Transcription
MEDICAID PROVIDER ENROLLMENTMARCH 2019Michael Cimmino, CMSTechnical Advisor, Division of Enrollment Operations
Poll QuestionCMS National Provider Enrollment Conference March 201902/20/2019 2
What is Medicaid?CMS National Provider Enrollment Conference March 201902/20/2019 3
Medicare vs. MedicaidMedicareFederal Health Care CoverageCMS National Provider Enrollment Conference March 2019MedicaidCooperative Federal and StateHealth Care Coverage02/20/2019 4
Medicare vs. Medicaid Medicare and Medicaid are separate programs Submitting an application to Medicare does notmean you have also submitting an application toMedicaid An enrollment approval in Medicare does notnecessarily guarantee enrollment approval inMedicaidCMS National Provider Enrollment Conference March 201902/20/2019 5
What is CMS’ role?CMS National Provider Enrollment Conference March 201902/20/2019 6
Medicaid Provider EnrollmentCMS Center for Program Integrity managesMedicare and Medicaid enrollment. CMS provides oversight while States administer theMedicaid program CMS issues Federal regulations and sub-regulatoryguidance that states must adhere to in implementingtheir Medicaid program CMS provides technical assistance to states via phone,email, and in-person visitsCMS National Provider Enrollment Conference March 201902/20/2019 7
Medicaid Provider Enrollment Requirements CMS promulgated requirements via regulations at42 CFR: 455 Subpart B (Disclosures) 455 Subpart E (Screening and Enrollment) The federal regulations became effective March 25,2011 (except FCBC) These requirements mirror those implemented inMedicare—with a few exceptionsCMS National Provider Enrollment Conference March 201902/20/2019 8
Sub-Regulatory GuidanceMedicaid.gov contains all provider enrollment relatedMedicaid guidance issued to states: index.htmlMost importantly, the Medicaid Provider EnrollmentCompendium (MPEC): https://www.medicaid.gov/affordable-care- act/downloads/program-integrity/mpec-7242018.pdf Updated July 24, 2018Guidance is for State Medicaid Agencies andprovidersCMS National Provider Enrollment Conference March 201902/20/2019 9
State-Based RequirementsCMS National Provider Enrollment Conference March 201902/20/2019 10
Poll QuestionCMS National Provider Enrollment Conference March 201902/20/2019 11
State RequirementsCMS does not prohibit states from implementing their ownprovider standards and requirementsMPEC: “Under § 455.452, nothing in Subpart E restricts a SMAfrom establishing provider screening methods in addition to ormore stringent than those required by Subpart E.” Conduct required screening in a more stringent manner thanMedicare or another State conducts the same required screening Conduct additional screening activities Impose additional requirements on providersCMS National Provider Enrollment Conference March 201902/20/2019 12
Risk Level and ScreeningFCBCHighSite VisitsModerate & HighLimited, Moderate, & High1. Check Federal or state requirements by provider type2. Licensure Checks3. Database ChecksCMS National Provider Enrollment Conference March 201902/20/2019 13
Medicaid-Medicare Differences Medicaid has a 5 year revalidation requirement for Suppliers ofDurable Medical Equipment and Supplies Fingerprinting for Medicaid “high” risk providers required as ofJuly 1, 2018 Risk categories for Medicaid-only provider types may differ other provider types will have similar risk level as Medicare States have the authority to raise (but not lower) the riskcategory for any provider type Criteria to elevate risk levelCMS National Provider Enrollment Conference March 201902/20/2019 14
How does this impact youand what to expect?CMS National Provider Enrollment Conference March 201902/20/2019 15
Application Fees States are authorized to charge applicationfees on a per application basis If a state requires providers to submit an application for eachpractice location, the state may charge a fee for each of thoseapplications Some states may permit all locations to be enrolledusing one application States may charge fees of provider types that Medicare doesnotCMS National Provider Enrollment Conference March 201902/20/2019 16
Application Fees Medicaid* cannot charge an application fee when the provider isenrolled with Medicare or another State’s Medicaid program The provider must be the igh”TINPracticeLocation(s)5 % or moreownersXXXXXXXXXXX*Medicare will charge the fee regardless of enrollment with MedicaidCMS National Provider Enrollment Conference March 201902/20/2019 17
Site Visits Site visits may differ between states and with Medicare’s sitevisit criteria/protocol Some states use site visits not only to confirm the practicelocation but also compliance with other state policies andrequirementsExamples:One state uses site visits to verify the location is wheelchairaccessibleVerification that employed staff have required CPRcertificationsCMS National Provider Enrollment Conference March 201902/20/2019 18
Fingerprinting States, like Medicare, must fingerprint all 5% or greater ownersof providers categorized as “high” risk States may categorize provider types at higher risk levels thanMedicare Some states may choose to fingerprint allowners, at least one state fingerprints managingemployeesCMS National Provider Enrollment Conference March 201902/20/2019 19
“High” Risk Providers Prospective (newly enrolling): Home health agencies (HHA) DMEPOS Provider types the State has categorized as “high” Providers elevated per 42 CFR 455.450(e)CMS National Provider Enrollment Conference March 201902/20/2019 20
