Transcription
OCDAn OCD-UK information guide for people affected byObsessive-Compulsive DisorderOCD-UK is the leading national charity, independently working with and forchildren and adults affected by Obsessive Compulsive Disorder (OCD)
You’re not aloneAround 1.2% of the population are thought to beaffected by Obsessive-Compulsive Disorder (OCD) andit is actually listed amongst the top 10 most debilitatingillnesses by the World Health Organisation in terms of lossof income and decreased quality of life.And the chances are you’re reading this booklet becauseyou are amongst that 1.2% and because at some time oranother you have felt upset, scared, and alone. But restassured, there is hope, OCD can be treated successfullyand beyond the illness there is a life full of opportunities toexperience.OCD-UK is unique in the respect that it is a service userled charity for people affected by OCD. Whatsmore it isrun by people that have experienced OCD first hand, andwho can help and inspire you towards the ultimate goal ofrecovery.The most important way they do this is by providing youwith knowledge. Because, as many ex-sufferers will tellyou, with OCD knowledge comes power. With powercomes the strength to overcome the illness once and for all.It is hoped that this guide will be just the starting point inclarifying some of the details about OCD, in terms of itssymptoms and possible treatments, and that it will offeryou hope and encouragement to embark on your ownpersonal road to recovery.ContentsAbout OCD-UK .OCD - An Introduction .Obsessions - An explanation .Compulsions - An explanation .OCD spectrum disorders .Understanding OCD .Treatments .Cognitive Behaviour Therapy (CBT) .Medications .What causes OCD? .2OCD-UK34567810121416The many faces of OCD . 18Family, Friends and Carers (FFC) . 22OCD-UK would like to thank two of ourvolunteers, Alison and Leigh for theircontributions towards compiling thisinformation guide. We remain grateful forthe kind support and commitment of them,and all of our fantastic volunteers.OCD INFORMATION GUIDE
AboutRegistered Charity Number: 1103210OCD-UK is the leading national charity,independently working with and for childrenand adults affected by Obsessive-CompulsiveDisorder (OCD).It is our belief that everyone affected bythis illness should receive care, support andtreatment of the very highest quality.By working with sufferers, their families,health professionals and researchers, we aimto develop and share our experiences andknowledge to help people gain a betterunderstanding of Obsessive-CompulsiveDisorder and to ultimately help reduce theeffect it has on people’s lives.We do this by providing accessible andeffective support services, and by campaigningfor improved access to quality treatment andcare.We also facilitate a safe environment forsufferers to communicate with each other andprovide mutual understanding and support.How can you help make a positivedifference to sufferers’ lives?Perhaps by making a one-off donation (everypenny really does make a difference), orby becoming a member of OCD-UK, orparticipating in a fundraising event, which willhelp us achieve our goals and make a realdifference to the lives of people affected.Find out about more about OCDFor more detailed information about ObsessiveCompulsive Disorder and details of how youcan get involved and help OCD-UK, pleasevisit our website at www.ocduk.org
Obsessive -Compulsive Disorder - An introductionObsessive–Compulsive Disorder (OCD) is aserious anxiety-related condition where aperson experiences frequent, intrusive andunwelcome obsessive thoughts, often followedby repetitive compulsions, impulses or urges.OCD presents itself in many guises, and peopleare often surprised to learn that it goes farbeyond the common perception of excessivehand washing or the repetitive checking of lightswitches. We hope this information guide willoffer you a better insight into what OCD is,and the different ways in which it can manifestitself.Who does it affect?It may surprise you to know that ObsessiveCompulsive Disorder affects as many as 12 inevery 1000 people (1.2% of the population)from young children to adults, regardless ofgender or social or cultural background. Basedon current estimates for the UK population,there are potentially around 741,504 peopleliving with OCD at any one time.Furthermore, the illness can be so debilitatingand disabling that the World HealthOrganisation (WHO) has ranked OCD in thetop ten of the most disabling illnesses of anykind, in terms of lost earnings and diminishedquality of life.Equally as disturbing is the fact that sufferersoften go undiagnosed for many years. This ispartly due to the lack of understanding of thecondition by individual sufferers and healthprofessionals alike and the intense feelingsof embarrassment, guilt and sometimes evenshame, associated with what is often calledthe ‘secret illness’, can often prevent sufferersfrom seeking appropriate treatment. It is notuncommon for a sufferer to wait an averageof 10–15 years before seeking help for thecondition.OCD has two main features, theObsessions and the Compulsions.4OCD-UKOCD INFORMATION GUIDE
