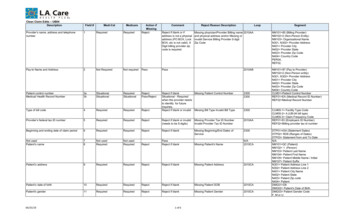
Transcription
Overview of the Patient-Driven Groupings Model (PDGM)February 12, 2019Presenters:Kelly Vontran, Technical Advisor, Division of Home Health and HospiceWil Gehne, Technical Advisor, Division of Institutional Claims Processing
Acronyms in this Presentation BLS: Bureau of Labor Statistics CPM NRS: Cost per Minute Non-RoutineSupplies MMTA: Medication Management, Teaching, andAssessment MS: Musculoskeletal CY: Calendar Year MSS: Medical Social Services HH PPS: Home Health Prospective Payment System OASIS: Outcome and Assessment Information Set HH: Home Health OT: Occupational Therapy HHAs: Home Health Agencies PDGM: Patient-Driven Groupings Model HHRGs: Home Health Resource Groups PT: Physical Therapy HIPPS: Health Insurance Prospective PaymentSystem RAP: Request for Anticipated Payment ICD: International Classification of Diseases SN: Skilled Nursing IV: Intravenous WWMC: Wage Weighted Minutes of Care SLP: Speech Language Pathology LUPA: Low Utilization Payment Adjustment MedPAC: Medicare Payment Advisory Commission2
Agenda1. Current HH PPS**8. Comorbidity Group2. Overview of the PDGM9. Case-Mix Weights3. Measuring Period Costs10. Other Adjustments4. 30-Day Periods5. Admission Source and Timing11. Grouper Tool andExample Scenarios6. Clinical Groups12. Operational Changes7. Functional Impairment Levels** indicates section to follow3
Current Home Health Prospective Payment System (HH PPS) Implemented in October 2000‒ Bundled payment for all covered HH services provided in a 60-day episode Level of payment determined by case-mix adjustment‒ Allows different payment for patients with different needs Differential resource use intensity measured using wage-weighted minutes ofcare (WWMC)‒ Amount of time multiplied by average wages from the Bureau of Labor Statistics (BLS) byhome health discipline4
Current Home Health Prospective Payment System, continued Home Health Agencies (HHAs) complete the Outcome and AssessmentInformation Set (OASIS) for each patient Result of the assessment groups episode into one of 153 Home HealthResource Groups (HHRGs)‒‒‒‒Timing (early/late episodes; exception 20 therapy group)3 clinical levels3 functional levels9 service use categories (number of therapy visits) HHRG is the starting point for payment calculation5
Current Home Health ProspectivePayment System, continued153 Home Health Resource Groups (HHRGs)based on severity levels: Clinical: whether the patient has one or moreclinical conditions such as incontinence; intravenousinfusion (IV), enteral, or parenteral therapies; thepresence of wounds or pressure ulcers, etc. Functional: whether the patient has problems withactivities of daily living such as dressing, bathing,transferring, walking (locomotion), and toileting Service utilization: based on the number of therapyvisits during the episodeSource: MedPAC Payment Basics as of 10/14/16.Available at: http://www.medpac.gov/-documents-/payment-basics6
Motivation for Development of the PDGM ‒Section 3131(d) Report to Congress Section 3131(d) of the Affordable Care Act - Report to Congress found currentpayment system produced lower margins for those patients:‒‒‒‒‒‒‒needing parenteral nutritionwith traumatic wounds or ulcerswho required substantial assistance in bathingadmitted to HH following an acute or post-acute staywho have a high Hierarchical Condition Category scorewho had certain poorly controlled clinical conditionswho were dual eligibleSource: ongress.pdf7
Motivation for Development of the PDGM –MedPAC Annual Reports (2011, 2015, 2017) The Medicare HH benefit is ill-defined HH payment should not be based on the number of therapy visits‒ Payments based on therapy thresholds creates financial incentives that distract agencies fromfocusing on patient characteristics when setting plans of care.‒ Trend of notable shifts away from non-therapy visits. HH payment should be determined by patient characteristicsSource: Mar11 Ch08.pdf?sfvrsn port-.pdf?sfvrsn /mar17 medpac ch9.pdf8