Increase in Risk Level CMS has designated specific criteria for states to use indetermining when a provider may need to have their risk levelincreased to “high” from “limited” or “moderate” This criteria is different between Medicare and Medicaid While you may be categorized as “limited” or “moderate” riskin Medicare, you may be “high” risk in Medicaid The state would be required to conduct “high” risk screeningCMS National Provider Enrollment Conference March 201902/20/2019 21
Criteria to Increase Risk LevelProviders Are “High” Risk When:Risk Remains “High”State imposes a payment suspensionon a provider based on credibleallegation of fraud, waste or abuse inthe past 10 yearsProvider has an existing Medicaidoverpayment* at initial enrollment orrevalidation10 years beyond date ofpayment suspensionFor any enrollment orrevalidation that theprovider continues to havean existing overpayment**Overpayment Criteria on next slideCMS National Provider Enrollment Conference March 201902/20/2019 22
Criteria to Increase Risk LevelAn overpayment that meets the criteria to bump a provider to“high” risk is 1500 or greater and all of the following: Is more than 30 days old Has not been repaid at the time the application was filed Is not currently being appealed Is not part of a SMA-approved extended repayment schedulefor the entire outstanding overpaymentCMS National Provider Enrollment Conference March 201902/20/2019 23
Criteria to Increase Risk LevelProviders Are “High” Risk When:Risk Remains “High”Provider has been excluded by the OIG oranother State's Medicaid program withinpast 10 yearsState or CMS, in the previous 6 months,lifted a moratorium for the particularprovider type anda provider that was prevented from enrollingapplies for enrollment within 6 months fromthe date the moratorium was lifted.For 10 years beyonddate of exclusionCMS National Provider Enrollment Conference March 2019State stops lookingat this beginning 6months and 1 dayafter a moratoriumis lifted02/20/2019 24
What If I am or will be aDually Enrolled Provider?CMS National Provider Enrollment Conference March 201902/20/2019 25
Poll QuestionCMS National Provider Enrollment Conference March 201902/20/2019 26
Relying on Medicare’s ScreeningStates may, but are not required to, relyon the results of screening performed byMedicare or its contractors CMS has designed the framework for when states can andcannot rely on Medicare’s screening for dually enrolledproviders More detailed guidance on the following is available in theMPECCMS National Provider Enrollment Conference March 201902/20/2019 27
Relying on Medicare’s ScreeningA state is able to fully rely on Medicare’s screening when: The provider has been screened in the past 5 years The provider is “approved” in Medicare The provider is the same risk level in both Medicare andMedicaid The provider is verified as the “same” providerCMS National Provider Enrollment Conference March 201902/20/2019 28
Relying on Medicare’s ScreeningWhat is the “same” provider?Risk CategorySSNAll 5%PracticeName NPI (Last 4 TINor moreLocation(s)digits)owners“Limited” IndividualXXX“Moderate” IndividualXXXX“High” Individual“Limited” OrganizationXXXXX“Moderate” OrganizationXXXX“High” OrganizationXXXXCMS National Provider Enrollment Conference March 2019XX02/20/2019 29
Relying on Medicare’s Screening If information submitted on Medicaid application does notalign with Medicare, the state may not be able to fully rely onMedicare’s screening States may choose to perform their own screening and onlyrely party on Medicare’s screening Enrollment with Medicare does not exempt providers fromdisclosing information requested on Medicaid application There may be instances when States can only partially rely onMedicare’s screeningCMS National Provider Enrollment Conference March 201902/20/2019 30
Partially Relying on Medicare’s ScreeningExample: State receives Medicaid application that lists three 5% orgreater owners. Upon checking PECOS the state only sees one 5%or greater owner.Next Steps: The state has two options:1. Perform screening on the two additional owners andenroll2. Reach out to CMS to see if a CHOW is pending; awaitCHOW approval to enroll In either case, States are asked to provide these discrepancies toCMS—could result is possible revocation or impact to applicationCMS National Provider Enrollment Conference March 201902/20/2019 31
What if I’m enrolled inanother state’s MedicaidProgram?CMS National Provider Enrollment Conference March 201902/20/2019 32
Relying on Another StateSimilar concept as relying onMedicare If a provider was screened and enrolled by another state, anysubsequent states may rely on that screening Relying is optional The same data elements used for relying on Medicare’sscreening would need to be confirmed and matched betweentwo statesCMS National Provider Enrollment Conference March 201902/20/2019 33
What if I don’t directlyparticipate with Medicaid?CMS National Provider Enrollment Conference March 201902/20/2019 34
Poll QuestionCMS National Provider Enrollment Conference March 201902/20/2019 35
Ordering and ReferringIs enrollment of the O/R provider required?ServiceDMEPOSMedicareAll ItemsMedicaidAll ItemsHome Health Services All ServicesAll ServicesClinical Lab ServicesTechnical ComponentOnly* Unless BilledGloballyBoth Technical andProfessionalComponentsImaging ServicesTechnical ComponentOnly* Unless BilledGloballyBoth Technical andProfessionalComponents*Provider performing the professional component must beenrolled in order to be reimbursed but O/R provider doesnotCMS National Provider Enrollment Conference March 201902/20/2019 36
