Transcription
Wellcare By Allwell2022 Provider OrientationSHP 20218310Confidential and Proprietary Information
Agenda Plan OverviewKey Resources for ProvidersMembershipBenefits and Additional ServicesBenefit OverviewHMO SNP Benefit OverviewMedical Home & Prior AuthorizationsPreventive Care and Screening TestMedicare Star RatingsWeb-Based ToolsNetwork PartnersConfidential and Proprietary Information Billing Overview Electronic Funds Transfer and ElectronicRemittance Advice Meaningful Use - Electronic MedicalRecords Advance Directives Regulatory Information Fraud, Waste and Abuse CMS Mandatory Trainings Model of Care Questions and Answers
Plan OverviewConfidential and Proprietary Information
Meet Wellcare By Allwell Welcome to the new Wellcare By Allwell! While you may have known us as Allwell before, we’ve combined multiplenational Medicare brands under the Wellcare name to offer a better range ofplans that provide members with affordable access to doctors, nurses, andspecialists We believe this change will make things easier for members, brokers, andproviders like you Our goal remains the same: ensuring your patients receive the best careConfidential and Proprietary Information
Who We Are Wellcare is a Medicare Advantage plan We provide quality healthcare you'dexpect from a big company, but deliveredon a local level That means our members benefit fromstrategic care coordination and programsthrough the strong and collaborativerelationships we build with healthcareproviders and community organizationsConfidential and Proprietary Information
Who We AreWellcare By Allwell is designed togive members: Affordable healthcare coverage Benefits they need to take good careof themselves Access to doctors, nurses andspecialists who work together to helpthem feel their best Coverage for prescription drugs Extra benefits that aren’t covered byMedicare Part A or Part B (OriginalMedicare)Confidential and Proprietary Information
Our Whole Health Approach Wellcare By Allwell provides complete continuity of care to Medicare members. This includes: Integrated coordination careCare managementCo-location of behavioral health expertiseIntegration of pharmaceutical services with the Pharmacy Benefits Manager (PBM)Additional services specific to the beneficiary needs Superior’s approach to care management facilitates the integration of community resources, healtheducation and disease management. Wellcare By Allwell promotes members’ access to care through a multidisciplinary team, including registerednurses, social workers, pharmacy technicians and behavioral health case managers, all co-located in a single,locally based unit.Confidential and Proprietary Information
Medicare 101Medicare is a federal health insurance program for people 65 years of age and older(under 65 with qualifying disabilities). It is made up of the following parts:Part AHospitalInsuranceMedicalInsurancePart BThis portion pays forhospital stays, skillednursing facilities andhospice stays.This pays for doctors’services both inpatientand outpatient as well aslab services, medicalequipment and supplies.Confidential and Proprietary InformationPart CMedicareInsuranceRxCoveragePart DMedicare Advantage planssuch as HMO’s and PPO’s.MA plans cover the sameservices as traditionalMedicare and may offerprescription drug coverage(Part D), dental, vision andhearing care.This pays for prescriptiondrugs for home use.
Medicare 101 – Election PeriodAnnual Election Period (AEP)Special Election Periods (SEP)October 15 – December 7Dates vary;Rules are based on the specific SEPAdd, drop, or change Medicare Advantageand/or Prescription Drug Plan (PDP) coverage.Plan changes are effective January 1of the following year.InitialEnrollmentAdd or change a Medicare Advantage plan orPDP (strictly controlled)Examples: Special Needs Plan (SNP) eligibilityMedicaid or Extra Help eligibilityA move out of a plan’s service areaLoss of group insurance3 months beforeyour birth monthConfidential and Proprietary Information3 months afteryour birth month65th birthday month
Wellcare By Allwell Medicare (HMO) Superior offers non-dual HMO plans. These HMO plans cover all Medicare-required services,along with a prescription drug benefit. HMO plans (unlike HMO SNP and MMP) do not requireMedicaid to enroll. Most Medicare plans (sometimes referred to as "Part C") include the Part D prescription drug benefitplan. This is Superior’s Wellcare By Allwell Medicare (HMO) plan. HMO plans cover the most commonly prescribed drugs. However, each specific Part D plan maydetermine which drugs are covered. The covered drugs are included in the plan’s formulary, or list ofdrugs: lary.htmlConfidential and Proprietary Information
