Transcription
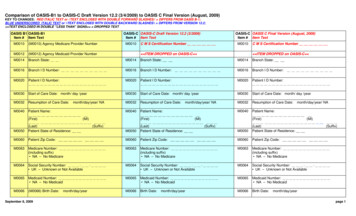
DRAFTMINIMUM DATA SET, Version 3.0 (MDS 3.0)FOR NURSING HOME RESIDENTASSESSMENT AND CARE SCREENING(Note: This MDS 3.0 Draft contains only the new/revised items that arebeing tested in the field trial. Some retained administrative items are notincluded in the study form in order to protect resident privacy.)DRAFT VERSION - 7/31/2006
INTRODUCTION: THE MDS 3.0 EVALUATION STUDYINTRODUCTION TO THE MDS 3.0This revision of the Minimum Data Set for Nursing Homes (MDS 3.0) builds on lessonslearned from using and testing the MDS 2.0. Like MDS 2.0, it focuses on clinical assessment ofnursing home residents to screen for common, often unrecognized or unevaluated, conditions andsyndromes. Revisions have been based on feedback from MDS users, resident advocates andfamilies, input from subject-area experts, and new knowledge and evidence about residentassessment. MDS 3.0 aims to increase the accuracy of assessments, obtain information directlyfrom residents, include assessment items used in other care-settings, and move items towardfuture electronic health record formats.ASSESSMENTS BASED ON INTERVIEW: GIVING RESIDENTS VOICEPerhaps the most significantadvance in this revision is the useof direct interview items toconsistently elicit resident voice.Respect for the individual residentis fundamental to high qualitycare and resident quality of life.One of the most direct ways ofconveying this respect is todirectly ask the resident abouthow he/she feels and about his orher preferences. General,unfocused questions often fail toconvey a real desire to hear howsomeone really feels and areunlikely to elicit meaningfulreport of symptoms orpreferences. Residents andfamilies want to be asked specificand direct questions. They cometo us for care and want that care tobe based on what they want andon improving how they feel.Equally as important, the mostaccurate way to assess manytopics is to directly ask theresident. For areas such ascognition, mood, preferences, andpain, studies have repeatedlyshown that staff or familyimpressions often fail to capturethe resident’s (or any adult’s) realcondition or preferences.Unfortunately, staff and familyobservations of mood and painsignificantly underestimate thepresence of these treatableconditions. This is true acrosssettings and in both short andlong stay residents. If we don’task the difficult questions, werisk leaving the resident to sufferin silence or to be incorrectlyevaluated.Resident interview is feasible.Experience and a large body ofresearch have shown that evenresidents with moderate cognitiveimpairment can accurately andreliably answer simple interviewquestions about how they feel andabout what they want. This isalso true for some residents withsignificant cognitive impairment.Surprisingly, going to theresident is often more efficient.Using the resident as the primaryinformation source is not onlytime well spent, it can actually befaster. Many MDS 2.0 sectionsdirect the assessor to talk to theresident, talk to the family, talk tostaff across all shifts and reviewthe record. Although the residentis mentioned as a data source, sheor he is only one in a long list.However, documentation of pain,mood, and preferences is oftenmissing or inaccurate in themedical record and the workloadin facilities can make observingsubtle signs and symptomschallenging. For cognitiveassessment, mood, preferencesand pain a simple residentinterview that uses standardizeditems can be the sole informationsource, providing more accurateinformation directly andefficiently. These items are nowdirectly on the MDS 3.0.Responses can be entered andthe item is complete. Accessingmultiple data sources is onlynecessary for those residentswho, despite being approached,cannot participate in answeringthe particular item.As in other aspects of clinicalmedicine, interview items havebeen tested to identify those thatwork better for measuring thetopic in question. The itemwording and response optionsincluded here have been testedand shown to work in nursinghome and other frail populations.Clinicians in other settingsalready use many of these. Theinclusion of structured interviewitems ensures that the MDSitems are using a commonmeasuring stick, are more likelyto be reliable across facilities andprovide a common language forcommunication across settings.Continued on next page i
