Transcription
A Guide to theNutritional Assessmentand Treatment of theCritically Ill Patient2nd Ed.Mark S. Siobal, BS, RRT, FAARCJami E. Baltz, MS, RD-AP, CNSCJodi Wright, RD, CNSCCopyright 2021 by the American Association for Respiratory Care
Table of ContentsExecutive Summary. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4Nutritional Overview . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7Nutritional Assessment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9Malnutrition. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16Nutritional Support . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19Determining Nutritional Requirement . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29Clinical Practice Recommendations For Nutritional Support . . . . . . . . . . . . . . . . . . . . . . . . . . 39Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45Acronyms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 512A Guide to the Nutritional Assessment and Treatment of the Critically Ill Patient, 2nd Ed.
ForewordThe American Association for Respiratory Care (AARC) is excitedto release its second edition of the Guide to the NutritionalAssessment and Treatment of the Critically Ill Patient. The goalof this guide is to assist respiratory therapists at the bedside asthey provide a higher level of assessment and management topatients. Since its original introduction in 2014, the content inthis guide has positively impacted the critical care communityand we are pleased to provide updated information to continueto promote positive patient outcomes.Proper nutritional assessment and treatment is essential to thesuccessful management of critically ill patients. Unfortunately,these patients are often malnourished - especially those whorequire mechanical ventilation. Malnutrition can lengthen thetime spent in the ICU and extend hospital length of stay. Forthe mechanically ventilated patient, it can delay or impede theweaning process - which adds another level of associated risks.All disciplines play an important role in managing the nutritionalneeds of the critically ill patient. All bedside clinicians have anobligation to ensure that critically ill patients are assessed fornutritional adequacy and intervention is taken when required.This guide reviews the process of nutritional assessment andmanagement of the adult critically ill patient, but also discussesspecific patient populations where malnutrition is more prevalent.We hope that you find this guide helpful as you manage yourpatients’ pulmonary and nutritional needs.Shawna Strickland, PhD, CAE, RRT, RRT-NPS, RRT-ACCS, AE-C, FAARCAssociate Executive DirectorAmerican Association for Respiratory Care3A Guide to the Nutritional Assessment and Treatment of the Critically Ill Patient, 2nd Ed.
Executive SummaryIntroductionNutritional Risk and AssessmentThe purpose of this guide is to provide an overview of theimportant considerations regarding nutritional assessment andtreatment that the health care team must address to ensurepatients are provided with appropriate nutritional support. Thegoal of this work is to review a broad list of topics that covers thenutritional support and care process to provide the health careteam with a broad understanding of the nutrition assessment andtreatment process for the hospitalized critically ill patient.Assessment of nutritional status is performed to identify patientsat higher risk for malnutrition related complications. Patients withmoderate or severe malnutrition are likely to have longer ICUand hospital length of stay and higher risk of death. After theinitial assessment, the primary goals of nutritional support areto maintain lean body mass in at-risk patients and to providecontinuous evaluation of the nutrition care plan. Minimized risk ofmalnutrition can be achieved by prompt initiation of nutritionalsupport, proper targeting of appropriate nutrient quantities, andpromotion of motility through the gastrointestinal tract.A registered dietitian or other trained clinician gathersinformation to examine the patient’s nutrition related historyand physical findings, anthropometric physical measurements,biochemical data, and medical tests and procedures, and thenscreens the patient for other nutrition associated conditions suchas malnutrition, obesity, and the risk of refeeding syndrome.OverviewAppropriate nutrition is essential for improving outcomes inthe health care environment. Hospitalized patients have highrates of malnutrition. Unmet nutritional needs and malnutritionlead to increased morbidity and mortality, decreased quality oflife, prolonged duration of mechanical ventilation, and increasedlength of hospital stay, all of which contribute to the highercost of health care. Critically ill patients and those patients withrespiratory failure require special attention to prevent musclewasting and to avoid overfeeding and complications associatedwith nutritional care. A functional nutrition support systemshould include an interdisciplinary team approach for assessmentand treatment, which incorporates an evaluation of nutritionalrisk, standards for nutritional support, an appropriate assessmentand reassessment process, proper implementation, route ofsupport based on patient condition, and a means of measuringnutrient requirements to determine if target goals are being met.Interdisciplinary ApproachThe Society of Critical Care Medicine (SCCM) recognizes thevalue and importance of a multidisciplinary team approach tonutritional care as a means to improve clinical outcomes. Eachdiscipline in an intensivist led interdisciplinary team, whichincludes dietitians, nurses, pharmacists, respiratory therapists,speech pathologists, and physical therapists, can contribute toimproved outcomes and reduced health care costs.Route of Nutritional SupportEnteral nutrition (EN) is the preferred route of nutritionalsupport. EN should be started within the first 24– 48 hours afteradmission in patients who are incapable of volitional intake.Gastric