Transcription
Skills inClinical NursingNinth EditionAudrey Berman, PhD, RNProfessor, School of NursingSamuel Merritt UniversityOakland, CaliforniaShirlee J. Snyder, EdD, RNRetired Dean and Professor, NursingNevada State CollegeHenderson, NevadaA01 BERM1444 09 SE FM.indd 119/11/2019 18:56
Senior Vice President, Product Management: Adam JaworskiSenior Vice President, Content Strategy and Management:Paul CoreyDirector, Product Management: Katrin BeacomProduct Manager: John GoucherDevelopment Editor: Teri ZakPortfolio Management Assistant: Taylor ScuglikManaging Producer, Health Science: Melissa BasheContent Producer: Michael GiacobbeFull Service Project Management and Composition: SPi GlobalVice President, Product Marketing: David GesellInterior Design and Cover Design: Studio MontageSenior Product Marketing Manager:Field Marketing Manager:Printer/Binder:Cover Printer:Cover Image:Copyright 2021, 2016, 2012, 2009 by Pearson Education, Inc. All rights reserved. Manufactured in the United States of America. Thispublication is protected by Copyright and permission should be obtained from the publisher prior to any prohibited reproduction, storage ina retrieval system, or transmission in any form or by any means, electronic, mechanical, photocopying, recording, or likewise. For informationregarding permission(s), write to: Rights and Permissions Department, 221 River Street, Hoboken, New Jersey 07030.Notice: Care has been taken to confirm the accuracy of information presented in this book. The authors, editors, and the publisher, however,cannot accept any responsibility for errors or omissions or for consequences from application of the information in this book and make nowarranty, express or implied, with respect to its contents.The authors and publisher have exerted every effort to ensure that drug selections and dosages set forth in this text are in accord with currentrecommendations and practice at time of publication. However, in view of ongoing research, changes in government regulations, and theconstant flow of information relating to drug therapy and drug reactions, the reader is urged to check the package inserts of all drugs for anychange in indications of dosage and for added warnings and precautions. This is particularly important when the recommended agent is a newand/or infrequently employed drug.Library of Congress Cataloging-in-Publication DataBerman, Audrey, author.Skills in clinical nursing / Audrey Berman and Shirlee Snyder. — Ninth edition.p.; cm.Includes bibliographical references and index.ISBN-13: 978-0-13-542144-4ISBN-10: 0-13-542144-6I. Snyder, Shirlee, author. II. Title.[DNLM: 1. Nursing Care—Handbooks. 2. Nursing Process—Handbooks. WY 489ISBN-10: 0-13-542144-6ISBN-13: 978-0-13-542144-4A01 BERM1444 09 SE FM.indd 219/11/2019 18:56
DedicationAudreyagain dedicates this book to her child, Jordanna Elise MacIntyre, who hasevolved and matured just as has the book itself. Also, like the book, Jordanna seeksto—and will—make the world a healthier and better place.Shirlee again dedicates this book to her husband, Terry J. Schnitter, for his continuallove and support; to the nurses, present and future, who contribute to the nursingprofession; to her step-children ( Kelly and Steven), grandchildren (Ashley, Brady, andRyan), and first great-grandchild (Oliver); to her younger brother, Dan Snyder, and hiswonderful family; and in memory of her older brother, Ted Snyder, who is missed byhis loving and caring family.A01 BERM1444 09 SE FM.indd 319/11/2019 18:56
AcknowledgmentsSpecial thanks to those without whom this edition would not have been possible: Teri Zak, Development Editor, whose unfailing energy, intelligence, memory, experience, and professionalism supported each aspect of the book’s creation. John Goucher, Product Manager, for his support for enhancing and marketingthis book. Michael Giacobbe, Pearson Content Producer, and Meghan DeMaio and PattyDonovan, SPi editorial project managers, whose efforts ensured a quality andtimely production. The reviewers, who provided many helpful comments.ivA01 BERM1444 09 SE FM.indd 419/11/2019 18:56