Obsessions - an explanationIn general, the obsessions experienced byOCD sufferers take the form of persistentand uncontrollable thoughts, images,impulses, worries, fears or doubts. They areoften intrusive and disturbing by nature,and significantly interfere with the ability tofunction on a day-to-day basis.The occurrence of these obsessive thoughtsusually produces a feeling best described asanxiety, but some patients report that what theyfeel is not anxiety, but general unease, tensionand discomfort.For the most part, people with OCD veryoften realise that their obsessive thoughtsare irrational, but they believe the only wayto relieve the anxiety caused by them isto perform compulsive behaviours, oftento prevent perceived harm happening tothemselves or, more often than not, to a lovedone. Some sufferers, however, are not able torecognise the intrusive nature of their thoughts,and the very fact that they are having them cancause them extreme distress. Worrying that you or something/someone/somewhere is contaminated.Worrying about catching HIV/AIDS orother media publicised illnesses such asBird Flu or Swine Flu.Worrying about causing physical or sexualharm to yourself or others, and havingIntrusive violent thoughts.Unwanted or unpleasant sexual thoughtsand feelings, including those aboutsexuality or fear of acting inappropriatelytowards children.Worrying that you have caused anaccident whilst driving.Having the unpleasant feeling that you areabout to shout out obscenities in public.Worrying that everything needs tobe arranged symmetrically or atperpendicular angles so everything is‘just right’.Worrying that something terrible willhappen unless you check repeatedly.The problem is that the person with OCD willbecome besieged by the obsessive thoughts. Infact the word ‘obsession’ comes from the Latin‘obsidere’ which means ‘to besiege’. Naturallythe sufferer neither wants nor welcomes theobsessional thoughts and will go to extremelengths to block and resist them. Invariablythey return within a short period of time, oftenlasting hours if not days, which can leave theperson both mentally and physically exhaustedand drained. This causes deep anguish anddespair.The list opposite details just someexamples of commonly occurringobsessions that affect peoplewith OCD:OCD-UKWWW.OCDUK.ORG5
Compulsions - an explanationCompulsions can either be repetitive physicalbehaviours and actions, or mental thoughtrituals that are performed over and over againin an attempt to relieve the anxiety caused bythe obsessive thoughts. Avoidance of places orsituations, to prevent triggering these obsessivethoughts, is also considered to be a compulsion.Sadly any relief that the compulsive behavioursprovide is only temporary and short lived, andoften reinforces the original obsession, creatinga gradual worsening cycle of the OCD.In most cases OCD sufferers recognise theircompulsive actions are senseless and irrational,but none-the-less feel bound to carry them out inorder to prevent harm coming to themselves orloved ones. Often a person with OCD will feela heightened sense of responsibility to performthe neutralising behaviour, simply becausethey feel doing so will prevent harm coming tothemselves or loved ones. What’s more suffererssometimes have an overwhelming urge to obtainthat ‘just right’ feeling with no other reason thanto feel comfortable.For example; people without the illness willwash their hands when they are dirty and‘see’ that they are dirty. In contrast someonewith OCD will ‘feel’ their hands are dirty, andtherefore keep washing until they ‘feel’ clean.The list below details just some examplesof commonly-occurring physical or mentalcompulsions that affect people with OCD (inbrackets are types of obsessional thoughts thatmay trigger such compulsive behaviours): 6Excessive washing of one’s hands orbody (thought of being contaminated, bychemical or body fluids).Excessive cleaning of clothes or roomsin the house, (thought of having comeinto contact with germs from the outsideor perceived contaminants from bodilyfluids).Checking that items are arranged‘just right’ and constantly adjustinginconsequential items, until they arealigned to feel ‘just right’ as opposed tolooking aligned (thought that somethingbad may happen if not aligned correctly).OCD-UK Mental rituals or thought patterns suchas saying a particular phrase, or countingto a certain number, to ‘neutralise’an obsessional thought (thought thatsomething bad may happen if not carriedout).Repeatedly opening and sealing letters /greetings cards that one has just written,maybe hundreds of times (fear of writingsomething offensive within the letter/card).Constant checking of light switches,handles, taps, locks etc to preventperceived danger from flooding, break in,gas leak or fire.Avoiding particular places, people orsituations