or small bowel feeding is acceptable in the ICU setting.Enteral feeding tube placement in the small bowel should bedone in patients at high risk for aspiration or whose intoleranceto gastric feeding is demonstrated. Holding enteral feeding forhigh gastric residual volumes (GRV) in the absence of clear signsof intolerance and demonstrated risk of aspiration may resultin an inappropriate cessation of EN and cause a calorie deficitover time. The definition for high GRV should be determined byindividual institutional protocol; but use of GRV up to 500 mL hasnot been shown to increase the risks of regurgitation, aspiration,or pneumonia in adult patients.The decision to initiate parenteral nutrition (PN) is influencedby the patient’s nutritional risk, clinical diagnosis and condition,gastrointestinal tract function, and duration of anticipated need.PN in a previously healthy patient should be considered when ENis not feasible for the first 7 – 10 days after hospital admission.Patients with evidence of moderate to severe malnutrition where4A Guide to the Nutritional Assessment and Treatment of the Critically Ill Patient, 2nd Ed.
EN is not an option should receive PN within the first few daysfollowing admission. Supplemental PN may be considered in adultand pediatric patients when nutritional requirements cannot beachieved with EN within the first weekNutritional Considerations During Critical IllnessThe general goals of nutritional care in all patients, includingthose with respiratory disorders and critical illness, are to provideadequate calories to support metabolic demands, to preservelean body mass, and to prevent muscle wasting.Nutritional support during critical illness attenuates themetabolic response to stress, prevents oxidative cellular injury,and modulates the immune system. The stress response tocritical illness causes wide fluctuation in metabolic rate. Thehypercatabolic phase can last for 7–10 days and is manifestedby an increase in oxygen demands, cardiac output, and carbondioxide production. Caloric needs may be increased by up to 100%during this phase. The goal is to provide ongoing monitoring andsupport with high protein feedings while avoiding overfeedingand underfeeding. Nutritional modulation of the stress responseincludes early EN, appropriate macro- and micronutrient delivery,and glycemic control.Determination of Nutritional RequirementsNutrient requirements can be calculated by over 200 differentequations. Predictive equations use traditional factors for age,sex, height, weight, and additional factors for temperature, bodysurface area, diagnosis, and ventilation parameters. Additionaldata such as injury- stress, activity, medications received, andobesity have been added to improve accuracy. Several predictiveequations were developed with a focus on specific patientpopulations and medical conditions.Predictive equations have varying degrees of accuracy. Errorrates can be significant and result in under- and overestimationof caloric needs that impact outcomes. Some equations areunsuitable for use in critically ill patients, while others have beenvalidated with improved accuracy. Due to the extreme metabolicchanges that can occur during critical illness, energy needsshould be measured using indirect calorimetry (IC) in patientsnot responding to nutritional support, have complex medicalconditions, and are ventilator dependent.Indirect calorimetry relies on accurate determination of oxygenconsumption (VO2) and carbon dioxide production (VCO2) usinga metabolic analyzer for precise measurements of inspired andexpired fractions of oxygen and carbon dioxide. The abbreviatedWeir equation uses the measured VO2 and VCO2 to determineresting energy expenditure (REE). The respiratory quotient (RQ),the ratio of VCO2 to VO2, can then be calculated. The RQ was oncethought to be a means to determine nutritional substrate use, butthis assumption has never been substantiated and use of the RQmeasurement is of limited clinical value. Measured values of RQbetween the physiologic ranges of 0.67–1.3 should be used asa way to validate test quality. Values of RQ outside of this rangeinvalidate the results due to technical measurement errors andshould be repeated.When a metabolic analyzer is unavailable, IC using othermethods should be considered as an alternative to the utilizationand dependence on predictive equations.Clinical Practice RecommendationsSeveral clinical practice guidelines are available to guidenutritional support. The SCCM and the American Society ofParenteral and Enteral Nutrition (ASPEN), the European Societyfor Clinical Nutrition and Metabolism (ESPEN), the Academy ofNutrition and Dietetics (AND), the Canadian Clinical PracticeGuidelines for Nutritional Support (CCPG), and the EuropeanSociety of Pediatric and Neonatal Intensive Care (ESPNIC)have developed best practice recommendations based on theinterpretation of available evidence, consensus agreement, andexpert opinion.The following present summaries of some of the bestpractice recommendations for adult patients from the variousorganizations: Nutritional support should be initiated early, within thefirst 24–48 hours in critically ill patients. Primary goals of nutritional support and care are to:preserve and maintain lean muscle mass; providecontinuous assessment, reassessment, and modificationto optimize outcome; monitor the patient for toleranceand complications such as refeeding syndrome; preventprotein energy malnutrition by giving higher proteincontent while providing adequate total calories; monitornutrition goals and target achievement rate of 65%within the first week; and prevent accumulation of acaloric deficit. Indirect calorimetry should be used when available orwhen predictive equations are known to be inaccurate. Current EN practice recommendations are to:preferentially feed via the enteral route; initiate ENwithin 24–48 hours; reduce interruptions of EN for5A Guide to the Nutritional Assessment and Treatment of the Critically Ill Patient, 2nd Ed.