Development of the PDGM Reexamined payment reform principles‒ Improve payment accuracy for HH services‒ Promote fair compensation to HHAs‒ Increase the quality of care for beneficiaries Conducted initial analytic work‒ Assessing utilization of current payment system‒ Considered alternative approaches to construct case-mix weights Diagnosis on top Predicted therapy Home Health Groupings Model Payment reform solidified by Bipartisan Budget Act of 2018‒ Payment based on 30-day periods (instead of 60-day episodes)‒ Elimination of therapy thresholds9
Agenda1. Current HH PPS8. Comorbidity Group2. Overview of the PDGM**9. Case-Mix Weights3. Measuring Period Costs10. Other Adjustments4. 30-Day Periods5. Admission Source and Timing11. Grouper Tool andExample Scenarios6. Clinical Groups12. Operational Changes7. Functional Impairment Levels** indicates section to follow10
Patient-Driven Groupings Model (PDGM) The PDGM is a new payment model for the Home Health Prospective PaymentSystem (HH PPS) that relies more heavily on clinical characteristics and otherpatient information to place home health periods of care into meaningfulpayment categories and eliminates the use of therapy service thresholds. PDGM will take effect January 1, 2020. In conjunction with the implementation of the PDGM there will be a change inthe unit of home health payment from a 60-day episode to a 30-day period.11
How the Patient-Driven GroupingsModel Works Five main case-mix variables—1.Admission Source2.Timing3.Clinical Grouping4.Functional Impairment Level5.Comorbidity Adjustment A 30-day period is grouped into one subcategory in each colorcategory This results in 432 possible case-mix adjusted paymentgroups into which a 30-day period can be placed:(2*2*12*3*3 432 HHRGs)1 Gastrointestinal2 Thetract/Genitourinary systeminfectious disease category also includes diagnoses related to neoplasms and blood-forming diseases12
Agenda1. Current HH PPS8. Comorbidity Group2. Overview of the PDGM9. Case-Mix Weights3. Measuring Period Costs**10. Other Adjustments4. 30-Day Periods5. Admission Source and Timing11. Grouper Tool andExample Scenarios6. Clinical Groups12. Operational Changes7. Functional Impairment Levels** indicates section to follow13
Measuring 30-Day Period Costs Under PDGM Need to measure period costs to calculate case-mix adjustmentfactors that account for variation in costs among different units ofservices. Cost per Minute plus Non-Routine Supplies (CPM NRS) Approach‒ Uses Medicare cost reports and better reflects total HHA costs‒ Incorporates NRS into the base payment instead of requiring a separatemodel (as is done under the current payment system)14
Cost per Minute plus Non-Routine Supplies (CPM NRS)Data Sources Cost reports, HH Medicare claimsGeneral Approach Total costs multiplied by amount of care provided for each disciplineCosts RepresentedWages, fringe benefits, overhead costs, transportation costs, other nonvisiting services labor costsNon-Routine Supply Use NRS cost-to-charge ratio to obtain NRS costs per period15
Agenda1. Current HH PPS8. Comorbidity Group2. Overview of the PDGM9. Case-Mix Weights3. Measuring Period Costs10. Other Adjustments4. 30-Day Periods**5. Admission Source and Timing11. Grouper Tool andExample Scenarios6. Clinical Groups12. Operational Changes7. Functional Impairment Levels** indicates section to follow16
30-Day Periods In the current HH PPS, HHAs are paid for each (up to) 60-day episode of careprovided. However, more visits tend to occur in the first 30-day period of a 60-day episodeof care. For the PDGM, payment is made for each 30-day period, as required by theBBA of 2018. Only affects payment, no changes to the requirements forcertification/recertification, completion of OASIS assessments, or updates to thepatient’s plan of care, all of which continue to be done on a 60-day basis.17
National, Standardized 30-day Period Payment Amount The PDGM will not be implemented until CY 2020. However, to provide HHAs with a sense of the payment amount for a30-day period of care, we estimated that if the PDGM was implementedin CY 2019, the estimated national, standardized 30-day paymentwould be: 1,753.68 This 30-day payment amount will be updated for CY 2020.18