Wellcare By Allwell Dual Medicare (HMO SNP) Wellcare By Allwell Dual Medicare (HMO SNP) is a plan for individuals with specific conditions or financialneeds who are eligible for both Medicare and medical assistance from Texas Medicaid. For HMO SNP members, Medicare is always the primary payor and Medicaid is secondary payor. HMO SNP members may have both Superior Medicare and Superior Medicaid but not always, so it isimportant to verify coverage prior to servicing the member.Please note: You may see members with Superior Medicare where their Medicaid is under another health plan or traditionalFee-For-Service (FFS) Medicaid or vice versa.Confidential and Proprietary Information
Key Resources for ProvidersConfidential and Proprietary Information
Key comConfidential and Proprietary Information
Getting AcquaintedDuring onboarding, you will receive a provider toolkit. Our toolkit contains useful information for getting started as anWellcare By Allwell provider.While we’ll cover some of that information in this presentation, your toolkit has additional information including: Welcome Letter Secure Portal Setup Electronic Funds Transfer Setup Prior Authorization Guide Quick Reference Guide Provider Office Window DecalConfidential and Proprietary Information
The Provider Manual The Provider Manual is your comprehensive guide to doing business with Wellcare By Allwell The Manual includes a wide array of important information relevant to providers including, but not limited to: Network information Billing guidelines Claims information Regulatory information Key contact list Quality initiatives And much more! The Provider Manual can be found in the Provider section of the Wellcare By Allwell website ining-manuals.htmlConfidential and Proprietary Information
Provider Services Our Provider Services Department includestrained Provider Relations staff who are availableto respond quickly and efficiently to all providerinquiries or requests including, but not limitedto:- Credentialing/Network status- Claims- Request for adding/deleting physicians to anexisting group By calling Provider Services at 1-877-391-5921providers will be able to access real timeassistance for all their service needsConfidential and Proprietary Information
AccountManagement As a Wellcare By Allwell provider,you will have a dedicated ProviderNetwork Specialist available toassist you Our Provider Network Specialistsserve as the primary liaisonsbetween our health plan andprovider network Your Provider Network Specialist ishere to help with things like:Confidential and Proprietary Information Inquiries related to administrativepolicies, procedures, and operationalissues Contract clarification Membership/provider roster questions Secure Portal registration and Pay Span Provider education HEDIS/Care gap reviews Financial analysis EHR Utilization Demographic information updates Initiate credentialing of a new practitioner
MembershipConfidential and Proprietary Information
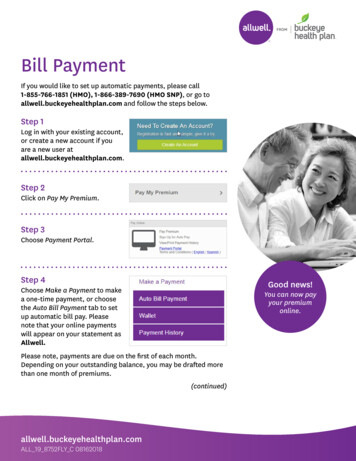
Membership Medicare beneficiaries have the option to stay in the original Fee-For-Service Medicare plan orchoose a Medicare Advantage Plan, such as Wellcare By Allwell from Superior HealthPlan. Wellcare By Allwell members may change Primary Care Providers (PCPs) at any time. Changestake effect on the first day of the month. Providers should verify eligibility before every visit by using one of the options below:– Secure Provider Portal: Provider.SuperiorHealthPlan.com– 24/7 Interactive Voice Response Line: 1-800-218-7453– Provider Services: HMO and HMO SNP – 1-877-391-5921Confidential and Proprietary Information
Member ID CardConfidential and Proprietary Information
Benefits and AdditionalServicesConfidential and Proprietary Information
Plan CoverageWellcare By Allwell covers: All Part A and Part B benefits by Medicare. Part B drugs – such as chemotherapy drugs. Part D drugs – no deductible at network retail pharmacies or mail order* Additional benefits and services such as:̶ Dental̶ Vision̶ No Cost/Low Cost PCP copay*̶ 0 generic prescription drugs For a summary of plan benefits, visit: als.html*Dependent on planConfidential and Proprietary Information
Pharmacy Formulary The Wellcare By Allwell formulary is available at ary.html. Please refer to the formulary for specific types of exceptions. When requesting a formulary exception, a Drug Coverage Redetermination form must besubmitted. These forms can be found under the ‘Redeterminations’ section of the CoverageDeterminations and Redeterminations for Drugs webpage: age-determinations-redeterminations.html The completed form can be faxed to Envolve Pharmacy Solutions at1-866-226-1093.Confidential and Proprietary Information
Covered Services Covered Services include, but are not limited to:̶̶AmbulanceBehavioral HealthHospital Inpatient/OutpatientLab and X-RayMedical Equipment and SuppliesPhysician̶̶̶*Specific counties only.Confidential and Proprietary Information̶̶̶̶̶PodiatryPrescribed MedicinesTherapyWellness Programs24-Hour Nurse Advice Line