nursing care and bedside procedures to preventunderfeeding; maintain head of bed (HOB) elevation toreduce aspiration risk; avoid routine monitoring of GRV oraccept GRV up to 500 mL before reducing or stopping ENin the absence of clear signs of intolerance; use motilityagents to improve tolerance; and promote post-pyloricfeeding tube placement when feasible. Current PN practice recommendations are to: only useexclusive PN when enteral route is not feasible; use PNbased on the patient’s nutritional risk classification formalnutrition; delay PN up to seven days in low nutritionalrisk patients; initiate PN early in high nutritional riskpatients; consider use of supplemental PN whenindicated; convert to EN as soon as tolerated to reducethe risks associated with PN. Use of trophic or “trickle feeding” and permissiveunderfeeding may be beneficial. Use of pharmaconutrients and immunonutrition: utilizehigh omega-3 fatty acid to omega-6 fatty acid ratios. Theuse of arginine, glutamine, nucleotides, antioxidants,and probiotics may be beneficial in specific patients. Theuse of arginine should be avoided in patients with severesepsis.When EN is unable to be initiated in the first week ofadmission, PN may be provided.Appropriate nutritional support in hospitalized patients and theprevention of malnutrition can improve outcomes and reducehealth care costs. The nutritional care plan should utilize theteam approach and be supported by organizational standardswith policies and procedures that are based on the best availableevidence. The health care team’s proper implementation,continuous assessment, and monitoring of the nutrition care planare key elements for success. In pediatric patients: EN is the preferred route of nutrition. Initiate EN within 24-48 hours of admission to the PICU A stepwise algorithmic approach to advancing EN shouldbe utilized. Goal is to achieve at least 2/3 of nutrient goal within thefirst week of admission. IC should be utilized when available to determine energyrequirements. Routine measurement of GRV is not recommended Either gastric or post-pyloric feeding can be utilized inthe majority of children. Measurement of anthropometrics should be obtained onadmission and regularly throughout the hospital course. Immunonutrition is not recommended for the critically illchild. Timing for PN initiation should be individualized with thebelow general guidance: In cases of severe malnutrition, supplemental PN maybe provided in the first week of admission if unableto advance beyond low volumes of EN.6A Guide to the Nutritional Assessment and Treatment of the Critically Ill Patient, 2nd Ed.