Thank YouWe extend thanks to our contributors from previous editions, who gave their time, effort,and expertise to the development and writing of chapters and resources that helpedfoster our goal of preparing student nurses for clinical practice.C ONTR IB UTORS TO TH E SEVENT H E DIT IO NJanet Adams, MSN, RT (AART), RNKathleen Kunkler, MS, BSNJanice L. Reilly, EdD, MSN, RN-BCSoutheast Missouri State UniversityCapital UniversityImmaculata UniversityCape Girardeau, MOColumbus, OHImmaculata, PABetty M. L. Bedner, RN, MSN/EdLora McDonald McGuire, MS, BSNMelissa Schmidt, PhD, MSN, BSNUniversity of Pittsburgh BradfordJoliet Junior CollegeTompkins Cortland Community CollegePittsburgh, PAJoliet, ILDryden, NYAnnette Gunderman, DEd, MSN, RNGail Rattigan, MSN, RN, FNP-BCRuby Wertz, MSHA, BSN, RNAssociate Professor of NursingBloomsburg UniversityNevada State College School of NursingNevada State College School of NursingHenderson, NVHenderson, NVBloomsburg, PAREVIEWERS OF THE NINTH EDITIONWe would like to express our sincere thanks to the educators who reviewed chapters of this text. Their insights, comments, suggestions, criticisms, and encouragement contributed to making this a more useful and relevant tool forstudents.Andrea Ackermann, PhD, RN, CNEMount Saint Mary CollegeNewburgh, NYKaren Cooper, MSN, RN, CNETyler Junior CollegeTyler, TXChristy Lenahan, DNP, MSN, FNP-BC, CNEUniversity of Louisiana at LafayetteLafayette, LALynn Barton, MSN, RN, CNSOregon Coast Community CollegeNewport, ORSally Davis, RN, MSN, CNEWestern Technical CollegeLa Crosse, WICatharine Muskus, MS, RN, FNP-BC, CNERasmussen CollegeOcala, FLMitzi Bass, MPH, MSN, RNBaltimore City Community CollegeBaltimore, MDJenny Elbracht, RN, MSNNebraska Methodist CollegeOmaha, NESusan Randol, MSN, RN, CNEUniversity of Louisiana LafayetteLafayette, LAWendy Batch-Wilson, DNP, RNCuyahoga Community CollegeCleveland, OHTracy George, DNP, APRN-BC, CNEFrancis Marion UniversityFlorence, SCJackie Reils, MSN, RNWestern Technical CollegeLa Crosse, WIKellie Bryant, DNP, WHNPNew York UniversityNew York, NYRuth Henderson, RN, MSN, CCRNMedical University of South CarolinaCharleston, SCLinda Shubert, MSN, RNJacksonville UniversityJacksonville, FLKatherine Houle, RN, MSN, CPANChristie Cavallo, MSN, RNGillette Children’s Specialty HealthcareUniversity of Tennessee Health Science CenterSt. Paul, MNMemphis, TNvA01 BERM1444 09 SE FM.indd 519/11/2019 18:56
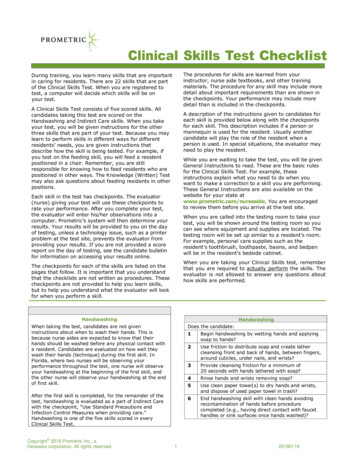
PrefaceThe skills performed by nurses exemplify the integrationof the knowledge, psychomotor dexterity, attitude, andcritical thinking necessary for effective clinical practicein the 21st century. The ninth edition of Skills in Clinical Nursing has been revised and updated to reflect thechanges in practice that have occurred since the previousedition. It includes: The 161 most important skills performed by nurses,including all common variations, organized from thesimple to the more complex. All skills have been revisedto reflect current clinical practice. More than 800 illustrations. Skills in Clinical Nursing isintended as a primary textbook for nursing educationprograms and as a reference for practicing nurses. Content was selected based on feedback from reviewers ofprevious editions, market surveys, and the extensiveteaching and practice experience of the authors.All content was reviewed by practicing clinical nurseswho provided invaluable firsthand knowledge of currentpractice.F O R M ATEach chapter contains concise introductory material, placing the skills in perspective to client anatomy, physiology,and pathophysiology, and provides an overview of therationale and purpose of the skills. The presentation ofeach skill follows the steps of the nursing process: A review of the assessment data required before performing the skill. During diagnosing, the second phase of the nursingprocess, the nurse uses critical thinking skills to interpret specific assessment data and identify the client’sstrengths and problems. The authors did not includethis step of the nursing process for the skills in this bookbecause the focus is on the skill and no specific clientassessment data are included. Application of nursingdiagnoses is reflected in each end-of-unit feature on thenursing process. As a