Additional Services Multi-language Interpreter ServicesInterpreter services are available at no cost to Wellcare By Allwell members and providers withoutunreasonable delay at all medical points of contact. To get an interpreter, call member services at: HMO: 1-844-796-6811 (TTY: 711)̶ HMO SNP: 1-877-935-8023 (TTY: 711) Non-Emergency Transportation̶̶̶Covered for a specified number (dependent upon the member’s service area) of one-way trips peryear, to approved locations.Schedule trips 48 hours in advance using the plan’s contracted providers.Contact us at 1-877-718-4201 to schedule non-emergency transportation.Confidential and Proprietary Information
Network HCA/MethodistTexas TechUniversity Hospital –Bexar, El PasoEl Paso Medical NetworkChristus Santa Rosa HealthDoctors Hospital at Renaissance (DHR)Mission HealthBaptist health SystemSouthwest General HospitalTexas Health Resources (THR)Confidential and Proprietary Information
Benefit OverviewConfidential and Proprietary Information
Supplemental Benefits at a Glance OTC PERS Utilities Flex Card Helper Bee’s Care Concierge Grocery Card by Shipt Telemedicine Transportation Dental Vision Hearing Fitness Meals*Benefit levels vary by plan/service areaConfidential and Proprietary Information
Medical Home & PriorAuthorizationConfidential and Proprietary Information
Primary Care Providers (PCPs) PCPs serve as a medical home and provide the following:– Sufficient facilities and personnel.– Covered services as needed. 24-hours a day, 365 days a year.– Coordination of medical services and specialist referrals.– After-hours accessibility using one of the following methods: Answering service. Call center system connecting to a live person. Recording directing member to a covering practitioner. Live individual who will contact a PCP.Confidential and Proprietary Information
Interdisciplinary Care Team The purpose of the Interdisciplinary Care Team (ICT) is to collaborate with the member, theirproviders/specialists and other health-care professionals to ensure appropriate services are inplace, and to identify alternative solutions to barriers identified in a member's care plan. Superior’s program is member-centric with the PCP being the primary ICT point of contact.Superior staff works with all members of the ICT in coordinating the plan of care for the member.Confidential and Proprietary Information
Interdisciplinary Care Team As part of the ICT process, providers are responsible for: Accepting invitations to attend member’s ICT. Maintaining copies of the Individualized Care Plan (ICP), ICT worksheets and transition of carenotifications in the member’s medical record. Collaborating and actively communicating with care managers the ICT, members and caregivers. Superior Care Managers (CMs) work with the member to encourage self-management of theircondition, as well as communicate the member’s progress toward these goals to the othermembers of the ICT.Confidential and Proprietary Information
Interdisciplinary Care Team The ICT will be led by a Care Coordinator, and at aminimum is comprised of the following coremembers: Member and/or authorized representative. PCP. Family and/or caregiver, if approved by the member. Care coordinator(s) (Service Coordinator [SC],Behavioral Health CM). Specialist if serving as member’s PCP.Confidential and Proprietary Information
Responsibility of the Interdisciplinary Care Team Analyze and incorporate the results of the initial and annual health risk assessment into the individualizedcare plan. Coordinate the medical, cognitive, psychosocial and functional needs of members. The development and implementation of ICP with the member’s participation, as feasible. Conduct ICT meetings according to the member’s condition; these meetings may be held face to face, viaconference call, or web- based interface.Confidential and Proprietary Information
Utilization Management Authorization must be obtained prior to the delivery of certain elective and scheduled services.The preferred method for submitting authorization requests is through the Secure ProviderPortal at Provider.SuperiorHealthPlan.com.Confidential and Proprietary Information
Prior Authorizations Prior authorization is required for: Inpatient admissions, including observationHome health servicesAncillary servicesRadiology (MRI, MRA, PET, CT)Pain management programsOutpatient therapy and rehab (OT, PT, ST)TransplantsSurgeriesDurable Medical Equipment (DME)Part B drugsConfidential and Proprietary Information
Prior Authorizations for Covid-19COVID-19 Testing, Screening and Vaccinations Prior authorization requirements will be waived for COVID-19 testing, screening and vaccinationservices at this time Member cost share liability (copayments, coinsurance and/or deductible cost share amounts) willalso be waived for these servicesConfidential and Proprietary Information