INTRODUCTION: THE MDS 3.0 EVALUATION STUDYASSESSMENTS BASED ON INTERVIEW: GIVING RESIDENTS VOICEThese items contribute to, butdo not replace, day-to-dayinteractions.Testing has includedconsideration of “simpler”yes/no formats for these items.If the item asks about somethingthat isn’t fixed or absolute, thenhaving more than two responsechoices can make respondingeasier for older adults. Manyadults who struggle withreducing their experience toyes/no will have a much easiertime when allowed to selectfrom a range of choices thatreflect the variations theyactually experience day to day.The response choices have beencarefully selected and tested toThus, these interview itemsconvey our respect for the residentas a care participant, openimportant clinical conversationswith our residents, increase theSome might worry that these type accuracy of our assessments,improve the quality of the care weof items dictate to residents andprovide and bring nursing homestaff about the content of theirinteractions. Users of structured care inline with care in othersettings. Most of us talk to ourinterviews such as theseresidents every day. We believeconsistently report that thethat we touch on these importantopposite occurs. Structuredtopics and provide amplequestions often bring upopportunity for residents toimportant issues for the residentand open up discussion between express what they feel. Theseitems ensure that we use part ofthe resident and provider. Theythose conversations to effectivelyhelp create an ongoing dialoguebetween the resident and provider and reliably screen for theseimportant preferences andwithin which it is safe to trulyconditions.report on symptoms and careneeds.allow this choice while matchingthe responses to the questionbeing asked. Both make the taskof responding easier.IMPROVEMENTS IN ACCURACYMDS 3.0 includes changes thatseek to improve the accuracy ofassessments. For many sectionsand items, we have includeditems identified by contentexperts and research as morevalid measures of the condition.Items have been revised basedon experience of users and inputfrom subject matter experts whoare familiar with nursing homeresidents and nursing homecare. In addition, MDS 3.0includes modified responseoptions or instructions that aimto increase clarity and thereforeagreement across assessors. Forexample, some items combineresponse categories wheredifferentiation had been difficultin the past. Instructions fordiagnoses have been revised toinclude detailed algorithms inorder to assist in defining activedisease. Whenever possible, wehave included items or languageused in other health care settingsin order to improvecommunication across settingsand providers. For example,items included in the NationalPressure Ulcer Advisory Panel’sPUSH tool are used to describepressure ulcers; new ADL itemsseparate toilet transfer fromtoileting and upper body dressingfrom lower body dressing. Thenew delirium section is a set ofitems that have been validated forfrail older adults in hospitalsettings and is based onobservations made duringstructured cognitive assessment.Language has been revised toreflect the standards applied inother settings.IMPROVEMENTS IN EFFICIENCYMany of the changes outlinedabove will increase theefficiency of completing theMDS by yielding higher qualityinformation for the timeinvested. MDS 3.0 includesother changes that will alsoincrease efficiency. Thequestions aim for greaterconsistency in look backwindows and test a shorter lookback than was used in priorversions. To the extent possible,items that did not addressscreening for clinical symptomsand syndromes were eliminated.We have, however, retained itemsthat currently form the basis forpayment and qualitymeasurement.ii