to avoid an OCD thought (be itfear of harming, or contamination).Saying out loud (or quietly) specific wordsin response to other words (to preventdisaster happening).Avoidance of kitchen knives and othersuch instruments, (for example lockingthem in a drawer) to prevent cominginto contact with them (thought ofharming someone).A compulsion can either be overt (i.e.observable by others), such as checking thata door is locked, or covert (cognitive) (anunobservable mental act), such as repeating aspecific phrase in the mind, or avoiding people,objects or situations.Overt compulsions typically include checking,washing, hoarding or symmetry of certain motoractions.Covert compulsions, or ‘cognitivecompulsions’, as they are sometimes referredto, are the carrying out of mental actions, asopposed to physical ones. Examples includemental counting, compulsive visualisation andsubstitution of distressing mental images orideas with neutralising alternatives.Another key compulsive behaviour, particularlywhere the sufferer lives with another person, isthe need to seek constant ‘reassurance’. This initself is another compulsion.OCD INFORMATION GUIDE
OCD spectrum disordersThere are a number of disorders whichresearchers have long believed to bebiologically linked to OCD, and thus havebeen categorised as OCD spectrum disorders.These include: Body Dysmorphic Disorder,Compulsive Skin PickingTourette SyndromeTrichotillomaniaHowever, it is now felt that Body DysmorphicDisorder is perhaps the closest linked of allthese disorders to OCD, with the others beingdifferent conditions in their own right, althoughthe common factor in all of these conditionsis that they do all involve, to some degree, thepresence of repetitive thoughts, behaviours orurges.When two diagnoses occur in the sameindividual they are referred to as ‘comorbid’.Many people with these other conditionswill also be comorbid and display OCD typesymptoms, and be diagnosed with OCD whichis why they are still considered to be relateddisorders.Body Dysmorphic Disorder (BDD)Body Dysmorphic Disorder (BDD) is oftencalled the ‘imagined ugliness’ disorder. It wasformerly known as Dysmorphophobia andis an anxiety disorder whereby a person isabnormally preoccupied with an imagined orslight defect in their physical appearance.Compulsive Skin PickingCompulsive Skin Picking (CSP), also knownas Dermatillomania, is an impulse controldisorder and is characterised by the habitualand excessive picking of skin lesions, or theexcessive scratching, picking, gouging orsqueezing of otherwise healthy skin, to theextent of causing bleeding, bruising, infection,and/or permanent disfigurement. Thesebehaviours are carried out solely to relievethe anxiety or urges being experienced by thesufferer.OCD-UKTourette SyndromeTourette Syndrome (TS) is a neurologicaldisorder characterised by sudden rapid,involuntary movements called tics, which occurrepeatedly. It is thought to be an inheritedneurological condition which affects morethan 300,000 children and adults in the UK. Inmost instances it starts in childhood, and forabout half of children with TS, the conditioncontinues into adulthood.TrichotillomaniaTrichotillomania (Pronounced: trick-oh-tilloh-may-nee-ah) is a type of psychologicaldisorder known as an impulse control disorder.Its defining characteristic is the recurrent,compulsive pulling of the hair out at theroot, from places like the scalp, eyebrows, oreyelashes, sometimes causing baldness. Pullingmay also occur from less common locationsincluding the pubic area, perirectal area, or anyother body region.Other DisordersThere are also a number of other disorderswhich often affect people with OCD. Althoughthese conditions are not in the OCD spectrumof disorders, they run alongside the OCD andare often a consequence of OCD. These includeDepression, Emetophobia, Panic Attacks andSelf-Harm.WWW.OCDUK.ORG7
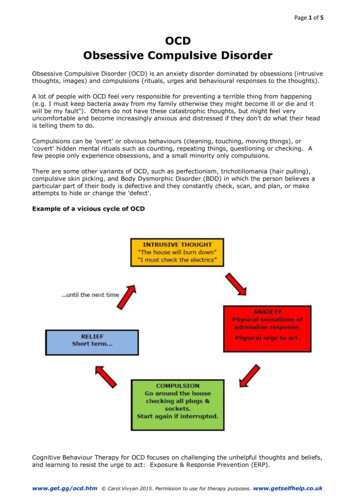
Understanding OCDUnderstanding what drives a person tocontinue performing the seemingly nonsensicaland repetitive behaviours, that ObsessiveCompulsive Disorder (OCD) creates, isdifficult, but partly it is due to the perception ofthe perceived level of danger and threat that aperson with OCD believes may cause harm tothemselves or a loved one.For many people with OCD there is also anoverinflated sense of responsibility to preventharm and over estimation about the perceivedthreat the intrusive thoughts bring. It is thesefactors which help drive their compulsivebehaviours, because they feel responsible to tryand prevent bad things happening.The problem that OCD creates is an increasein anxiety. Whilst a normal response to ananxiety provoking situation is for the anxietyto slowly decrease after the initial event, forsomeone with OCD the anxiety is maintainedand often increases, usually because of theiroverestimation of the perceived level of threat.The problem with the anxiety is that it isproportional to a person’s perception ofdanger and risk. The worse the