component of the planning phase, informationabout when it is and is not appropriate to assign eachskill to assistive personnel (AP). Implementation steps, including client teaching, observation of standard infection prevention precautions, andclient record documentation. Rationales are indicatedby italic type. Considerations in evaluation of the skill, focusing onsteps indicated for follow-up and communication withother members of the healthcare team.HIGHLIGHTS OF THE 9TH ED IT I ON Emphasis on QSEN! The delivery of high-quality andsafe nursing practice is imperative for every nurse.This edition has incorporated QSEN competencies andspecified expectations into the narrative. This contenthighlights relevant information in patient-centered care,teamwork and collaboration, and safety. Updated art! Many new photos and drawings Current CDC and WHO definitions and guidelines 2019 National Patient Safety Goals (NPSGs) for hospitals and long-term care Current CMS guidelines for use of restraints Healthy People 2020 objectives for cholesterol, hypertension, and diabetes Updated Infusion Nurses Society guidelines Updated nursing standards and references (ANA,NPSG, and so on)viA01 BERM1444 09 SE FM.indd 619/11/2019 18:56
Features of the Ninth Edition704Unit 8 Wounds and Injury CareNURSING PROCESS: SUTURES AND STAPLESSkills in ClinicalNursingRemoving Sutures and StaplesASSESSMENTAssess:SKILL 31.6continues to be a definitiveresource for the mostcommonly performednursing skills. This skillsbook is designed as aneasy reference for boththe classroom and clinicalpractice!Skills are organized in anursing process frameworkand include step-by-stepinstructions.Easy-to-find RAT ION A LES provide abetter understanding of why criticalsteps are performed. Appearance of the suture lineFactors contraindicating suture removal (e.g., nonuniformity of closure, inflammation, presence of drainage).PLANNINGBefore removing skin sutures, verify (a) the orders for suture removal(many times only alternate interrupted sutures or staples are removedone day and the remaining sutures or staples are removed a day ortwo later); (b) when the client may bathe or shower; and (c) whether adressing is to be applied following the suture removal. Some primarycare providers prefer no dressing; others prefer a small, light gauzedressing to prevent friction by clothing.AssignmentRemoval of sutures or staples requires application of knowledge andproblem-solving and is not assigned to AP.IMPLEMENTATIONPerformance1. Prior to performing the procedure, introduce yourself and verifythe client’s identity using agency protocol. Explain to the clientwhat you are going to do, why it is necessary, and how toparticipate. Inform the client that suture removal may produceslight discomfort, such as a pulling or stinging sensation, butshould not be painful.2. Perform hand hygiene and observe other appropriate infectionprevention procedures.3. Provide for client privacy.4. Apply clean gloves, remove any dressings, and clean the incision (see Skill 31.4). Clean the suture line with an antimicrobial solution beforeand after suture or staple removal. Rationale: This is generally done as a prophylactic measure to prevent infection.5. Remove the sutures or staples. Apply sterile gloves.Plain Interrupted Sutures Grasp the suture at the knot with a pair of forceps. Place the curved tip of the suture scissors under thesuture as close to the skin as possible, either on theside opposite the knot ❶ or directly under the knot.EquipmentWaterproof bagSterile glovesSterile dressing equipment including:Sterile suture scissors or staple removerGauze squaresSterile hemostat or forcepsSterile butterfly tape or Steri-Strips (optional)Tape, if a dressing is to be applied Cut the suture. Rationale: Sutures are cut as close to theskin as possible on one side of the visible part becausethe visible suture material is contaminated with skinbacteria and must not be pulled beneath the skin duringremoval. Suture material that is beneath the skin is considered free from bacteria. With the forceps or hemostat, pull the suture out inone piece. Inspect carefully to make sure that all suturematerial is removed. Rationale: Suture