Prior Authorizations for Covid-19COVID-19 Treatment Related Services COVID-19 treatment related services (those billed with a confirmed ICD-10 diagnosis code) willcontinue to be eligible for coverage at this time, in accordance with the member’s plan benefits Prior authorization is required for COVID-19 treatment related services in accordance with CMSguidance and plan benefits Providers should also collect Medicare member liability at the point of service for applicabletreatment related servicesConfidential and Proprietary Information
Prior Authorizations for Covid-19Telehealth Services Any services that can be delivered virtually will continue to be eligible for telehealth coverage atthis time Any prior authorization requirements that apply to in-office services will also apply to thoseservices when delivered via telehealth Providers should collect Medicare member liability at the point of service for applicabletelehealth services, in accordance with the member’s plan benefits Providers should reflect telehealth care on their claim form by following standard telehealthbilling protocols in their state.Confidential and Proprietary Information
Out-of-Network Coverage Plan authorization is required for out-of-network services, except:– Emergency care.– Urgently needed care when the network provider is not available (usually due to out-ofarea).– Kidney dialysis at Medicare-certified dialysis center when temporarily out of the servicearea.Confidential and Proprietary Information
Medical Necessity Determination When medical necessity cannot be established, a peer-to-peer review is offered. Denial letters will be sent to the member and provider. The clinical basis for the denial will be indicated. Member appeal rights will be fully explained.Confidential and Proprietary Information
Preventive Care andScreening TestConfidential and Proprietary Information
Preventive Care No copay for all preventive services covered under original Medicare at zero cost-sharing. Initial Preventive Physical Exam – Welcome to Medicare: Measurement of height, weight, body mass index, blood pressure, visual acuity screen and otherroutine measurements. Also includes an electrocardiogram, education and counseling. Does not includelab tests. Limited to one per lifetime. Annual Wellness Visit Available to members after the member has the one-time initial preventive physical exam (Welcome toMedicare Physical).Confidential and Proprietary Information
Preventive Care Abdominal Aortic Aneurysm Screening Flexible Sigmoidoscopy Alcohol Misuse Counseling HIV Screening Blood Pressure Screening Medical Nutrition Therapy Services BMI, Functional Status Medication Review Bone Mass Measurement Obesity Screening and Counseling Breast Cancer Screening (mammogram) Pain Assessment Cardiovascular Disease (behavioral therapy) Prostate Cancer Screenings (PSA) Cardiovascular Screenings Cervical and Vaginal Cancer ScreeningsSexually Transmitted Infections Screening andCounseling Colonoscopy Colorectal Cancer ScreeningsTobacco Use Cessation Counseling (counseling forpeople with no sign of tobacco-related disease) Depression Screening Diabetes ScreeningsVaccines, Including Flu Shots, Hepatitis B Shots,Pneumococcal Shots Fecal Occult Blood TestConfidential and Proprietary Information
MedicareStar RatingsConfidential and Proprietary Information
Medicare Star Ratings What are Centers for Medicare and Medicaid Services (CMS) Star Ratings? CMS uses a five-star quality rating system to measure Medicare beneficiaries’ experience with theirhealth plans and the health-care system. This rating system applies to Allwell plans that cover bothhealth services and prescription drugs (Allwell Medicare [HMO] and Allwell Dual Medicare [HMO SNP]). The ratings are posted on the CMS consumer website, www.Medicare.gov, to give beneficiaries help inchoosing a plan offered in their area. The Star Rating System is designed to promote improvement inquality and recognize primary care providers for demonstrating an increase in performance measuresover a defined period of time.Confidential and Proprietary Information
Medicare Star Ratings CMS’ Star Rating Program is based on measures in 9 different areas:Part C:1. Staying healthy: screenings,tests and vaccines.2. Managing chronic (long-term)conditions.3. Member experience with thehealth plan.4. Member complaints, problems.getting services andimprovement in the healthplan’s performance5. Health plan customer service.Confidential and Proprietary InformationPart D:1. Drug plan customer service.2. Member complaints and changesin the drug plan’s performance.3. Member experience with the drugplan.4. Drug safety and accuracy of drugpricing.