Agenda1. Current HH PPS8. Comorbidity Group2. Overview of the PDGM9. Case-Mix Weights3. Measuring Period Costs10. Other Adjustments4. 30-Day Periods5. Admission Source and Timing**11. Grouper Tool andExample Scenarios6. Clinical Groups12. Operational Changes7. Functional Impairment Levels** indicates section to follow19
Periods are Grouped byAdmission Source and Timing Admission source‒ Institutional versus community Period timing‒ Early versus late20
Admission Source Institutional:‒ Acute (inpatient acute care hospitals), or;‒ Post-acute (skilled nursing facility, inpatient rehabilitation facility, long term carehospital, or inpatient psychiatric facility) care in the 14 days prior to the HHadmission Community: No acute or post-acute care in the 14 days prior to the HHadmission 30-day periods with an institutional admission source were found to have higherresource use than periods with a community admission source21
Timing Sequence of HH periods: Periods with no more than 60 daysbetween the end of one period and the start of the next period (nochange from current definition) Early periods: the first 30-day period in a sequence of HH periods Late periods: second and later 30-day periods in a sequence of HHperiods22
Additional Notes on Admission Source and Timing Late 30-day periods are always classified as a community admission unless there is anacute hospitalization in the 14 days prior to the late home health 30-day period (HHAshave the option whether or not to discharge the patient if the patient is hospitalized for ashort period of time). A post-acute stay in the 14 days prior to a late home health 30-day period would not beclassified as an institutional admission unless the patient had been discharged fromhome health prior to post-acute stay (which is what we would expect to occur). Information will come from Medicare systems during claims processing to automaticallyassign admission source and timing categories. HHAs have the option to include an occurrence code on the claim to identify aninstitutional admission source.23
Agenda1. Current HH PPS8. Comorbidity Group2. Overview of the PDGM9. Case-Mix Weights3. Measuring Period Costs10. Other Adjustments4. 30-Day Periods5. Admission Source and Timing11. Grouper Tool andExample Scenarios6. Clinical Groups**12. Operational Changes7. Functional Impairment Levels** indicates section to follow24
Periods are Grouped by PrimaryReason for Home Health underthe PDGM Clinical groups are intended to reflectthe primary reason for HH services Defined by the principal diagnosisreported on HH claim Twelve total groups used in the PDGM25
Description of the 12 Clinical GroupsClinicalGroupDescriptionMain reason for HH encounter is to provide:1Musculoskeletal RehabilitationTherapy (PT/OT/SLP) for a musculoskeletal condition2Neuro/Stroke RehabilitationTherapy (PT/OT/SLP) for a neurological condition or stroke3Wounds-Post Op Wound Aftercare and Skin/Non-Surgical Wound CareAssessment, treatment and evaluation of a surgical wound(s);assessment, treatment and evaluation ofnon-surgical wounds, ulcers, burns and other lesions4Complex Nursing InterventionsAssessment, treatment and evaluation of complex medical and surgicalconditions (e.g., ostomies, TPN)5Behavioral Health CareAssessment, treatment and evaluation of psychiatric and substanceabuse conditions26
Description of the 12 Clinical Groups, continuedClinicalGroupDescriptionMain reason for HH encounter is to provide:Medication Management, Teaching and Assessment (MMTA)6. MMTA-Surgical Aftercare7. MMTA-Cardiac/Circulatory8. MMTA-Endocrine6-129. MMTA-GI/GU10. MMTA-Infectious Disease/Neoplasms/Blood-forming Diseases11. MMTA-RespiratoryAssessment, evaluation, teaching, and medicationmanagement for a variety of medical and surgicalconditions not classified in one of the previous groups.The subgroups represent common clinical conditionsthat require home health services for medicationmanagement, teaching and assessment.12. MMTA-Other27