SectionASelect Demographic ItemsA1. Assessment Reference Date (last day of MDS observation period)/M MA2. GenderEnter1. MaleCodeD D/1017/Y Y Y Y18/2. FemaleA3. LanguageEnterDoes the resident need or want an interpreter to communicate with a doctor or health care staff?0. NoCode1. Yes Î If yes, specify primary language:9. Unable to determineA4. EthnicityÐ Complete only on admission assessment ÐEnterIs the resident of Hispanic or Latino origin or descent?0. NoCode1. Yes9. Unable to determineA5. RaceÐ Complete only on admission assessment Ða.American Indian or Alaska Nativeb. Asianc.Black or African Americand. Native Hawaiian or Other Pacific Islandere.Whitef.Otherg. Unable to determineA6. Mental Health HistoryÐ Complete only on admission assessment ÐEnterThe resident has been evaluated by Level II PASRR, and determined to have a serious mental illness and/or mentalretardation.Code0. No1. Yes9. Not applicable (Unit not Medicaid certified)2031/32/33/34/Check all that apply.MDS 3.0 Evaluation Study Test Items19/35/36/37/38/39/40/Page 1
SectionBHearing, Speech, and VisionB1. ComatoseEnterPersistent vegetative state/no discernible consciousness last 5 days.0. NoCode1. Yes Î If yes, skip to section G, Functional Status.B2. HearingEnterAbility to hear (with hearing aid or hearing appliance if normally used) last 5 days.0. Adequate—no difficulty in normal conversation, social interaction, listening to TVCode1. Minimal difficulty—difficulty in some environments (e.g. when person speaks softly or setting is noisy)2. Moderate difficulty—speaker has to increase volume and speak distinctly3. Highly impaired—absence of useful hearingB3. Hearing AidEnterHearing aid or other hearing appliance used in above 5-day assessment.0. NoCode1. YesB4. Speech ClarityEnterSelect best description of speech pattern in last 5 days.0. Clear speech—distinct intelligible wordsCode1. Unclear speech—slurred, mumbled words2. No speech—absence of spoken wordB5. Makes Self UnderstoodEnterAbility to express ideas and wants, consider both verbal and non-verbal expression in last 5 days.0. Understood—clear comprehensionCode1. Usually understood—difficulty communicating some words or finishing thoughts but if given time or someprompting is able2. Sometimes understood—ability is limited to making concrete requests3. Rarely/never understoodB6. Ability to Understand OthersEnterUnderstanding verbal content, however able (with hearing aid or device if used) in last 5 days.0. Understands—clear comprehensionCode1. Usually understands—misses some part/intent of message BUT comprehends most conversation2. Sometime understands—responds adequately to simple, direct communication only3. Rarely/never understandsB7. VisionEnterAbility to see in adequate light (with glasses or other visual appliances) in last 5 days.0. Adequate—sees fine detail, including regular print in newspapers/booksCode1. Impaired—sees large print, but not regular print in newspapers/books2. Moderately impaired—limited vision; not able to see newspaper headlines but can identify objects3. Highly impaired—object identification in question, but eyes appear to follow objects4. Severely impaired—no vision or sees only light, colors or shapes; eyes do not appear to follow objectB8. Corrective LensesEnterCorrective lenses (contacts, glasses, or magnifying glass) used in above 5-day assessment.0. NoCode1. YesMDS 3.0 Evaluation Study Test Items41/42/43/44/45/46/47/48/Page 2
SectionCCognitive PatternsBrief Interview for Mental Status (BIMS)C1. Interview AttemptedEnter0. No (resident is rarely/never understood or needed interpreter not present) Î Skip to C8, Staff Assessment forMental StatusCode1. YesC2. Repetition of Three WordsC4. RecallAsk resident: “I am going to say three words for you toAsk resident: “Let’s go back to the first question. Whatremember. Please repeat the words after I have said allwere those three words that I asked you to repeat?”If unable to remember a word, give cue (somethingthree. The words are: sock, blue, and bed. Now tell methe three words.”to wear; a color; a piece of furniture) for that word.EnterCodeNumber of words repeated after first attempt0. None1. One2. Two3. ThreeAfter the resident’s first attempt, repeat the wordsusing cues (“sock, something to wear; blue, a color;bed, a piece of furniture”).You may repeat the wordsup to two more times.C3. Temporal Orientation (orientation to year, month,and day)EnterAsk resident: “Please tell me what year it is right now.”a.Able to report correct yearCode3. CorrectEnter2. Missed by 1 year1. Missed by 2–5 years0. Missed by 5 years or no answerAsk resident: “What month are we in right 1/Able to