MedicareMedicare Patientvisits non-enrolled Dr.and the Dr. orders anX-rayPatient visitsMedicare enrolledImaging provider andX-ray is takenX-ray is read byMedicare enrolledRadiologistImaging providerbills Medicare fortechnicalcomponentRadiologist billsMedicare forprofessionalcomponentMedicare deniesclaim for technicalcomponent becausethe Ordering provideris not enrolled oropted out ofMedicareCMS National Provider Enrollment Conference March 2019Medicare pays claimfor professionalcomponent only02/20/2019 37
MedicaidMedicaid Patientvisits non-enrolled Dr.and the Dr. orders anX-rayPatient visitsMedicaid enrolledImaging provider andX-ray is takenX-ray is read byMedicaid enrolledRadiologistImaging providerbills Medicaid fortechnicalcomponentRadiologist billsMedicaid forprofessionalcomponentMedicaid denies claimfor technicalcomponent becausethe Ordering provideris not MedicaidenrolledCMS National Provider Enrollment Conference March 2019Medicaid denies claimfor professionalcomponent becauseOrdering provider isnot Medicaid enrolled02/20/2019 38
Ordering, Referring, and Prescribing States are required to enroll all ordering, referring, andprescribing providers Unlike Medicare, this requirement applies to all items andservices due to statutory language drafted by Congress This is typically accomplished via a claims edit which will denyany claim with an unenrolled provider’s NPI The NPI for the ordering, referring, prescribing provider mustalmost always be a Type 1 individual NPICMS National Provider Enrollment Conference March 201902/20/2019 39
Ordering, Referring, and Prescribing Providers do not have the option of“opting out” in Medicaid as it is notpermitted by Medicaid regulations Some states offer a streamlined enrollment approach Ordering, referring, prescribing only Crossover claims are also subject to this requirement—someproviders may need to enroll with Medicaid in order for adually eligible beneficiary to receive their Medicaid benefitCMS National Provider Enrollment Conference March 201902/20/2019 40
Managed Care Network Providers Medicaid Managed Care “In-Network” providers must bescreened and enrolled with the state If your status is “in-network” with a Medicaid Managed Care planyou must execute a provider agreement with the state Your provider agreement with the plan will not fill thisrequirement Some states have allowed MCOs to screen providers Screening must be consistent with ACA requirementsCMS National Provider Enrollment Conference March 201902/20/2019 41
Managed Care Network Providers Once again, providers do not have the ability to “opt out” The use of a Preclusion List approach is not permitted inMedicaid Some states have created an “MCO-only” provider type andseparate enrollment processCMS is not aware of any states that requireparticipation or acceptance of Medicaid patientsbecause you have enrolled with their programCMS National Provider Enrollment Conference March 201902/20/2019 42
How might a Medicaidtermination impact you?CMS National Provider Enrollment Conference March 201902/20/2019 43
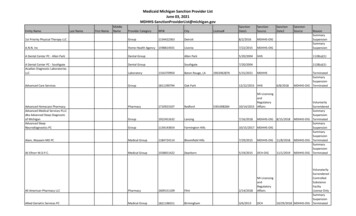
Terminations States are required to report terminated providers toCMS This does not include providers who voluntarilyterminate their enrollment If a provider is terminated from any state, CMS hasthe discretion to revoke the provider from Medicare A provider who is first revoked from Medicare, mustbe terminated from all state Medicaid programsCMS National Provider Enrollment Conference March 201902/20/2019 44
Other Key DifferencesCMS National Provider Enrollment Conference March 201902/20/2019 45
State-only Moratoria States have the authority to implement a state-based(Medicaid only) moratoria Requires CMS initial approval and re-approval every sixmonths CMS requires states to conduct a thorough access tocare analysis States are also required to provide strong reasoning asto the need for the moratoriaCMS National Provider Enrollment Conference March 201902/20/2019 46
Enrollment Effective Dates States have the authority to backdate an enrollmenteffective date but are not required to do so In most cases, states can backdate to the Medicarecertification date but not to exceed one year States have the authority to set their own backdatingpolicies Some states will not backdate while others may onlygo as far back as six monthsCMS National Provider Enrollment Conference March 201902/20/2019 47
Contacting the State Most states include on their website a contact orgeneral inquiry box for enrollment related inquiries If you do not have a method for contacting aparticular state, CMS can facilitate and have the statereach out to youCMS National Provider Enrollment Conference March 201902/20/2019 48
Questions?March 2019 This summary material was part of an in-person presentation. It was current atthe time we presented it. It does not grant rights or impose obligations. We encourage you toreview statutes, regulations, and other directions for details.If you need more accessibility options for the material, contact providerenrollment@cms.hhs.govCenters for Medicare & Medicaid ServicesCMS National Provider Enrollment Conference March 201902/20/2019 49
MEDICAID PROVIDER ENROLLMENT MARCH 2019. Michael Cimmino, CMS. Technical Ad