material leftbeneath the skin acts as a foreign body and causesinflammation. Discard the suture onto a piece of sterile gauze or intothe moisture-resistant bag, being careful not to contaminate the forceps tips. Sometimes, the suture sticks to theforceps and needs to be removed by wiping the tips on asterile gauze.Staples Place the lower tips of the sterile staple remover underthe staple. Squeeze the handles together until they are completelyclosed. ❷ Rationale: Pressing the handles together causesthe staple to bend in the middle and pulls the edges of thestaple out of the skin. Do not lift the staple remover whensqueezing the handles.CR ITIC A L S T EPS are visually represented with full-color photos and illustrations.❶ Removing a skin suture.Bojan Fatur/Getty Images.M31B BERM1444 09 SE C31.indd 704❷ Removing surgical clips or staples.14/11/2019 18:55viiA01 BERM1444 09 SE FM.indd 719/11/2019 18:56
450Unit 5 Medication AdministrationAdministering Intermittent Intravenous Medications—continuedSKILL 17.8 When the medication has been infused, disconnect the9. After infusion of the secondary IV medication bag, regulate therate of the primary solution by adjusting the clamp or IV pumpIV tubing, maintaining sterility of the end of the IV tubing. Insert the second saline syringe into the port and flush at theinfusion rate. Some infusion pumps will do this automatically.10. Leave the secondary piggyback bag and tubing in place forsame rate that the drug was injected until the entire drug dosefuture administration or discard as appropriate.has been cleared from the infusion system and vascular access11. Document relevant data.device lumen. Rationale: This clears the tubing and maintains Record the date, time, medication, dose, route, andpatency. Clamp the saline lock after flushing, if appropriate. Dispose of syringes in the appropriate container.solution; assessment of the IV site, if appropriate; and theclient’s response.Variation: Adding a Medication to a Volume-Control Infusion Record the volume of fluid of the medication infusion bag Withdraw the required dose of the medication into a syringe.on the client’s intake and output record. Ensure that there is sufficient fluid in the volume-control fluidVariation: Using a Saline Lockchamber to dilute the medication. Generally, at least 50 mL ofIntermittent infusion devices ❺ may be attached to an IV catheter tofluid is used. Check the directions from the drug manufacturerallow medications to be administered intravenously without requiringor consult the pharmacist.a continuous IV infusion. The device may also have a port at one end Close the inflow to the fluid chamber by adjusting the upperof the lock and a needleless injection cap at the other end, with theroller or slide clamp above the fluid chamber; also ensure thatextension tubing between the two ends. ❻the clamp on the air vent of the chamber is open. Prepare two normal saline prefilled syringes (10 mL each). Clean the medication port on the volume-control fluid chamber Spike the medication bag with minidrip (60 gtt/mL) IV tubing.with an antiseptic swab. Attach the needleless adapter to the tubing, prime the tubing, Inject the medication into the port of the appropriately filledand close the clamp.volume-control set (i.e., the ordered amount of solution). Clean the needleless injection port of the saline lock with an Gently rotate the fluid chamber until the fluid is well mixed. Regulate the flow by adjusting the lower roller clamp below theantiseptic swab. Open the saline lock clamp, if appropriate.fluid chamber.Insert the first saline syringe into the port, flush 1 to 2 mL, Attach a medication label to the volume-control fluidand then gently aspirate to check for patency. Flush the remainchamber.ing volume slowly, noting any resistance, swelling, pain, or burning. Document relevant data and monitor the client and theRationale: This ensures placement of the IV in the vein.infusion.and mayeitherpotentiallyharmful. ForAfter connectingthe IVbetubingto theharmlessinjection port orof thelock,administer the medication, regulating the drip rate to allow medicationexample,digitalisincreasesthestrengthof myocardialto infuse for the