ICD-10 Codes Used to Determine Clinical Group 30-day period assigned to clinical group based on principal diagnosis code onthe claim. The average resource use of all 30-day periods within a clinical group variesacross clinical groups and the payment reflects those differences. If a diagnosis code is used that does not fall into a clinical group (e.g., dentalcodes or other uncovered/invalid codes), claim is returned to the provider formore definitive coding. Additional adjustments made for other health conditions (discussed later).28
Agenda1. Current HH PPS8. Comorbidity Group2. Overview of the PDGM9. Case-Mix Weights3. Measuring Period Costs10. Other Adjustments4. 30-Day Periods5. Admission Source and Timing11. Grouper Tool andExample Scenarios6. Clinical Groups12. Operational Changes7. Functional Impairment Levels**** indicates section to follow29
Periods are Grouped byFunctional Impairment Levelunder the PDGM 30-day periods are categorized into oneof three functional impairment levels Certain OASIS items are used to createthe levels30
PDGM Functional Impairment Level Based on Responses toSeven OASIS ItemsFunctional OASIS ItemsCurrent Payment SystemPDGMM1800: GroomingNoYesM1810: Current ability to dress upper body safelyYesYesM1820: Current ability to dress lower body safelyYesYesM1830: BathingYesYesM1840: Toilet TransferringYesYesM1850: TransferringYesYesM1860: Ambulation/LocomotionYesYesM1033: Risk for hospitalizationNoYes31
Steps for Creating the Functional Impairment Levels Determine points for response groups‒ Resource use is regressed on the seven OASIS items (along with other covariates fromeach of the PDGM groups)‒ Regression coefficients determine the number of points‒ Points reflect relative resource group (high intensity, greater number of points) Calculate the functional score‒ For each 30-day period, points are summed to determine an overall functional score Assign functional impairment level using score‒ Within each PDGM diagnosis grouping, periods are split into thirds and assigned to a low,medium, or high functional impairment group32
Functional Impairment Levels and Associated PointsThresholds for Functional Levels by Clinical Group, CY 2017Clinical GroupBehavioral HealthComplex Nursing InterventionsMusculoskeletal RehabilitationNeuro RehabilitationWoundMMTA - Surgical AftercareLevel of ImpairmentPoints (2017 Data)LowMediumHighLowMediumHighLow0-3637-5253 0-3839-5859 ediumHigh53 0-4445-6061 0-4243-6162 0-2425-3738 33
Functional Impairment Levels and Associated Points, continuedThresholds for Functional Levels by Clinical Group, CY 2017Clinical GroupMMTA - Cardiac and CirculatoryMMTA - EndocrineMMTA - Gastrointestinal tract and Genitourinary systemMMTA - Infectious Disease, Neoplasms,and Blood-Forming DiseasesMMTA - RespiratoryMMTA - OtherLevel of ImpairmentPoints (2017 iumHighLow0-3637-5253 0-5152-6768 0-2728-4445 0-3233-4950 0-29Medium30-43*HighLowMediumHigh44 0-3233-4849 34
Agenda1. Current HH PPS8. Comorbidity Group**2. Overview of the PDGM9. Case-Mix Weights3. Measuring Period Costs10. Other Adjustments4. 30-Day Periods5. Admission Source and Timing11. Grouper Tool andExample Scenarios6. Clinical Groups12. Operational Changes7. Functional Impairment Levels** indicates section to follow35
Periods are Grouped by aComorbidity Adjustment The PDGM includes a comorbidityadjustment category based on thepresence of secondary diagnoses A 30-day period may receive‒ no comorbidity adjustment,‒ a low comorbidity adjustment,‒ or a high comorbidity adjustment36
Comorbidity Adjustment The principal HHA-reported diagnosis determines the PDGM clinical group. However, secondary diagnoses also impact resource use and should be takeninto account. A comorbidity is defined as a medical condition coexisting in addition to aprincipal diagnosis.‒ Comorbidity is tied to poorer health outcomes, more complex medical need andmanagement, and higher care costs.37
Comorbidities Specific to Home HealthA HH specific comorbidity list was developed with broad clinical categories usedto group comorbidities within the PDGM:‒‒‒‒‒‒‒Heart diseaseRespiratory diseaseCirculatory diseaseCerebral vascular diseaseGastrointestinal diseaseNeurological conditionsEndocrine disease‒‒‒‒‒NeoplasmsGenitourinary/Renal diseaseSkin diseaseMusculoskeletal diseaseBehavioral health issues (includingsubstance use disorders)‒ Infectious diseases38