recall “sock”2. Yes, no cue required1. Yes, after cueing (“something to wear”)0. No—could not recallAble to recall “blue”2. Yes, no cue required1. Yes, after cueing (“a color”)0. No—could not recallAble to recall “bed”2. Yes, no cue required1. Yes, after cueing (“a piece of furniture”)0. No—could not recallEnter Numbers54/55/56/5758/C5. Summary ScoreAdd scores for questions C2–C4 and fill intotal score (00–15).Enter 99 if unable to complete interview52/b.CodeAble to report correct month2. Accurate within 5 days1. Missed by 6 days to 1 month0. Missed by 1 month or no answerAsk resident: “What day of the week is today?”c.Able to report correct day of the week1. Correct0. Incorrect or no answer50/49/53/C6. Organized ThinkingEntera.Ask resident: “Are there fish in the ocean?”1. Correct (“yes”)Code0. Incorrect or no answerEnterb. Ask resident: “Does one pound weigh morethan two pounds?”Code1. Correct (“no”)0. Incorrect or no answerEnterc.Ask resident: “Can a hammer be used topound a nail?”Code1. Correct (“yes”)0. Incorrect or no answer60/61/62/C7. Skip Item: Interview CompletedEnter0. No (resident was unable to complete interview) Î Continue to C8, Staff Assessment for Mental Status1. Yes Î Skip to C12, Signs and Symptoms of DeliriumCodeMDS 3.0 Evaluation Study Test Items59/Page 3
SectionCCognitive PatternsStaff Assessment for Mental Status—Complete only if resident interview (C2–C6) not completed63/C8. Short Term Memory OKEnterSeems or appears to recall after 5 minutes.0. Memory OKCode1. Memory problemC9. Long Term Memory OKEnterSeems or appears to recall long past.0. Memory OKCode1. Memory problemC10. Memory/Recall AbilityCheck all that the resident was normally able to recall during the last 5 days:a. Current seasonb. Location of own roomc. Staff names and facesd. That he or she is in a nursing homee. None of the above is recalledC11. Cognitive Skills for Daily Decision MakingEnterMakes decisions regarding tasks of daily life.0. Independent—decisions consistent/reasonableCode1. Modified independent—some difficulty in new situations only2. Moderately impaired—decisions poor; cues/supervision required3. Severely impaired—never/rarely made decisions64/Check all that apply.65/66/67/68/69/70/DeliriumC12. Signs and Symptoms of Delirium (from CAM)After interviewing the resident, code the following behaviors (a–d) in last 5 days.Entera.Inattention—Did the resident have difficulty focusing attention(easily distracted, out of touch or difficulty keeping track of whatwas said)?CodeCoding:0. Behavior not present1. Behavior continuously present,does not fluctuate2. Behavior present, fluctuates (comesand goes, changes in severity)Ð Enter Codes in BoxesÐEnterb.CodeEnterc.CodeDisorganized thinking—Was the resident’s thinkingdisorganized or incoherent (rambling or irrelevant conversation,unclear or illogical flow of ideas, or unpredictable switchingfrom subject to subject)?Altered level of consciousness—Did the resident have altered72/73/level of consciousness? (e.g., vigilant—startles easily to anysound or touch; lethargic—repeatedly dozes off when beingasked questions, but responds to voice or touch; stuporous—very difficult to arouse and keep aroused for the interview;CodeEnter71/d.comatose—cannot be aroused)Psychomotor retardation—Did the resident have an unusually74/decreased level of activity such as sluggishness, staring intospace, staying in one position, moving very slowly?75/C13. Acute Onset Mental Status ChangeEnterIs there evidence of an acute change in mental status from the resident’s baseline in last 5 days?1. YesCode0. NoMDS 3.0 Evaluation Study Test ItemsPage 4