perceivedconsequences the greater is the fear ofsomething bad happening.The level of perceived risk would beconsiderably higher, and the resulting anxietywill become considerably higher too, and theneed to prevent that risk becomes stronger.OCD becomes a vicious cycle. As theobsessional thought causes a person’s anxietyto increase, they become besieged by theobsessive thoughts. Naturally the suffererneither wants nor welcomes the obsessionalthoughts and will go to extreme lengths toblock and resist them.People with OCD realise that their obsessionalthoughts are irrational, but they believe theonly way to relieve the anxiety caused bythe obsessions is to perform compulsivebehaviours, often to prevent perceived harmhappening to themselves or more often thannot, a loved one.Unfortunately, any relief that the compulsivebehaviours provide is only temporary and oftenreinforce the original obsession, creating agradual worsening cycle of the OCD.As an example, imagine that you’ve been toldthat you have to walk a 30-foot-long plank,which is one foot wide and is two feet abovesoft ground. For most people the perceived riskwould be low, the task would seem easy and sothe anxiety is low and manageable, and fadesquickly.Now what if we tell youthat the 30-foot-longplank, which was onefoot wide and is two feetabove soft ground is nowjust half a foot wide, andhundreds of feet above acanyon?8OCD-UKOCD is driven by the fear of consequences, nomatter how unlikely the risk.The reality is that OCD is like a pair of Chinesehandcuffs, the harder you pull to get away (thecompulsions), the tighter the grip becomes (theobsessions).OCD INFORMATION GUIDE
You don’t haveto suffer
Treatments for OCDOCD can be an extremely isolating, upsettingand distressing illness. But while it can bechronic, it is also a very treatable medicalcondition, and seeking early intervention andappropriate treatment is the key to long termrecovery.The treatment found to be the most effectivein successfully treating OCD is CognitiveBehavioural Therapy (CBT). In many cases,CBT alone is highly effective in treating OCD,but for some people a combination of CBT andmedication is also effective. Medication mayreduce the anxiety enough for a person to start,and eventually succeed in therapy.However what we know is that left uncheckedand untreated OCD will mushroom and feedupon itself and can have the power to consumeif left unchallenged. It is therefore important toseek professional medical advice and supportthe moment someone recognises OCD typesymptoms.NHS RouteBefore any kind of treatment for ObsessiveCompulsive Disorder can commence youshould always consult your GP. If you areworried about doing this, we have a GPicebreaker sheet (available to download on ourwebsite) which can sometimes make that firstGP visit a little easier.While some GPs still have a limited knowledgeof the wide range of symptoms of OCD, this isnow slowly changing. However, the symptomsoften still go unrecognised and, as a result,undiagnosed by GPs. If this happens to you,it may be that you have to tell your GP whatOCD is, as well as what your symptoms are.You may also wish to refer your GP to theclinical classifications of the illness on ourwebsite and the National Institute for Healthand Clinical Excellence (NICE) guidelines forthe identification, treatment and management ofOCD and BDD.In general, doctors, nurses and other healthcareprofessionals within the NHS are all expectedto follow NICE’s clinical guidelines.10OCD-UKWhen you first see a health care professionalabout your symptoms, it is very important thatyou are honest and open about your thoughtsand behaviours, no matter how embarrassingthey may seem. Almost certainly, they haveheard it all before – and by being honest, youwill help them to identify the most suitabletreatment for you.After an initial appointment your GP shouldrefer you to your local Community MentalHealth Team (CMHT) or Improving Accessto Psychological Therapies (IAPT) team, orits local equivalent. Here you are likely to beseen by an appropriate clinical psychologist orpsychiatrist who will ensure a correct diagnosisand recommend a course of treatment.Subsequent treatment may then involve apsychologist, psychiatrist or another mentalhealth professional such as a community mentalhealth nurse (CPN).The treatment you should be offered isCognitive Behavioural Therapy (a form oftalking therapy). You may also be offeredmedication to help with your recovery. Moreabout these will be discussed later on in thebooklet.Exposure and Response Prevention (ERP)should also form part of the CBT treatment.This involves being exposed in a verystructured way, with the support of yourtherapist, to whatever it is that makes you feelanxious, without then engaging in the checkingor other OCD behaviours.Medication is not recommended as a soletreatment method, although in practice your GPmay well offer drug treatment straight awaybecause of the long waiting lists for CognitiveBehavioural Therapy. If this happens, itshould be your choice whether to accept themedication, and if you do, you should alsodiscuss the possible side effects with your GP.In many cases, CBT alone is highly effective intreating OCD, but for some people with OCDa combination of CBT and medication is moreeffective.OCD INFORMATION GUIDE
