Transcription
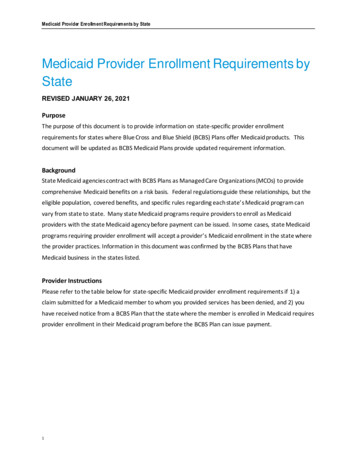
Medicaid Provider Enrollment Requirements by StateMedicaid Provider Enrollment Requirements byStateREVISED JANUARY 26, 2021PurposeThe purpose of this document is to provide information on state-specific provider enrollmentrequirements for states where Blue Cross and Blue Shield (BCBS) Plans offer Medicaid products. Thisdocument will be updated as BCBS Medicaid Plans provide updated requirement information.BackgroundState Medicaid agencies contract with BCBS Plans as Managed Care Organizations (MCOs) to providecomprehensive Medicaid benefits on a risk basis. Federal regulations guide these relationships, but theeligible population, covered benefits, and specific rules regarding each state’s Medicaid program canvary from state to state. Many state Medicaid programs require providers to enroll as Medicaidproviders with the state Medicaid agency before payment can be issued. In some cases, state Medicaidprograms requiring provider enrollment will accept a provider’s Medicaid enrollment in the state wherethe provider practices. Information in this document was confirmed by the BCBS Plans that haveMedicaid business in the states listed.Provider InstructionsPlease refer to the table below for state-specific Medicaid provider enrollment requirements if 1) aclaim submitted for a Medicaid member to whom you provided services has been denied, and 2) youhave received notice from a BCBS Plan that the state where the member is enrolled in Medicaid requiresprovider enrollment in their Medicaid program before the BCBS Plan can issue payment.1
Medicaid Provider Enrollment Requirements by StateStateBCBS PlanOut-of-StateEnrollmentRequirementOther StateMedicaidEnrollmentAccepted?Detail on Out-of-State EnrollmentRequirement LanguageLink to RequirementLink to StateProvider PageCaliforniaAnthem BlueCross ofCaliforniaYesNoRequirements:An out-of-state provider does needto register to bill the payer, howevera provider can directly bill a nonMedi-Cal eligible patient. .Reference toRequirements:Provider EnrollmentRegulationsLink to ProviderPage:Medicaid ProviderEnrollmentNot RequiredNot Applicable(Enrollment NotRequired)Requirements:The website does not address outof-state providers specifically andDelaware requirements are not welldefined for the MCOs.Highmark assumes that since it is notdefined, the state does not requireprovider enrollment.Requirements:Out-of-state provider enrollment isnot required.Reference toRequirements:State MedicaidProvider PortalLink to ProviderWebsite:Medicaid ProviderEnrollmentReference toRequirements:State MedicaidProvider PortalLink to ProviderPage:Medicaid ProviderEnrollmentRequirements:Enrollment is required for anyprovider submitting a claim for thestate of Illinois Medicaid Program.Reference toRequirements:IL ProviderRequirements.Link to ProviderPage:IL MedicaidProvider WebsiteDelawareBlue Shield ofCaliforniaHighmark BlueCross BlueShieldDelawareHawaiiHMSANot RequiredNot Applicable(Enrollment NotRequired)IllinoisBlue Cross andBlue Shield ofIllinoisYesYes, but also mustenroll withIlliniois.(Out-of-stateEnrollment is nota replacement)Blue shading indicates enrollment requirement.
Medicaid Provider Enrollment Requirements by State3StateBCBS PlanOut-of-StateEnrollmentRequirementOther StateMedicaidEnrollmentAccepted?Detail on Out-of-State EnrollmentRequirement LanguageLink to RequirementLink to StateProvider PageIndianaAnthem BlueCross and BlueShield IndianaYesNoRequirements:Enrollment is required for anyprovider submitting a claim for thestate of Indiana Medicaid Program.If the provider is not registered withthe state of Indiana, the encounterwill reject.Link to ProviderPage:Indiana MedicaidProvider WebsiteKentuckyAnthem BlueCross and BlueShieldKentuckyYesRequirementsProviders must have a KentuckyMedicaid ID in order to be paid.MichiganBlue Cross BlueShield ofMichiganYesYes, but also mustenroll withKentucky(Out-of-stateEnrollment is nota replacement)NoReferences toRequirements:Provider ReferenceModule: ProviderEnrollment (Section 2Provider Eligibilityand EnrollmentRequirements)Reference toRequirements:KY ProviderEnrollment WebsiteLink to ProviderPage:MI MedicaidProvider WebsiteMinnesotaBlue Cross andBlue Shield ofMinnesotaNoReferences toRequirements: MI ProviderManual (Section7.3) Provider BulletinReference toRequirements:MN ProviderEnrollment Website(Providers LocatedOutside of MinnesotaSection)Out-of-StateProvidersNot Applicable(Enrollment NotRequired)Requirements:All providers furnishing services toMichigan Medicaid beneficiaries willbe required to enroll through anonline portal as a requirement forreimbursement.Requirement:Providers who submit claims toMinnesota Medicaid Managed CareOrganization (including as BCBS ofMN) are required to enroll withMinnesota DHS.Link to ProviderPage:KY HFS ProviderWebsiteLink to ProviderPage:MHCP EnrolledProviders Website
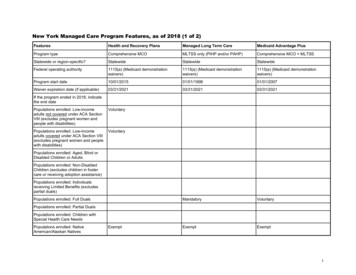