appropriate time period. Macrodrip (10 to 20 gtt/mL)tubing mayalso be used if usingan IV pumpto regulatethe itflow.contractions(desiredeffect),butcan have the side effectVAR IATIO NS present alternativemethods of performing certain skills.376Unit 5 Medication Administration448of nausea and vomiting. Some side effects are toleratedfor the drug’s therapeutic effect; more severe side effects,also called adverse effects or reactions, may justify thediscontinuation of a drug. The nurse should monitor fordose-related side or adverse effects and report these to theUnit 5 MedicationAdministrationhealthcareproviderwho may discontinue the medicationor change the dosage.the primary infusion container so that the medication isadministered through the client’s IV line. Volume-controlsets are frequently used to infuse solutions into childrenMedication Ordersand older clients when the volume administered is critical and must be carefully monitored. Skill 17.8 providesadditional information.❺ Intermittentinfusion devicePROCESS:with an injection port.Intermittent infusion deviceINFUSIONSwith an injection port and extension tubing.NURSINGINTERMITTENT ❻INTRAVENOUSSKILL 17.8A physician usually determines the client’s tionsa Secondary Piggyback Setneeds andIntermittentorders medications,althoughin some Usingsettings Compare to previous findings, if available. Conduct appropriate follow-up such as desired effect ofnurseandphysician Report (PAs)significantcandeviations from normal to the primarymedication,anypractitionersadverse reactions or sideeffects,or change assistantsASSESSMENTprovider.ifnursesigns. in vital palpate theIV insertionsite forlawsigns ofinfection,Determinethe client has allergies to the medication(s). Reassess status of the IV lock site and patency of the Check the compatibility of the medication, primary IV fluid, andinfiltration, or a dislocated yand theinfusion.the surrounding skin for redness, pallor, or swelling. IV Inspectany medication(s) in the primary IV bag. DeterminePalpatethe surroundingtissuestenderness,coldness,classesof chdrug action, side effects, normal dosage,the presence of edema, which could indicate leakage of therecommended administration time, and peak action time.healthwill have its own policies.Usually CheckIV fluidinto theagencytissues.patency theof the IV line by assessing flow rate. Takevital signsbaseline dataif the medicationbeingintoverbala vein byvenipuncture or into an existing IV lineorderis forwritten,althoughtelephoneandordersadministered is particularly potent.through an injection port or through an IV lock. Intravenous Pusharepushacceptablein issomeNursingstudents needIntravenous(IVP) or bolusthe IVagencies.administrationofThere are two major disadvantages to this method ofASSIG NME N T highlights guidelinesfor when it is appropriate and how toassign skills to a ssistive personnel (AP).an PLANNINGundiluteddrug directlyinto the systemicto knowthe agencypoliciescirculation.about medicationorders.Any error in administration cannotdrugadministration:EquipmentIt isAssignmentuseda medicationcannotbe diluted oronlyin an licensedbe correctedafterthe drug has entered the client, and ��sMARor computer nsinvolvestheappliemergency situation. An IVP can be introduced directlydrug may be irritating to the lining of the blood vessels.Figure 15.1 Some controlled substances are kept in speciallydesigned packages or plastic containers that are sectioned andnumbered. Pharmacy-preparedcationpermittedof nursing knowledgeand critical telephonethinking. Check thestate’sto acceptandverbalorders. It ismedication-infused bag with correct label Short secondary administration setnurse practice act to verify the scope of practice for the LPN/LVN wabssolid Antisepticfor disinfection of needleless connector orit relatesto IV medicationadministration. Agencyalso mustinjection portbe checkedand followed.skill is notto eeliminateerrorsoccur Needleless adapter, syringe, and saline if medication ishowever, can inform the AP of the intended therapeutic effects andringfromof verbalorders.Forall verbalwithorthe primary infusionspecificside effectsthe medicationand directthe example,AP to report for incompatiblespecificclient observationsto