Treatments for OCDThis usually takes the form of antidepressantswhich act in the Serotonin System, and they arecalled SSRIs (Selective Serotonin Re-uptakeInhibitor).providing national guidance on treatments andcare for people using the NHS in England andWales. It is the world leader in setting highquality healthcare standards.Occasionally you may only be offered groupCognitive Behavioural Therapy, often inan attempt to keep long waiting lists down.However, you should always request individualone-to-one therapy, even though it is sometimeshelpful for people who have the same type ofOCD problems to receive therapy as a group.However group therapy should not be offeredto you as a sole treatment because this won’t betailored to your individual needs and it may nothave the same impact as individual treatment.Sharing sessions with other people cansometimes help you realise you’re not alonewith your problem and enables each member tocontribute to the progress and wellbeing of theothers, but this can also be found through nontherapeutic support groups.NICE and the National Collaborating Centrefor Mental Health launched their set of clinicalguidelines for the identification, treatmentand management of Obsessive-CompulsiveDisorder and Body Dysmorphic Disorder on23rd November 2005.Self Help RouteMany people with OCD decide to try and beatOCD themselves using resources they pickup from self-help books, support groups andwebsites like the OCD-UK website atwww.ocduk.org. There are many self-helpresources out there, but it is important that youare careful and do not assume everything youread on the internet is correct. Sometimes beingable to run things past a trained mental healthprofessional can be better than attempting theself-help route.Private TherapistsWhen choosing a therapist, especially ifpaying to go private, it is important to makesure your therapist is suitably qualified to betreating you, so it is important to ask somerelevant questions to allow you to gauge if yourtherapist seems knowledgeable enough in howto treat OCD. You can read more about this onour website, under ‘Finding a therapist’.The guidance is intended for health careprofessionals, patients and their carersto help them make decisions abouttreatment and health care. Unfortunately,despite breakthroughs in the awareness,understanding and treatment of OCD, manyhealth professionals still do not recognisethe symptoms, or know how to correctlytreat the disorder. If this is the case for you,you may wish to refer your GP to the NICEguidelines for the identification, treatment andmanagement of OCD and BDD.To obtain copies of the guidelines, there areseveral options: Download them from our website atwww.ocduk.org.Obtain a hard copy from OCD-UK.Please send two first class stamps whenrequesting your copy.Order copies by calling the NHS ResponseLine on 0845 003 7783 (national rate)and asking for: N0920 Information forthe public or N0919 Quick referenceguide for healthprofessionals.NICE Guidelines for OCDThe National Institute for Health and ClinicalExcellence (NICE) is part of the NHS and isthe independent organisation responsible forOCD-UKWWW.OCDUK.ORG11
Cognitive Behaviour Therapy - an explanationCognitive Behaviour Therapy (CBT) is aspecial form of talking therapy which is thetreatment found to be the most effective insuccessfully tackling Obsessive-CompulsiveDisorder (OCD).The principal aim of this therapeutic approachis to enable the person to become theirown therapist and to provide them with theknowledge and tools to continue workingtowards complete recovery from OCD. Whattherapy will teach the person with OCD is thatit’s not the thoughts themselves that are theproblem; it’s what the person makes of thosethoughts, and how they respond to them, that isthe key to recovery.A good way of understanding how differentresponses to thoughts can affect the way webehave can be demonstrated in the examplebelow, which sufferers and non-sufferers alikewill be able to relate to.It’s the middle of the night, you’re in bed. Youhear a noise from downstairs. You might think: ‘It’s the stupid cat again’,feel angry, put your head under the pillowand try to go back to sleep. You might think: ‘It’s my partner comingin, I haven’t seen them all day!’, feelhappy and get out of bed to say ‘hello’. You might think: ‘It’s a burglar’, feelfrightened and call the police.What this example shows is that the same eventcan make people feel completely differentemotions (angry, happy, anxious), and result inthem behaving in very different ways, due totheir different beliefs about the event.In summary, it’s not the thoughts themselvesthat are the focus of treatment; it’s what wemake