Nutritional OverviewThe Importance of Appropriate NutritionAppropriate nutrition is essential for health and healing. Inhospitalized patients, malnutrition is a common and seriousproblem affecting both adult and pediatric populations.1-4Critically ill patients are at high risk for malnutrition relatedcomplications. The resulting detrimental effects of malnutritioninclude increased morbidity and mortality, decreased functionalquality of life, prolonged duration of mechanical ventilation, andincreased length of hospital stay, all which contribute to higherhealth care cost.5Critical illness associated with respiratory failure requiresspecial attention to prevent catabolic or destructive metabolism.6Nutritional therapy in this setting requires maintenance ofadequate calorie and protein intake to prevent muscle wastingand avoid overfeeding and complications associated withnutritional care.7 Malnutrition is a risk factor for the onset ofrespiratory failure and can worsen further after respiratory failureis established. Nutritional support can affect respiratory musclestrength, endurance and function, carbon dioxide production,and immune system response. To ensure successful supportand recovery from respiratory failure, the nutritional care planmust also consider other important aspects, such as fluid andelectrolyte balance, micronutrient requirements, and acid-basestatus. Recovery from respiratory failure requires a regimentednutritional support process that includes a comprehensiveassessment of risk, proper implementation, ongoing reassessmentof caloric requirements, tolerance of treatment monitoring, andavoiding the development of complications.6Importance of Interdisciplinary CollaborationThe role of health care team members in providing expertiseregarding nutritional support has evolved around interdisciplinarycollaboration. Registered dietitians and physicians completespecialized training programs to attain the Certified NutritionSupport Clinician (CNSC) credential and are increasingly involvedin nutrition support organizations such as the American Society ofParenteral and Enteral Nutrition (ASPEN).8Respiratory therapists have traditionally maintained theresponsibility and technical expertise in performing metabolicmeasurements by indirect calorimetry assessments, especially inthe mechanically ventilated critically ill patient. Clinical practiceguidelines developed by the American Association for RespiratoryCare (AARC) maintain an evidence-based framework for nutritionalassessments using indirect calorimetry for patients receivingmechanical ventilation.9Speech pathologists aid in the assessment of post-extubationdysphagia. Detection of swallowing dysfunction that is commonafter prolonged mechanical ventilation can help prevent thedetrimental impact and risks associated with aspiration andpoor nutrition among patients with or without neurologicdysfunction.10,11 Post-extubation dysphagia is associated withlonger hospitalization in survivors of critical illness with neurologicimpairment.Critical care organizations such as the Society of Critical CareMedicine (SCCM) recognize the importance of an intensivistled multidisciplinary team consisting of nurses, dietitians,pharmacists, respiratory therapists, and physical therapists.12Each discipline provides expertise pertinent to nutritional supportand care, contributes to improved outcomes, and reduces costs.The future and ongoing challenge to the evolution of healthcare is to facilitate the team approach toward best practicesand therapeutic efficacy. Appropriate nutritional assessment andtreatment protocols require devoted resources toward diagnosis,intervention, and monitoring. The integrated health care deliveryteam trained in nutritional assessment and treatment will bebetter equipped to optimize and ensure health care resourcesare maximized.13Importance of Adequate Nutritional Assessmentand TreatmentNutritional deficits related to chronic disease and acuteillnesses are frequently found in patients admitted to the ICU.Many patients who cannot resume oral food ingestion withinthe first few days of admission are prone to losing body massdue to poor nutrient intake and are at risk for developing anacute and prolonged inflammatory process. Patients in the ICUfor more than 48 hours need nutritional assessment and supportmaintained constantly throughout their period of critical illness7A Guide to the Nutritional Assessment and Treatment of the Critically Ill Patient, 2nd Ed.
Conditions Likely to Require Parenteral Nutrition* Impaired absorption or loss of nutrients Mechanical bowel obstruction Need to restrict oral or enteral intake: bowel rest Motility disorders Inability to achieve or maintain enteral accessPatient AssessmentNutrition Support IndicatedNOYESAny Condraindications toEnteral Nutrition?Enteral NutritionNOCompromised GIFunction?Standard FormulaParenteral NutritionYESDurationSpecial considerations Short Term No Central AccessSpecialized FormulaPeripheral PNFeeding ToleranceYESAdvance to OralFeeding WhenAble to Eat Safely Long Term Low volumeconcentrated PNNOYESSupplementationwith PNConsider OralFeedingCentral PNReturned GI Function?NOYESNOOral Intake indicated?YESFigure 1. Example of a Nutrition Management Protocol15and hospitalization. Many critically ill patients experience severegastrointestinal motility disorders and can experience dysphagiafollowing extubation, which may increase the risks for aspiration.Complications associated with critical illness can have seriousconsequences that can be diminished with early recognition andintervention. The promotion of effective nutrition can only beachieved with a standardized nutritional support protocol thatincorporates regular assessments of gastrointestinal function andtolerance of parenteral and enteral feeding.14In critically ill patients unable to take nutrition by mouth, enteralnutrition (EN) through the gastrointestinal tract is the preferredroute. Parenteral nutrition (PN) by intravenous access is anotheralternative. Use of an evidence-based nutritional managementprotocol increases the likelihood that patients receive nutrition viathe enteral route (Figure 1).A standardized approach targeting gastric or post-pyloricfeeding tube placement when indicated, gastric decompression,and use of bowel motility agents can shorten the duration ofmechanical ventilation and reduce the risk of death. Clinicaloutcome benefits from improving the rate of EN can besignificant when adjusted for nutritional risk of moderate-tosevere malnutrition at baseline.16Development and maintenance of a best-practice nutritionalsupport program reduces costs and improves outcomes.Maintenance of nutritional support requires continuous monitoringof the appropriate route of administration and the adequacy ofusage in order to minimize costs and reduce waste.17 Insufficientcalorie intake is associated with an increase in mortality risk. Thereasons for failure to achieve recommendations for best clinicalpractice include lack of sufficient nutritional support services tomonitor adherence, inadequate training in nutritional support,and restricted use of nutrient formulations that show improvedoutcomes secondary to their higher cost, or disagreement aboutthe supporting evidence.178A Guide to the Nutritional Assessment and Treatment of the Critically Ill Patient, 2nd Ed.
