements: Key Elements for Legislativeand Regulatory Authority. Richmond, VA:The National Alliance of State PharmacyAssociations; 2015.6. American Pharmacists Association.Collaborative Practice Agreements: NASPAWorkgroup Releases Recommendationswebsite. .Accessed February 14, 2017.10. Centers for Disease Control andPrevention. A Program Guide for PublicHealth: Partnering with Pharmacists in thePrevention and Control of Chronic Diseases.Atlanta, GA: Centers for Disease Controland Prevention, US Dept of Health andHuman Services; 2012.7. Centers for Disease Control andPrevention. Collaborative PracticeAgreements and Pharmacists’ PatientCare Services: A Resource for Pharmacists.Atlanta, GA: Centers for Disease Controland Prevention, US Dept of Health andHuman Services; 2013.11. Agency for Healthcare Research andQuality. New Models of Primary CareWorkforce and Financing Case Example#3: Fairview Health Services. Rockville,MD: Agency for Healthcare Research andQuality; 2016.8. Centers for Disease Control andPrevention. Collaborative PracticeAgreements and Pharmacists’ Patient CareServices: A Resource for Doctors, Nurses,Physician Assistants, and Other Providers.Atlanta, GA: Centers for Disease Controland Prevention, US Dept of Health andHuman Services; 2013.9. Centers for Disease Control andPrevention. Collaborative PracticeAgreements and Pharmacists’ Patient CareServices: A Resource for Government andPrivate Payers. Atlanta, GA: Centers forDisease Control and Prevention, US Deptof Health and Human Services; 2013.Best Practices for Cardiovascular Disease Prevention Programs12. McBane S, Dopp A, Abe A, et al. ACCPwhite paper: collaborative drug therapymanagement and comprehensivemedication management - 2015.Pharmacotherapy. 2015;35(4):e39–e50.13. Centers for Disease Control andPrevention. Select Features of StatePharmacist Collaborative Laws. Atlanta,GA: Centers for Disease Control andPrevention, US Dept of Health and HumanServices; 2013.14. National Association of Boards ofPharmacy. Model State Pharmacy Act/Rules website. edocuments/model-pharmacy-act-rules/.Accessed May 18, 2017.27
Collaborative Practice Agreements 26 Four Considerations for Implementation 1 Settings Enabling CDTM through CPAs has been found to be effective in several clinical and community settings, including federally qualified health centers (FQHC), patient-centered medical homes, managed care health