SectionDMoodSelf-Rated Mood Interview—Complete D1–D4 for all residents who are capable of any communication (B5 0, 1, or 2), and forwhom an interpreter is present or not required.D1. Interview AttemptedEnter0. No (resident is rarely/never understood or needed interpreter not present) Î Skip to D6, Staff Assessment1. Yes10/CodeD2. Interview (From PHQ-9)I. Symptom PresenceIf yes, obtain frequency.Say to resident: “Over the last 2 weeks, have youbeen bothered by any of the following problems?”II. Symptom FrequencyCircle one response0.1.0–12–6daydays(Not at all)a.Little interest or pleasure in doing thingsEnterCodeb.Feeling down, depressed, or hopelessEnterCodec.Trouble falling or staying asleep, orsleeping too muchEnterCoded.Feeling tired or having little energyEnterCodee.EnterPoor appetite or overeatingCodef.g.h.i.Feeling bad about yourself—or that youare a failure or have let yourself or yourfamily downTrouble concentrating on things, such asreading the newspaper or watchingtelevisionMoving or speaking so slowly that otherpeople could have noticed. Or the oppositebeing so fidgety or restless that you havebeen moving around a lot more than usualThoughts that you would be better offdead, or of hurting yourself in some way1) If i “Yes”, check here to indicatethat the charge nurse has been .0.1.9.0.1.9.0.1.9.0.1.9.0.1.9.0.1.9.0.1.9.NoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo response0.1.9.NoYes ÎNo e than halfthe days)(Nearlyevery 320/21/012322/23/012324/25/012326/27/012328/29/D3. Total Severity ScoreEnter NumbersSum of all circled frequency responses (D2–II; items a–i). Score may be between 00 and 27. Enter 99 if unableto complete interview (3 or more items in column I marked “No response”)Check here if some or all frequency responses (D2–II; items a–i) are missing from total score.MDS 3.0 Evaluation Study Test ItemsPage 53031/32/
SectionDMoodD4. Evidence of DepressionEnterAre 2 or more frequency items in shaded columns circled (D2–II, a–i), and at least one of these is question a or b?0. NoCode1. Yes33/D5. Skip Item: Resident Interview CompletedEnter0. No (3 or more items in D2–I, items a–i marked “No response”) Î Continue to D6, Staff Assessment of Depression1. Yes Î Skip to Section E, Behavior34/CodeStaff Assessment of Mood—Complete D6–D8 only if resident interview (D1–D5) not completed. (From PHQ-9)D6. Staff AssessmentI. Symptom PresenceII. Symptom FrequencyIf yes, obtain frequency.Circle one responseSay to staff: “Over the last 2 weeks, did the resident0.1.2.have any of the following problems?”0–12–67–11daydaysdays(Not at all)a.Little interest or pleasure in doing thingsEnterCodeb.Feeling down, depressed, or hopelessEnterCodec.Trouble falling or staying asleep, orsleeping too muchEnterCoded.Feeling tired or having little energyEnterCodee.EnterPoor appetite or overeatingCodef.g.h.i.j.Feeling bad about themselves—or that heor she is a failure or has let themselves ortheir family downEnterTrouble concentrating on things, such asreading the newspaper or watchingtelevisionEnterMoving or speaking so slowly that otherpeople could have noticed. Or the oppositebeing so fidgety or restless that you havebeen moving around a lot more than usualThoughts that they would be better offdead, or of hurting themselves in some wayEnter1) If i “Yes”, check here to indicate that thecharge nurse has been informed:Feeling short-tempered, easily 9.0.1.9.0.1.9.0.1.9.0.1.9.NoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo responseNoYes ÎNo response0.1.9.NoYes ÎNo response(Severaldays)(More than halfthe days)3.12–14days(Nearlyevery erCode0.1.9.NoYes ÎNo response54/0MDS 3.0 Evaluation Study Test Items123Page 655/
SectionDMoodD7. Total Severity ScoreSum of all circled frequency responses (D6–II, a–i; do not include D6j). Score may be between 00 and 27.Check here if staff responses are based on observation for less than 14 days.D8. Evidence of DepressionEnterAre 2 or more frequency items in shaded columns circled (D6–II, a–i), and at least one of these is question a or b?0. NoCode1. YesEnter NumbersMDS 3.0 Evaluation Study Test ItemsPage 75657/58/59/
SectionEBehaviorCheck all that apply.E1. PsychosisCheck if problem condition was present at any time in last 5 days:a. Hallucinations (perceptual experiences in the absence of real external sensory stimuli) or Illusions (misperceptionsin the presence of real external sensory stimuli)b. Delusions (misconceptions or beliefs that are firmly held, contrary to reality)c. None of the above60/61/62/Behavioral SymptomsÐE2. Behavioral Symptom—Presence & FrequencyNote presence of symptoms and their frequency in the last 5 days:Entera. Physical behavioral symptoms directed toward others (e.g.,Coding:0. Not present in last 5 days1. Present 1–2 days2. Present 3 or more daysÐ Enter Codes in BoxesCodeEnterhitting, kicking, pushing, scratching, grabbing, abusing otherssexually)b. Verbal