of those thoughts in the first place.Cognitive Behaviour Therapy makes use oftwo evidence-based behaviour techniques,Cognitive Therapy (C) that looks at how wethink, and Behaviour Therapy (B) which looksat how this affects what we do. In treatment weconsider other ways of thinking (C), and howthis would affect the way we behave (B).12OCD-UKExposure and Response Prevention therapy(ERP) is used as part of the behaviouralapproach to help explore alternative ways torespond to the obsessional thoughts or doubts.What we also know from research is that almosteveryone has intrusive thoughts, that are eithernonsensical or alarming. The aim of CBT isnot about learning not to have these thoughtsin the first place, because in essence, as will bediscussed later, intrusive thoughts cannot beavoided. Instead it is about helping a personwith OCD to identify and modify their patternsof thought that cause the anxiety, distress andcompulsive behaviours.The goal of treatmentIn treatment for OCD, one of the first things aperson will be asked to do is to think of a recentspecific example of when the OCD was reallysevere. They will be asked to go into a lot ofdetail, and try and understand what thought(s)(or doubts, images or urges) popped into theirhead at this time.For example some intrusive thoughts might be: A horrible thought that I may have saidsomething inappropriate.A thought that there might be blood in myfood.A thought that I am contaminated from thetoilet.People with OCD often ask if treatment canhelp them get rid of these intrusive thoughts,as they are so distressing and horrible. Butif you instead consider whether all intrusivethoughts are always horrible you will see thatthey are not. Usually people can think of anoccasion when they suddenly had a thought thatwas helpful, such as suddenly rememberinga friend’s birthday is coming up, or having amemory of a lovely holiday pop into their head.We can conclude from this that getting rid ofintrusive thoughts themselves isn’t a realistic,or sometimes, desirable goal.It is also worth remembering that everyone hasall sorts of intrusive thoughts – including thenasty ones: thoughts of harm coming to people,images of violence, urges to check things,OCD INFORMATION GUIDE
Cognitive Behaviour Therapy - an explanationdoubts about whether they have donesomething. The difference with other peopleis that their intrusive thoughts do not becomebothersome.The goal of treatment therefore is not to get ridof the thoughts, but to learn different ways ofresponding to them.The cyclical nature of the problem can beillustrated by drawing a diagram of how itworks - we sometimes call it the ‘viciousflower’ – one of Professor Paul Salkovskis’sdiagrams shows the general idea.Challenging the meaning attached tothe thoughtsIn CBT the person with OCD will explorealternative meanings or beliefs about theintrusive thoughts and rituals in all their guises(for example washing, checking, writing lists,tapping, touching, repeating, cleaning, tryingto get a ‘just right’ feeling, praying) and willlearn what it is that ultimately keeps alive themeanings they attach to such thoughts andrituals.So during the first few sessions a good therapistshould spend time making sense of how theOCD works and what keeps it going. Theidea and reason behind this is that if we canunderstand the factors that keep a problemalive, we can then take the next step, which isto think about alternative ways of viewing theproblem and what we can then do to change it.Therefore in CBT we look at how OCDconvinces you that the rituals and compulsionsperformed are necessary, in order to preventsomething bad happening. If such a badoutcome were to be true as a result of thethought, the sufferer would be convinced itwas entirely their fault and responsibility. Wealso look at the possibility that OCD is a liar.All the sufferer’s coping strategies have comeabout in the first place to make them feel saferand less anxious, when in fact they do the exactopposite, they make the person feel unsafe andscared. Even if they provide temporary relieffrom anxiety, all these rituals make the meaningattached to those intrusive thoughts, images,urges and doubts feel even stronger, thereforeit becomes necessary for the sufferer to keepdoing the rituals continuously. Ultimately thismakes the thoughts seem even more real, andlike there is even more truth in them.OCD-UKSo how do we deal with all these rituals? Hereis one common example, along with an idea ofpossible ways they may be tackled in CBT.CheckingChecking is a common OCD ritual. During acourse of CBT, the sufferer might be asked totry ‘behavioural experiments’ to find out wh
OCD-UK would like to thank two of our volunteers, Alison and Leigh for their contributions towards compiling this information guide. We remain grateful for the kind support and commitment of them, and all of our fantastic volunteers. Around 1.2% of the population are thought to be affected by Obsessive-Compulsive Disorder (OCD) and