How Can Providers ImproveStar Ratings? Continue to encourage patients to obtain preventive screenings annually or when recommended. Manage chronic conditions, such as hypertension and diabetes, including medication adherence. Continue to talk to patients and document interventions regarding topics such as fall prevention,bladder control and the importance of physical activity and emotional health and wellbeing(HOS). Create office practices to identify noncompliant patients at the time of their appointment. Identify opportunities to have an impact on patient health and well-being.Confidential and Proprietary Information
How Can Providers ImproveStar Ratings? Submit complete and correct encounters/claims with appropriate codes and properly documentmedical charts for all members, including availability of medical records for chart abstractions. Review the gap in care files that list members with open gaps. These are available on Superior’sSecure Provider Portal. Review medication and follow up with members within 14 days post hospitalization. Make appointments available to patients and reduce wait times (CAHPS). Follow up with patients regarding their test results (CAHPS).Confidential and Proprietary Information
Web-Based ToolsConfidential and Proprietary Information
Superior Website Through www.SuperiorHealthPlan.com, providers can access:–Billing Manuals–Forms–HEDIS Quick Reference Guide–Provider News–Pre-Auth Needed Tool–Provider ResourcesConfidential and Proprietary Information
Superior Secure Provider Portal On Superior’s Secure Provider Portal (Provider.SuperiorHealthPlan.com), providers can access:– Authorizations– Claims Download Payment HistoryProcessing StatusSubmission / AdjustmentsClean Claim Connection – Claim Auditing Software– Health Records Care Gaps*– Patient Listings* and Member Eligibility*Available for PCPs only.Confidential and Proprietary Information
Primary Care Provider Reports Patient List – Located on Provider.SuperiorHealthPlan.com. Includes member’s name, ID number, date of birth and telephone number. The Patient List is available todownload to Excel or PDF formats and includes additional information such as member’s effective date,termination date, product, gender and address.Confidential and Proprietary Information
Updating Your Data Providers can improve member access to care by ensuring that their data is current in our providerdirectory. To update your provider data:1.Log in to the Secure Provider Portal2.From the main tool bar, select “Account Details”3.Select the provider whose data you want to update4.Choose the appropriate service location5.Make appropriate edits and saveConfidential and Proprietary Information
PCP Cost Reports Members with Frequent ER visits: This report includes members who frequently visit the ER on a monthlybasis. The report is available in Excel and PDF formats, and provides member information, paid (ER) providerinformation, claim number, procedure information, diagnosis and cost. High Cost Claims: This report includes members with high-cost claims. The report is available in Excel andPDF formats, and provides detailed member information, provider information, claim number, procedureinformation, diagnosis and cost. Rx Claims Report: This report includes members with pharmacy claims on a monthly basis. The report isavailable in Excel and PDF formats, provides detailed member information, provider information, detailedprescription information (such as pharmacy, units, days refill, etc.) and cost.Confidential and Proprietary Information
Network PartnersConfidential and Proprietary Information
Partners and VendorsServiceSpecialty Company/VendorContact InformationHigh Tech Imaging ServicesNational Imaging l PainManagementNational Imaging Associates1-866-214-2569www.radmd.comVision ServicesEnvolve Vision alth.comDental ServicesEnvolve Dental Benefitswww.dental.envolvehealth.comPharmacy ServicesEnvolve Pharmacy Solutions1-866-399-0928 (Phone)1-866-399-0929 (Fax)Hearing AidsHearing Care mConfidential and Proprietary Information
Partners and VendorsServiceSpecialty Company/VendorContact InformationFitness ServicesASHwww.silverandfit.comMealsVendor ServicesGA Foods & Mom’s -575-2772www.GAFoods.comOTC careLegacy Allwell:https://www.cvs.com/otchs/allwellPERS portation ServicesModivCare1-877-718-4201Confidential and Proprietary Information
TurningPoint HealthCare Solutions Superior HealthPlan started working with TurningPoint Healthcare Solutions, LLC to launch a new Surgical Quality andSafety Management Program. TurningPoint is responsible for processing prior authorizations requests for medical necessity and appropriate length ofstay for Musculoskeletal Surgical procedures. In addition, Superior has expanded the partnership with TurningPoint HealthCare Solutions to process prior authorizationrequests for medical necessity and appropriate length of stay for certain Cardiac procedures, Ear, Nose and Throat (ENT)surgeries and sleep study procedures. TurningPoint’s Procedure Coding and Medical Policy Information can be located under Billing Resources tml.Confidential and Proprietary Information