behavioral symptoms directed toward others (e.g.,threatening, screaming at others; cursing at others)63/64/CodeEnterCodec.Other behavioral symptoms not directed toward others (e.g.,65/physical symptoms such as the resident hitting or scratchingSelf, pacing, rummaging, public sexual acts, disrobing in public,and throwing or smearing food or bodily wastes, or verbal/vocalsymptoms like screaming, disruptive sounds)66/E3. Overall Presence of Behavioral Symptoms in the last 5 daysEnterWere any behavioral symptoms in questions E2 coded 1 or 2?0. No Î Skip to E6, Rejection of CareCode1. Yes Î Considering all of the symptoms together, answer E4 and E5 belowE4. Impact on ResidentDid any of the identified symptom(s):Entera.Put the resident at significant risk for physical illness or injury?0. NoCode1. YesEnterb. Significantly interfere with the resident’s care?0. NoCode1. YesEnterc.Significantly interfere with the resident’s participation in activities or social interactions?0. NoCode1. YesMDS 3.0 Evaluation Study Test Items67/68/69/Page 8
SectionEBehaviorE5. Impact on OthersDid any of the identified symptom(s):Entera.Put others at clinically significant risk for physical injury?0. NoCode1. YesEnterb. Significantly intrude on the privacy or activity of others?0. NoCode1. YesEnterc.Significantly disrupt care or living environment?0. NoCode1. Yes70/71/72/E6. Rejection of Care—PresenceEnterIn the last 5 days, did the resident reject evaluation or care (e.g., bloodwork, taking medications, ADL assistance)that is necessary to achieve the resident’s goals for health and well-being? Do not include behaviors that have alreadyCodebeen addressed (e.g., by discussion or care planning with the resident or family), and/or determined to be consistentwith resident values, preferences, or goals.0. No Î Skip to E8, Wandering1. Yes73/E7. Rejection of Care—FrequencyEnterNumber of days on which care was rejected1. 1–2 daysCode2. 3 or more days74/Wandering75/E8. Wandering—PresenceEnterIn the last 5 days, has the resident wandered on at least one occasion?0. No Î Skip to E11, Change in Behavioral SymptomsCode1. YesE9. Wandering—ImpactEntera.Does the wandering place the resident at significant risk of getting to a place having greater risk of danger(e.g., stairs, outside of the facility)?Code0. No1. YesEnterb. Does the wandering significantly intrude on the privacy or activities of others?0. NoCode1. Yes76/77/E10. Wandering—FrequencyEnterOf the last 5 days, on how many days has wandering occurred?1. 1–2 daysCode2. 3 or more days78/E11. Change in Behavioral or Other Symptoms—Consider all of the symptoms assessed in items E1 through E10.Ð Complete only on follow-up assessmentÐEnterHow does resident’s current behavior status, care rejection, or wandering compare to last assessment?0. SameCode1. Improved2. Worse79/MDS 3.0 Evaluation Study Test ItemsPage 9
SectionFPreferences for Customary Routine,Activities, Community SettingF1. Preferred RoutineAll residents should be asked about preferences. Complete F1 for all residents who are capable of any communication (B5 is coded0, 1, or 2), and for whom an interpreter is present or not required. For residents who are not able to communicate, interview familymember, or significant other who knows the resident and can provide information on past customs and preferences.Preface a–h by saying to resident: “While you are in the nursing home ”10/Entera.How important is it to you to choose what clothes to wear?Code11/EnterCodeb. How important is it to you to take care of your personalbelongings or things?12/EnterCoding:1. Very important2. Somewhat important3. Not very important4. Not important at all5. Important, but can’t do or no choice9. No response or non-responsiveÐ Enter Codes in BoxesÐc.CodeHow important is it to you to choose between a tub bath, shower,bed bath, or sponge bath?13/Enterd. How important is it to you to have snacks available betweenmeals?Code14/Entere.If you could go to bed whenever you wanted, how important would itbe to you to stay up past 8:00 p.m.?f.How important is it to you to have your family or a close friendinvolved in discussions about your care?Code15/EnterCode16/Enterg. How important is it to you to be able to use the phone in private?Code17/EnterCodeh. How important is it to you to have a place to lock your things tokeep them safe?18/F2. Primary RespondentIndicate primary respondent for F1, Preferred Routine:Enter1. Resident2. Significant Other (family, close friend, or other representative)Code9. Could not be completed by resident or significant otherMDS 3.0 Evaluation Study Test ItemsPage 10