Comorbidities Specific to Home HealthHome health 30-day periods of care can receive a comorbidity adjustment underthe following circumstances: Low comorbidity adjustment: There is a reported secondary diagnosis that isassociated with higher resource use, or; High comorbidity adjustment: There are two or more secondary diagnosesthat are associated with higher resource use when both are reported togethercompared to if they were reported separately. That is, the two diagnoses mayinteract with one another, resulting in higher resource use. No comorbidity adjustment: there is no reported secondary diagnosis thatfalls in either the low or high comorbidity adjustment.39
Low Comorbidity Adjustment SubgroupsAs shown in the CY 2019 HH PPS Final Rule (83 FR 56487)Comorbidity SubgroupDescriptionCerebral 4Includes sequelae of cerebral vascular diseasesCirculatory 10Includes varicose veins with ulcerationCirculatory 9Includes acute and chronic embolisms and thrombosisHeart 10Includes cardiac dysrhythmiasHeart 11Includes heart failureNeoplasms 1Includes oral cancersNeuro 10Includes peripheral and polyneuropathiesNeuro 11Includes diabetic retinopathy and other blindnessNeuro 5Includes Parkinson’s diseaseNeuro 7Includes hemiplegia, paraplegia, and quadriplegiaSkin 1Includes cutaneous abscess, cellulitis, lymphangitisSkin 3Includes diseases of arteries, arterioles, and capillaries with ulceration and non-pressure, chronic ulcersSkin 4Includes Stages Two through Four and Unstageable pressure ulcersSource: CY 2017 Medicare claims data for episodes ending on or before December 31, 2017 (as of June 30, 2018).40
High Comorbidity Adjustment Interaction SubgroupsAs shown in the CY 2019 HH PPS Final Rule (83 FR avioral 2Includes depression and bipolar disorderSkin 3Includes diseases of arteries, arterioles, and capillaries withulceration and non-pressure, chronic ulcers2Cerebral 4Includes sequelae of cerebral vascular diseasesCirculatory 4Includes hypertensive chronic kidney disease3Cerebral 4Includes sequelae of cerebral vascular diseasesHeart 10Includes cardiac dysrhythmias4Cerebral 4Includes sequelae of cerebral vascular diseasesHeart 11Includes heart failure5Cerebral 4Includes sequelae of cerebral vascular diseasesNeuro 10Includes peripheral and polyneuropathies6Circulatory 10Includes varicose veins with ulcerationEndocrine 3Includes diabetes with complications7Circulatory 10Includes varicose veins with ulcerationHeart 11Includes heart failure8Circulatory 4Includes hypertensive chronic kidney diseaseSkin 1Includes cutaneous abscess, cellulitis, lymphangitis9Circulatory 4Include hypertensive chronic kidney diseaseSkin 3Includes diseases of arteries, arterioles, and capillaries withulceration and non-pressure, chronic ulcers10Circulatory 4Include hypertensive chronic kidney diseaseSkin 4Includes Stages Two through Four and Unstageable pressureulcersSource: CY 2017 Medicare claims data for episodes ending on or before December 31, 2017 (as of June 30, 2018).41
High Comorbidity Adjustment Interaction Subgroups, continuedAs shown in the CY 2019 HH PPS Final Rule (83 FR rculatory 7Includes atherosclerosisSkin 3Includes diseases of arteries, arterioles, and capillaries withulceration and non-pressure, chronic ulcers12Endocrine 3Includes diabetes with complicationsNeuro 5Includes Parkinson’s disease13Endocrine 3Includes diabetes with complicationsNeuro 7Includes hemiplegia, paraplegia, and quadriplegia14Endocrine 3Includes diabetes with complicationsSkin 3Includes diseases of arteries, arterioles, and capillaries withulceration and non-pressure, chronic ulcers15Endocrine 3Diabetes with complicationsSkin 416Heart 10Includes cardiac dysrhythmiasSkin 417Heart 11Includes heart failureNeuro 10Includes peripheral and polyneuropathies18Heart 11Includes heart failureNeuro 5Includes Parkinson’s disease19Heart 11Includes heart failureSkin 3Includes diseases of arteries, arterioles, and capillaries withulceration and non-pressure, chronic ulcers20Heart 11Includes heart failureSkin 4Includes Stages Two through Four and Unstageable pressureulcersSource: CY 2017 Medicare claims data for episodes ending on or before December 31, 2017 (as of June 30, 2018).Includes Stages Two through Four and Unstageable pressureulcersIncludes Stages Two through Four and Unstageable pressureulcers42