Medicaid Provider Enrollment Requirements by State4StateBCBS PlanOut-of-StateEnrollmentRequirementOther StateMedicaidEnrollmentAccepted?Detail on Out-of-State EnrollmentRequirement LanguageLink to RequirementLink to StateProvider PageNew JerseyHorizon BlueCross and BlueShieldYes, for certainservicesWhen required forcertain services:Yes, but also mustenroll with NewJersey. (Out-ofstate Enrollmentis not areplacement.)Requirements: New Jersey does not requireproviders to enroll/register withMedicaid prior to renderingservices or being reimbursed byMedicaid HMOs (such asHorizon BCBS). For carve out services (notusually covered by Medicaid)provided by any Fee-for-Serviceprovider submitting a claim tothe state of New JerseyMedicaid Program, enrollment isrequired.Reference toRequirements:New Jersey MedicaidAdministrationManual (Title 10Chapter 49Subchapter 3)Link to ProviderPage:New JerseyMedicaid ProviderPortalNew MexicoBlue Cross andBlue Shield ofNew MexicoYesYes, but also mustenroll with NewMexico.(Out-of-stateEnrollment is nota replacement)Requirements:Enrollment is required for anyprovider submitting a claim for thestate of New Mexico MedicaidProgram.Link to ProviderPage:New MexicoMedicaid ProviderPortalNew YorkHealthnowExcellus BlueCross BlueShieldNot RequiredNot Applicable(Enrollment NotRequired)Requirements:Enrollment in New York StateMedicaid is not required for out-ofstate professional or institutionalproviders to bill an MCO in New YorkState.Reference to StateMedicaid Page:NM MedicaidGeneral ProviderPolicies (Out-of-Stateand Border AreaProviders)Reference toRequirement:Link to providerManualLink to ProviderPage:eMedNY ProviderWebsite
Medicaid Provider Enrollment Requirements by StateStateBCBS PlanOut-of-StateEnrollmentRequirementOther StateMedicaidEnrollmentAccepted?Detail on Out-of-State EnrollmentRequirement LanguageLink to RequirementLink to StateProvider PagePennsylvaniaIndependenceBlue CrossYesYes, but also mustenroll with PARequirements:Out-of-State providers must enroll inPennsylvania’s Medicaid program,but must be enrolled first in theirhome state.Out-of-state practitioners must belicensed and currently registered bythe appropriate agency in their stateand they must providedocumentation that they participatein that state's Medicaid program.The Plan’s Prior Authorization lineoperators will be trained to insistthat out of area providers enroll.Requirements:Triple-S Salud (Puerto Rico) does notrequire providers to enroll/registerwith Medicaid prior to renderingservices or being reimbursed byMedicaid. Reimbursement based onlocal Medicaid Coverage.Requirements:For services other than emergencythat require prior authorization, theout-of-state provider must confirm,in writing, that he or she will enrollin the South Carolina Medicaidprogram and will accept Medicaidreimbursement as payment in full.Reference k to ProviderPage:PennsylvaniaProvider WebsiteReference to PuertoRico Medicaid Page:Puerto Rico MedicaidLink to ProviderPage:Provider PortalWebsiteReference toRequirements:Provider EnrollmentInformationLink to ProviderPage:HealthyConnectionsMedicaid ProviderInformation(Out-of-stateEnrollment is nota replacement)Puerto RicoTriple SSouth Carolina Blue Cross andBlue Shield ofSouth Carolina5Not required.Not applicable(Enrollment NotRequired)Yes – for servicesother thanemergency thathave priorauthorization.No
Medicaid Provider Enrollment Requirements by StateStateBCBS PlanOut-of-StateEnrollmentRequirementOther StateMedicaidEnrollmentAccepted?Detail on Out-of-State EnrollmentRequirement LanguageLink to RequirementLink to StateProvider PageTennesseeBlue Cross BlueShield ofTennesseeYesNoRequirements:New TennCare/ Medicaid providersneed to register.References toRequirement:Provider RegistrationLink to ProviderPage:TennCare ProvidersTexasBlue Cross andBlue Shield ofTexasYesYes, but also mustenroll with TXSTAR Program.Requirements:Enrollment is required for anyprovider submitting a claim for thestate of Texas Medicaid ProgramReference toRequirement:Texas MedicaidProvider ProceduresManual (Volume ISection 1)Link to Billing, Rendering, and AttendingProviders need to be registered onthe master file with the state.For physicians that operate out-ofstate (more than 50 miles from theVA border) you will also need toattest to enrollment in your residentstate Medicaid program.Requirement:Out-of-state providers who do notmeet the requirements for borderstate enrollment may be reimbursedfor non-emergency services providedto a Wisconsin medical assistancerecipient through a priorauthorization, under Wisconsin statelaw DHS 107.04.Reference toRequirement:Provider EnrollmentTutorialLink to ProviderPage:DMAS ProviderServicesDMAS ProviderResourcesReference toRequirement:Wisconsin StateLegislature Rule forOut-of-StateProvidersLink to ProviderPage:Forward HealthProvider LinksVirginiaWisconsin6Anthem BlueCross and BlueShield VirginiaYesAnthem BlueCross and BlueShieldWisconsinNot Required(Out-of-stateEnrollment is nota replacement)YesEnrollment instate MedicaidProgram whereprovider practicesis also required.Not Applicable(Enrollment NotRequired)
Medicaid Provider Enrollment Requirements by State7
TennCare Providers Texas Blue Cross and Blue Shield of Texas Yes Yes, but also must enroll with TX STAR Program. (Out-of-state Enrollment is not a replacement) Requirements: Enrollment is required for any provider submitting a c