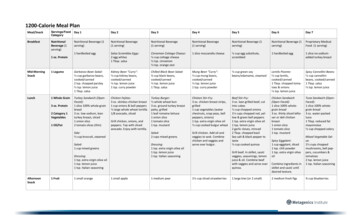
Nutritional AssessmentNutritional Risk AssessmentThe nutritional assessment process should begin at admissionwith a nutrition screening followed by a formal assessmentwhen indicated.18 This process can be automatically triggeredby electronic medical record (EMR) systems. Several nutritionscreening and assessment tools are available to evaluate therisks of malnutrition in hospitalized patients.19 Parameters thatare evaluated include BMI and weight loss, history of nutritionalintake, severity of illness, and anthropometric measurements(Figure 2). Recent guidelines based on expert consensus, suggestthe use of the Nutrition Risk Screening tool (NRS 2002) and theNutrition Risk in the Critically Ill assessment tool (NUTRIC score) inall patients admitted to the ICU when insufficient volitional intakeis anticipated.12 Patients with a high risk of malnutrition are morelikely to benefit from early initiation of EN.Nutrition risk assessment should encompass two necessaryelements. The initial assessment establishes the presence or(ii)BMI (kg/m2)1 5-10%1 18.5-20.02 10%2 18.5(iii)Nutritional support standards for acute care have beenHospital admissioneonargssichmidisadICUICUWeight loss in 3-6 months0 5%0 20.0Standards for Nutritional SupportAcute disease effectFunctional statuslean body mass(i)Additionally, the safe provision of nutritional support requires acontinuous evaluation of the risks of nutritional care. Minimizedrisk can be achieved by prompt initiation of nutrition, targetingthe appropriate nutrient quantities, promoting motility throughthe gastrointestinal tract, and averting serious life-threateningcomplications such as refeeding syndrome. Patients found tobe at higher risk for nutrition-related problems should receivespecialized nutritional support. Development of nutritionalassessment and care protocols designed for the specific needsof critically ill patients are required to minimize the reduction oflean body mass until discharge. Nutritional care from admission tohospital discharge is essential to reducing risk of nutrition relatedcomplications and promoting recovery (Figure 3).Hospital dischargeNormalLow riskNutritionModerate riskSeverelyimpairedNo nutrition careHigh riskTimeAdd a score of 2 if there hasbeen or is likely to be no ornutritional intake for 5 days.Figure 3. Time Course of Increasing Nutritional Risk Assessment andSupport in Critical Illness14OVERALL RISK OF UNDERNUTRITION0LOWRepeat screeningHospital - every weekCare Homes - every monthCommunity - every year forspecial groups, e.h. those 75 y1MEDIUM2 or moreHIGHHospital - document dietrary and fluidintake for 3 daysCare Homes - (as for hospital)Community - Repeat screening, e.g. from 1 mo to 6 mo (with dietary advice ifnecessary)Hospital - refer to dietitian orimplement local policies.Generally food first followed by foodfortification and supplementsCare Homes (as for hospital)Community (as for hospital)Figure 2. Malnutrition Universal Screening Tool (MUST) for Adults20estimate of lean body mass loss prior to ICU or hospital admission.The goal of preventing further loss of lean body mass canbe achieved when acute illness is promptly controlled andwith the formation of an adequate nutritional support process.developed to guide the nutrition support process. These standardsare designed to optimize the development and performance of acompetent nutritional care plan (Figure 4). Components of anutritional support program should include the following.18OrganizationA nutritional support service or interdisciplinary team approachwith established policies, procedures, and a performanceimprovement process should be initiated for each admitted patient.9A Guide to the Nutritional Assessment and Treatment of the Critically Ill Patient, 2nd Ed.