TurningPoint HealthCare Solutions Prior authorization is required for the following Musculoskeletal surgical procedures in both inpatient andoutpatient settings*:*This is not an all-inclusive list. For a detailed list of impacted CPT codes, visit TurningPoint’s Web Portal ck.html.Confidential and Proprietary Information
TurningPoint Healthcare Solutions –Cardiac Surgical Procedures Prior authorization is required for the following Cardiac surgical procedures in both inpatient andoutpatient settings: Arterial ProceduresLoop RecordersCoronary Angioplasty/StentingNon-coronary Angioplasty/StentingCoronary Artery Bypass GraftingPacemakerImplantable Cardioverter Defibrillator (ICD)Pacemaker Revision or RemovalICD Revision or RemovalValve ReplacementLeft Atrial Appendage OccludersWearable Cardiac DefibrillatorConfidential and Proprietary Information
TurningPoint Healthcare Solutions –ENT Surgery and Sleep Study Prior authorization is required for the following ENT surgeries and sleep studiesperformed in the inpatient, outpatient, physician’s office and in-home settings.Sleep Study ProceduresActigraphyHome Sleep StudyMultiple Sleep Latency and Maintenance ofWakefulness TestingPolysomnographyENT SurgeriesBalloon Dilation EsophagoscopyCochlear Implant DeviceLaryngoscopy and LaryngoplastyRhinoplasty and SeptoplastySinus SurgeryThyroidectomy and ParathyroidectomyTonsillectomy (with or without Adenoidectomy)Tympanostomy and TympanoplastyConfidential and Proprietary Information
TurningPoint Healthcare Solutions Emergency related procedures do not require authorization. It is the responsibility of the ordering physician to obtain authorization. Providers rendering the above services should verify that the necessary authorization has been obtained.Failure to do so may result in non-payment of claims. Authorization requirements for facility and radiology may also be applicable. For questions regarding this notification, prior authorization requirements, or impacted CPT codes, pleasecontact TurningPoint: Email: providersupport@turningpoint-healthcare.com Phone: TurningPoint Provider Support: 1-866-422-0800. Intake: 1-855-336-4391Confidential and Proprietary Information
Lab and DME PartnersLab PartnersBio ReferenceSequenome CenterMD LabsLab CorpQuestConfidential and Proprietary InformationDME PartnersAmerican Home PatientApriaBregCCS MedicalCritical Signal TechnologiesDJOEBIEdge ParkJ&B MedicalKCILincareHanger Prosthetics and OrthoticsNational Seating & MobilityNextra Health
AcariaHealth - Specialty Pharmacy AcariaHealth is a national, comprehensive specialty pharmacy providing services in all specialty diseasestates including:‒Cystic Fibrisis‒Hemophilia‒Hepatitis C‒Multiple Sclerosis‒Oncology‒Rheumatoid ArthritisMost biopharmaceuticals and injectables require prior authorization at:‒CustomerCare@acariahealth.comConfidential and Proprietary Information
Billing OverviewConfidential and Proprietary Information
Electronic Claims Transmission and Support 6 clearinghouses for Electronic Data Interchange (EDI) submission:‒ Payer ID: 68069‒ Faster processing turn around time than paper submission. Companion guides for EDI billing requirements and loop segments can be found atwww.SuperiorHealthPlan.com. For more information, email EDIBA@centene.com.Confidential and Proprietary Information
Claims Filing Timelines Allwell claims should be mailed to the following billing address:– Allwell from Superior HealthPlanAttn: ClaimsP.O. Box 3060Farmington, MO 63640-3822 Participating providers have 95 days from the date of service to submit a timely claim. All requests for reconsideration or claim disputes must be received within 120 days from lasttimely processed claim.Confidential and Proprietary Information
Claims Payment A clean claim is received in a nationally accepted format in compliance with standard coding guidelines,and requires no further information, adjustment or alteration for payment. A claim will be paid or denied with an Explanation of Payment (EOP) mailed to the provider who submittedthe original claim. Providers may not bill members for services when the provider fails to obtain authorization and the claim isdenied. Dual-eligible members are protected by law from balance billing for Medicare Parts A and B services. Thisincludes deductibles, co-insurance and co
̶24-Hour Nurse Advice Line . Texas Tech University Hospital -Bexar, El Paso El Paso Medical Network Christus Santa Rosa Health . Recording directing member to a covering practitioner. Live individual who will contact a PCP. Confidential and Proprietary Information