the nursefollow-up.must first write down thetelephoneordersthefornurseM17 BERM1444 09 SE C17.indd 45019/09/19 7:00 PMorder and then read it back, verbatim, to the prescribingIMPLEMENTATIONof the solution to exit the tubing to ensure that the clientcare provider.Included on the inventory record are the controlled Preparationreceives the full dose of medication. Check the MAR. Clamp the secondary tubing.substances wasted during preparation. When a portion or Check the label on the medication carefully against the Attach the appropriate label to the secondary surethatthecorrectmedicationisbeingall of a controlled substance dose is discarded, the nurseNote: Per the Infusion Nurses’ Society (2016), all primaryprepared.SafetyGoalsand identifyotherand secondary administration sets used for intermittentmust askPatienta secondnurseto witnessthe discardingof the Confirm that the dosage is correct.administration should be replaced every 24 hours. Ensure medication compatibility with the primary infusionc rucialsafetyinformation.unused medication. Both nurses must sign the control Encourage the prescribing care provider to providecor- up subsequent medication bags whenWhen settingsolution.primaryand secondary fluids are compatible: Consulta pharmacist,to confirmcompatibilityof the as “B as in boy.”inventory form.rectspellingif required,of a drug,usingaids suchIt Use the back priming method for administering the nextdrugs and solutions being mixed.In most agencies, counts of controlled substances Organizemedicationis alsoimportant for the provider to pronounce numbers dose with the same administration set.the equipment.Lower the previous medication infusion bag below thethe medicationForbag example,from the refrigerator30 minutes 16 should beare taken at the end of each shift. The count total should Removeseparately.the numberstatedprimary IV bag.before administration, if appropriate.match the total at the end of the last shift minus the num- PerformanceOpen the clamp of the medication bag.as “one six” to avoid confusion with the number 60. Allow the solution from the primary IV bag to backfillber used. If the totals do not match and the discrepancy 1. Perform hand hygiene and observe other appropriate infectionthe secondary IV tubing and one-third to one-half of thesecondary tubing chamber. ❶ Rationale: This methodcannot be resolved, it must be reported immediately to prevention procedures.2. Provide for client privacy.of priming the secondary tubing allows for no loss ofthe nurse manager, nursing supervisor, and pharmacy 3. Prepare the client.medication.Policiesabout primary care providers’ ordersvaryto performing the procedure, introduce yourself Detach the empty container and insert spike into theaccording to agency policy. In facilities that use a com- ocol.considerably from agency to agency. For example,a cli- bag.new medicationputerized dispensing system, manual counts are notRationale: This ensures that the right client receives the Clamp the secondary IV tubing.ent’smedication.orders may be automatically canceled aftersurgeryrequired because the dispensing system runs a continu- essmentor an examination involving an anesthetic Clinicalagent. ThepriAlertmeasures necessary for the medication.ous count; however, discrepancies must still be reportedmaryprovidermustwrite4. Explainthe carepurposeof the medicationandthenhow it willhelp, new orders.EachIVmedicationbag requires its own secondary tubing. Mediand accounted for.using languagethe client canalsounderstand.MostthatagencieshaveIncludelists of abbreviationscation from the IVoffiinfusion bag remains in the secondary tubing. Itrelevant information about the effects of the medication.is important, therefore, when hanging subsequent IV infusion bagscially Informationaccepteduseacceptancein the agency.To preventmedicaRationale:canforfacilitateof andto hang the same medication on the same secondary tubing. Thisadherence to the therapy.A01 BERM1444 09 SE FM.indd 819/11/2019 18:56avoidstheagenciesmixing of incompatible hat5. Assemble the secondary piggyback infusion:Safety Alert!viiiSAFETY