High Comorbidity Adjustment Interaction Subgroups, continuedAs shown in the CY 2019 HH PPS Final Rule (83 FR udes diseases of arteries, arterioles, and capillaries withulceration and non-pressure, chronic ulcers21Heart 12Includes other heart diseasesSkin 322Heart 12Includes other heart diseasesSkin 423Neuro 10Includes peripheral and polyneuropathiesNeuro 524Neuro 3Includes dementiasSkin 325Neuro 3Includes dementiasSkin 426Neuro 5Includes Parkinson’s diseaseRenal 327Neuro 7Includes hemiplegia, paraplegia, and quadriplegia Renal 3Includes nephrogenic diabetes insipidus28Renal 1Includes Chronic kidney disease and ESRDSkin 3Includes diseases of arteries, arterioles, and capillaries withulceration and non-pressure, chronic ulcers29Renal 1Includes Chronic kidney disease and ESRDSkin 4Includes Stages Two through Four and Unstageable pressureulcers30Renal 3Includes nephrogenic diabetes insipidusSkin 4Includes Stages Two through Four and Unstageable pressureulcersSource: CY 2017 Medicare claims data for episodes ending on or before December 31, 2017 (as of June 30, 2018).Includes Stages Two through Four and Unstageable pressureulcersIncludes Parkinson’s diseaseIncludes diseases of arteries, arterioles, and capillaries withulceration and non-pressure, chronic ulcersIncludes Stages Two through Four and Unstageablepressure ulcersIncludes nephrogenic diabetes insipidus43
High Comorbidity Adjustment Interaction Subgroups, continuedAs shown in the CY 2019 HH PPS Final Rule (83 FR sp 5Includes COPD and asthmaSkin 3Includes diseases of arteries, arterioles, and capillaries withulceration and non-pressure, chronic ulcers32Resp 5Includes COPD and asthmaSkin 4Includes Stages Two through Four and Unstageable pressureulcers33Skin 1Includes cutaneous abscess, cellulitis,lymphangitisSkin 3Includes diseases of arteries, arterioles, and capillaries withulceration and non-pressure, chronic ulcers34Skin 3Includes diseases of arteries, arterioles, andcapillaries with ulceration and non-pressure,chronic ulcersSkin 4Includes Stages Two through Four and Unstageable pressureulcers44
Agenda1. Current HH PPS8. Comorbidity Group2. Overview of the PDGM9. Case-Mix Weights**3. Measuring Period Costs10. Other Adjustments4. 30-Day Periods5. Admission Source and Timing11. Grouper Tool andExample Scenarios6. Clinical Groups12. Operational Changes7. Functional Impairment Levels** indicates section to follow45
Home Health Groupings Model: Case-Mix Weights The PDGM assigns separate payment weights to periods for patients withsimilar characteristics and needs:‒ Each 30-day period assigned into one of 432 case-mix groups.‒ Regression using a fixed effects model to measure resource use with the Cost PerMinute (CPM) NRS approach.‒ Each group’s case-mix weight reflects the group’s predicted mean cost relative tothe overall average.‒ New case-mix weights are used to adjust the HH base payment amount; higherresource need periods are assigned higher case-mix weights and thereby receivemore payment.‒ Annual recalibration of the PDGM case-mix weights to reflect the most recentutilization data available at time of rulemaking.46
Agenda1. Current HH PPS8. Comorbidity Group2. Overview of the PDGM9. Case-Mix Weights3. Measuring Period Costs10. Other Adjustments**4. 30-Day Periods5. Admission Source and Timing11. Grouper Tool andExample Scenarios6. Clinical Groups12. Operational Changes7. Functional Impairment Levels** indicates section to follow47
Low Utilization Payment Adjustment Payments for 30-day periods with a low number of visits are not case-mixadjusted, but instead paid on a per-visit basis using the national per-visit rates. Each of the 432 different PDGM payment groups has a threshold thatdetermines if the 30-day period receives this Low-Utilization PaymentAdjustment (LUPA).‒ For each payment group, the 10th percentile value of visits is used to create apayment group specific LUPA threshold with a minimum threshold of at least two foreach group (range is 2-6 visits in a 30-day period).‒ The LUPA thresholds for each of the 432 case-mix groups can be found in Table 32in the CY 2019 HH PPS Final Rule (83 FR 56493) and on the HHA Centerwebpage.48