A.S.P.E.N. ADULTNUTRITION CARE PATHWAYCONTINUED FROM PREVIOUS PAGE(Age 18 years)SUSPECTED MALNUTRITION?YESGENERATENUTRITION CONSULTADMISSIONObtain actual, measuredheight/weight and BMI anddocument on admissionValidated screening tool completedVia EMR, automatic trigger ordocumented in MR Screen completed in 24 hours Results documented in EMRPhysician consult on admissionNOFOLLOW UP/RESCREENNUTRITION CARE PLAN AND INTERVENTIONMONITORING & EVALUATION[RD, NST, RN, MD/PA/NP, PharmD][RD, NST, RN, MD/PA/NP, PharmD, PT, OT]Nutrition care plan created & documented;goals identifiedInitiate order/identify type of nutritionsupport required Provide least restrictive, medically appropriate diet Determine need for nutritional supplementation Treatment of medical issues impactingnutrition intake and utilizationDetermine access needs for specialized nutritionsupport to maximize nutritional intake (Enteralfeeding tubes, IV access for PN) Review medications regarding impact onnutritional intakeCommunicate nutrition care plan with teammembers on multidisciplinary patient care roundsEducate patient/caregiver regarding plan of care.Follow-up within 3 daysMonitoring parameters Tolerance of nutrient intake Oral intake including supplements,vitamins, minerals Enteral/Parenteral intake Anthropometric data (weight trends) Biochemical data Functional status[RD, NST, DT, OR DESIGNEE]Every 3-7 days to preventhospital-acquired malnutritionBased on length of stayUpon transition of careNUTRITION ASSESSMENTREVISE NUTRITIONCARE PLANNO[RD, NST]Completed within 24 hours of consultFood and Nutrition HistoryAnthropometricsBiochemical data/Medical Tests& ProceduresNutrition Focused PhysicalExam (NFPE)Clinical and Medical History[RD, NST, PT, OT]NOMALNUTRITIONIDENTIFIED?AND/A.S.P.E.N. malnutritioncharacteristicsYESYESReassess every 3-5 daysBegin discharge planningCommunication StepsNFPE Nutrition FocusedPhysical ExamNST Nutrition SupportTeamMD Medical DoctorNP Nurse PractitionerPA Physician AssistantPharmD Pharmacist 2015 American Society for Parenteral and Enteral Nutrition. All rights reserved.MALNUTRITION DIAGNOSIS/RISKDOCUMENTEDKEYRN Registered NurseRD Registered DietitianDT Diet TechnicianAdequate nutrient intakeStable or increased weightStability of biochemical dataImproved strength and functionCONTINUE CURRENTNUTRITION CARE PLAN 2015 American Society for Parenteral and Enteral Nutrition. All rights reserved.Action StepsDocumentation StepsDOCUMENT PARAMETERS THATINDICATE IMPROVEMENT INNUTRITION STATUSKEY[RD, NST, RN, MD/NP/PA]CM Case ManagerOT Occupational TherapistPT Physical TherapistAND Academy of Nutritionand DieteticsA.S.P.E.N. AmericanSociety for Parenteral andEnteral NutritionPN Parenteral NutritionEN Enteral NutritionNPO/CLD Nothing byMouth/Clear Liquid DietEMR/MR ElectronicMedical Record or MedicalRecordBMI Body Mass IndexRD documents malnutrition risk statusRD documents supporting evidence ofmalnutrition severityMD documents malnutrition and severityin progress note and adds to problem listCODE MALNUTRITIONDIAGNOSISCoder notified of diagnosisAdult Malnutrition CodesAction StepsDocumentation StepsDISCHARGE PLAN[RD, RN, MD/PA/NP, PharmD, CM]Education / Counseling with patient and caregiversCommunication of PN, EN or Oral Nutrition Supplement prescriptionCase management for continuity of careOutpatient follow-up as ap
continuous evaluation of the nutrition care plan. Minimized risk of malnutrition can be achieved by prompt initiation of nutritional support, proper targeting of appropriate nutrient quantities, and promotion of motility through the gastrointestinal tract.