SectionFPreferences for Customary Routine,Activities, Community SettingF3. Activity Pursuit PatternsAll residents who are able to communicate should be asked about activity pursuit patterns—even if they have not been able tocomplete F1. Complete F3 for all residents who are capable of any communication (B5 is coded 0, 1, or 2), and for whom aninterpreter is present or not required. For residents who are not able to communicate, interview family, or significant otherwho knows the resident and can provide information on past customs and preferences.Preface a–j by saying to resident: “While you are in the nursing home ”19/Entera.CodeHow important is it to you to have books, newspapers, andmagazines to read?20/Enterb.How important is it to you to listen to music you like?Code21/Enterc.How important is it to you to be around animals such as pets?Coding:1. Very important2. Somewhat important3. Not very important4. Not important at all5. Important, but can’t do or no choice9. No response or non-responsiveÐ Enter Codes in BoxesÐCode22/Enterd.How important is it to you to keep up with the news?Code23/Entere.How important is it to you to do things with groups of people?Code24/Enterf.How important is it to you to do your favorite activities?Code25/Enterg.How important is it to you to do things away from the nursinghome?h.How important is it to you to go outside to get fresh air when theweather is good?Code26/EnterCodeEnter27/i.How important is it to you to participate in religious services orpractices?CodeEnter28/j.If your doctor approves, would you like to be offered alcohol on occasion at meals or social events?0. NoCode1. Yes5. Yes, but can’t do or no choice9. No response or non-responsive answerF4. Primary RespondentIndicate primary respondent for F3, Activity Pursuit Patterns:Enter1. Resident2. Significant Other (family, close friend, or other representative)Code9. Could not be completed by resident or significant otherMDS 3.0 Evaluation Study Test Items29/Page 11
SectionFPreferences for Customary Routine,Activities, Community SettingF5. Return to CommunityÐ Complete only on admission assessment ÐAsk resident (or family or significant other if resident unable to respond):Enter“Do you want to talk to someone about the possibility of returning to the community?”0. NoCode1. Yes30/F6. Skip Item: Staff Assessment RequiredEnterWas either F2, Preferred Routine Respondent, or F4, Activity Respondent coded 9?0. No Î Skip to Section G, Functional StatusCode1. Yes Î Complete F7, Staff Assessment of Activity and Daily Preferences31/Check all that apply.Check all that apply.F7. Staff Assessment of Activity and Daily Preferences—Complete only if unable to interview resident or other representativefor either F1, Preferred Routine, or F3, Activity Pursuit Patterns.Resident Prefers:32/k. Place to lock personal belongingsa.Choosing clothes to wear33/l.Reading books, newspapers, or magazinesb. Caring for personal belongings34/m. Listening to musicc.Receiving tub bath35/n. Being around animals such as petsd. Receiving shower36/o. Keeping up with the newse.Receiving bed bath37/p. Doing things with groups of peoplef.Receiving sponge bath38/q. Participating in favorite activitiesg. Snacks between meals39/r.Spending time away from the nursing homeh. Staying up past 8:00 p.m.40/s.Spending time outdoorsi.Family or close friendt.Participating in religious activities or practicesinvolvement in care discussions41/u. None of the abovej.Use of phone in privateMDS 3.0 Evaluation Study Test ItemsPage 1242/43/44/45/46/47/48/49/50/51/52/
Sec
Adequate—sees fine detail, including regular print in newspapers/books Enter Code 1.Impaired—sees large print, but not regular print in newspapers/books 2. Moderately impaired—limited vision; not able to see newspaper headlines but can identify objects 3. Highly impaired—object identification in question, but eyes appear to follow .