ne and272Unit 3 Assisting with Client Hygiene and ComfortManaging Pain with a PCA IV Pump—continued260SKILL 9.2EVALUATIONPRACTICE GUIDELIN ES provide Conduct appropriate follow-up: Painstatusinstantaccesssummaries Respiratory rate and characterof commonpmedicationrocedures Amount of used and Frequency of useclinicalpractice.Unit 3 Assisting with Client Hygiene and ComfortCompare to previous findings, if available.Report significant deviations from normal to the primary carePRACTICEprovider.GUIDELINES Strategies for Colleague Accountability in Pain ManagementWhat do we do if the healthcare team does not respond positivelyto a client’s report of pain?Cite recommendations from evidence-based clinical practiceguidelines (e.g., American Pain Society, Agency for HealthCare Policy and Research), The Joint Commission standards, Speak up! Inappropriate professional behavior will persist if notorganization-specific documents (e.g., mission statement,challenged. If necessary, file an “incident” or “variance” report forpatient bill of rights, practice standards), or relevant researchpersistent patterns or unacceptable violations of standards ofand quality reports. As necessary, distribute or post with keyLIFESPAN CONSIDERATIONS PCA Pumpcare. These types of behaviors (ignoring reports of pain, failing topassages highlighted.treat or mistreating people with pain) are not only unethical, but Involve key committees, managers, and administrators inADULTSCHILDRENlegallyOLDERindefensiblebecause a standard of care is not being met.studying and addressing the problem from a cost, quality, Include the parents in teaching.Carefullymonitoroffordrugside effects. Clarify thatthe sensationpainis subjectiveand that profescompetency, and credentialing perspective. Assess the child’s ability to understand and use the client Use cautiously for individuals with impaired pulmonary or renalsionals havea duty to believe clients’ reports of their symptoms.control button. Pasero and McCaffery (2011) report that “PCAfunction. Assess the client’s cognitive and physical ability to use the clienthas been used effectively and safely in developmentally normalchildren as young as 4 years old” (p. 314).control button. Use distraction techniques to avoid dislodging or disconnectionby the child. Use pediatric elbow immobilizers (no-nos, Snuggle Wraps) ifdistraction is not effective in keeping the child from playing withReducing a client’s misconceptions about pain and itsA preventive approach to pain management involves thetubing and ports.Reducing Misconceptions About Pain Preventing Paine painvel, and cognitiveain intensity scalesmining the client’ssistency for nursesand children) andSKILL 9.2treatment will remove one of the barriers to optimal painprovision of measures to treat the pain before it occursrelief. The nurse should explain to the client that pain isor before itC becomesL I ENT Tsevere.EACH IPreemptiveN G CO N SIanalgesiaD E R ATIisO se ora highly individual experience and that the client is thegiveoftipsand toolshelp toclientsCLIENT TEACHING CONSIDERATIONSrelieve pain after surgery and reduce the need for opioidonly one who really experiences the pain, although othersfacilitate self-care and wellness.can untpain control.(i.e., pushbutton) 5 to 10times to receive thesameClient Self-Management of Painof medication(10 mgmorphinereceiveSome authors, however, believe the term “preventive”dealtthe nurseandclientequivalent)discuss theythe wouldcontextChoose a time to teach the client about pain management whenthe with whenin a standard “shot.”pain is controlled so that the client is able to focus on the teaching.analgesia better explains the assumption of the practice—of pain controlas part of the healing process. For exam Describe the use of the pain scale and encourage the client toTeaching the client about self-management of pain can includethat the only way to prevent central sensitization mightple, clients mayrefusepainmedicineunderstanding.out of concern forrespondin orderto demonstratethe foll
evolved and matured just as has the book itself. Also, like the book, Jordanna seeks to—and will—make the world a healthier and better place. Shirlee again dedicates this book to her husband, Terry J. Schnitter, for his continual love and support; to the nurses