Partial Payment Adjustment Payments would be adjusted if a beneficiary transfers from one home healthagency to another or is discharged and readmitted to the same agency within30 days of the original 30-day period start date. The case-mix adjusted payment for 30-day periods of that type is pro-ratedbased on the length of the 30-day period ending in transfer or discharge andreadmission, resulting in a partial period payment.49
Outlier Payment Periods that have estimated costs of care (the wage-adjusted costs) that exceeda specific outlier threshold receive an outlier payment to cover a portion of thehigh costs associated with that 30-day period. The approach to calculating the outlier payment is the same as the approachused in the current system.50
Agenda1. Current HH PPS8. Comorbidity Group2. Overview of the PDGM9. Case-Mix Weights3. Measuring Period Costs10. Other Adjustments4. 30-Day Periods5. Admission Source and Timing11. Grouper Tool andExample Scenarios**6. Clinical Groups12. Operational Changes7. Functional Impairment Levels** indicates section to follow51
Example Grouper Tool Interactive Grouper tool for learning about the PDGM. Obtain the resulting HIPPS code and case mix weight by entering informationon a patient’s 30-day period for each PDGM category Purpose of this tool is informational and illustrative only –final CMS grouper software available in 2020Download Updated PDGM Grouper Tool CY 2019 11 6 18.xlsxDisclaimer:All scenarios are for illustrative purposes and assumption is that these beneficiaries meet all criteria for home health services.52
Example Scenario 1 – Timing and Admission SourceMr. Smith was newly diagnosed by his primary care physician with type 2 diabeteswith hyperglycemia (E11.65). Mr. Smith’s doctor made a home health referral fordiabetic management teaching, medication review and evaluation of complianceand response to new medications. Mr. Smith also has a documented history ofchronic, systolic (congestive) heart failure (I50.22), cerebral atherosclerosis (I67.2),and benign prostatic hypertrophy (N40.0)Select Timing and Admission Source of the 30-periodDisclaimer:All scenarios are for illustrative purposes and assumption is that these beneficiaries meet all criteria for home health services.53
Example Scenario 1 – Clinical GroupingMr. Smith was newly diagnosed by his primary care physician with type 2 diabeteswith hyperglycemia (E11.65). Mr. Smith’s doctor made a home health referral fordiabetic management teaching, medication review and evaluation of complianceand response to new medications. Mr. Smith also has a documented history ofchronic, systolic (congestive) heart failure (I50.22), cerebral atherosclerosis (I67.2),and benign prostatic hypertrophy (N40.0)Input E11.65 for primary diagnosisDisclaimer: All scenarios are for illustrative purposes and assumption is that these beneficiaries meet all criteria for home health services.54
Example Scenario 1 – Comorbidity AdjustmentMr. Smith was newly diagnosed by his primary care physician with type 2 diabeteswith hyperglycemia (E11.65). Mr. Smith’s doctor made a home health referral fordiabetic management teaching, medication review and evaluation of complianceand response to new medications. Mr. Smith also has a documented history ofchronic, systolic (congestive) heart failure (I50.22), cerebral atherosclerosis (I67.2),and benign prostatic hypertrophy (N40.0)Input I50.22, I67.2, N40.0 for secondary diagnoses55
Example Scenario 1 – Functional Points, Part 1 of 2The HHA completed the initial OASIS assessment: M1033 Risk of Hospitalization: Responses 4-7 (two or more emergencydepartment visits in 6 months; decline in mental, emotional or behavioral statusin the past 3 months; reported or observed history of d
Clinical: whether the patient has one or more clinical conditions such as incontinence; intravenous infusion (IV), enteral, or parenteral therapies; the