Transcription
Informational MemoProvider Action:Revalidation of Enrollment RequiredforAll Service LocationsODP Communication Number: Memo 041-14The mission of the Office of Developmental Programs is to support Pennsylvanians with developmentaldisabilities to achieve greater independence, choice and opportunity in their lives.AUDIENCE:Medical Assistance (MA) Providers who have an enrolled service location(s) inthe Provider Reimbursement and Operations Management System (PROMISeTM)with the Office of Developmental Program’s (ODP) Provider Eligibility Programs(PEPs) attached to their enrollment profile. This communication applies to Baseproviders, Consolidated and/or Person/Family Directed Support (P/FDS) waiverproviders. Note: All ODP providers are considered Medical Assistanceproviders1.PURPOSE:This ODP informational memo is intended to provide clarification regardingprovider revalidation (re-enrollment) specified in MA Bulletin # 99-14-06. Thisnew requirement is a result of the Affordable Care Act (ACA).Intermediate Care Facilities should contact the Office of Long Term Living (OLTL) Provider Call Center forinquiries regarding revalidation. The call center can be reached by phone at 1-800-932-0939. Theirhours of operation are Monday – Thursday, 9 AM - 12 PM and 1 PM - 4 PM.BACKGROUNDThe Patient Protection and Affordable Care Act (PPACA) 2010 HR3590, or Affordable Care Act(ACA) for short, is the health care reform law in America. The Patient Protection and AffordableCare Act consist of the Affordable Health Care for America Act, the Patient Protection Act, and1By completing and signing the "DPW, OMAP, Provider Agreement for Outpatient Providers", ODP Providers agree toparticipate in the Pennsylvania Medical Assistance Program and comply with the terms of the agreement.ISSUE DATE: 6/20/2014ODP Communication Number: Memo 041-14page 1 of 7
the health care related sections of the Health Care and Education Reconciliation Act and theStudent Aid and Fiscal Responsibility Act. It also includes amendments to other laws like theFood, Drug and Cosmetics Act and the Health and Public Services Act. Since being signed intolaw, additional rules and regulations have expanded upon the law.On March 7, 2014, the Office of Medical Assistance (OMAP) issued Bulletin # 99-14-06 titled“Re-enrollment/Revalidation of Medical Assistance (MA) Providers”. This bulletin was a resultof the Affordable Care Act (ACA) amending Section 1902 of the Social Security Act whichrequires States to comply with provider screening requirements. All providers must re-enroll,also referred to as revalidation, their enrollment information for each individual servicelocation enrolled in PROMISeTM. This applies to all active service locations in PROMISeTM.NOTE: Providers of P/FDS and Consolidated waiver services will not receive payment for servicelocation codes that are end dated and closed in PROMISeTM. When a Base only providersubmits claims for an end dated and closed service location(s) in PROMISeTM, thoseclaims will be denied and show as denied on their remittance advices.DISCUSSIONIn response to MA Bulletin # 99-14-06, ODP has received many inquiries related to revalidationof enrollment for MA Providers. Throughout this communication the term “revalidation” willbe used but keep in mind that “re-enrollment” has the same meaning. This communication willaddress the most frequently asked questions regarding revalidation.What is the purpose of revalidating enrollment?The purpose of revalidation is not only to comply with the Federal Regulation 42 CFR 455.414 but it is alsoto ensure State provider enrollment systems contain valid active provider enrollment data.Why is the revalidation deadline March 24, 2016 and how do I determine what the revalidation datesare for each of my service locations?The March 24, 2016 deadline is used because the Federal regulation at 42 CFR 455.414 requires States,beginning March 25, 2011, to complete revalidation of enrollment for all providers, regardless of providertype, at least every five years. After initial revalidation is complete for every service location, therevalidation requirement will continue to apply to every active service location every five years. The March24, 2016 deadline is somewhat misleading so the following examples should provide clarification on how aprovider’s revalidation date is determined: If a provider’s service location was enrolled before March 25, 2011 and is currently still active in thesystem, the system will show a revalidation date of March 24, 2016. All providers who enrolledbefore March 25, 2011 have a revalidation date in PROMISeTM of March 24, 2016. Provider servicelocations that fall into this category have until March 24, 2016 to have their revalidation finalized inthe system.ISSUE DATE: 6/20/2014ODP Communication Number: Memo 041-14page 2 of 7
If a provider’s service location was enrolled on March 25, 2011 or forward their revalidation datewould be the original enrollment date plus five years.The following are examples to demonstrate how a provider’s service location revalidation date iscalculated:Service Location Enrollment DateBefore March 25, 2011March 25, 2011 or afterJune 29, 2011August 29, 2012September 5, 2013Revalidation Date in SystemMarch 24, 2016Add 5 years to enrollment dateJune 29, 2016August 29, 2017September 5, 2018What would ODP recommend to enrolled providers as first steps?Step 1: Providers should review all their service locations currently enrolled in PROMISeTM and HCSIS anddetermine if all the service locations present should all continue to remain active. To view the provider’s service locations in PROMISeTM, providers should login to ePEAP (ProviderEnrollment Automation Project). To access ePEAP, go to the PROMISe Internet Portal and login.Next, click the “ePEAP (Provider Enrollment Automation Project)” link, located in the “Other Links”box. A listing of the sites and associated provider types will be displayed based on the provider IDused to log into ePEAP. To view service locations in HCSIS, log in HCSIS go to Provider Access and click “View My ApplicationSummary” located on the left sidebar of the screen. A listing of all sites with the provider type andspecialty code designations will be displayed.Step 2: Service locations should be identical in both HCSIS and PROMISeTM. If a provider is closing aservice location in PROMISeTM then the provider should ensure the service location is also closed (enddated) in HCSIS. To close a service location in PROMISeTM that should no longer be active, providers should completethe PROMISe Service Location Change Request form. The completed and signed form should beforwarded to ODP using one of the three methods below.Email: RA-odpproviderenroll@pa.govFax:717-783-5141 Attn: Provider EnrollmentMail: Office of Developmental Programs – IDAttn: Provider EnrollmentRoom 413 Health and Welfare BuildingHarrisburg, PA 17101 To close a service location in HCSIS, please refer to the “HCSIS Provider Updates Tip Sheet” whichcan be found in LMS and on the Provider Access home page on the left hand side under Job Aids.ISSUE DATE: 6/20/2014ODP Communication Number: Memo 041-14page 3 of 7
Step 3: For service locations that have been determined to remain open/active, providers should reviewthe revalidation date in the system. This information should be on the same screen in ePEAP as the sitesand provider types.Step 4: Ensure the revalidation process for each service location is finalized by the revalidation date thatappears in the system. The business process to revalidate is the same as the new provider enrollmentapplication process.To perform revalidation, Providers should complete a PROMISeTM Provider Enrollment Base Application foreach site of service (service location). The enrollment application is located on the Department of PublicWelfare’s (DPW) PROMISe provider enrollment website. Click the following hyperlink to visit thiswebsite: mentinformation/index.htmOnce you reach the “Enrollment Information” screen of the DPW PROMISe provider enrollment website,scroll down until you find your provider type. Click on the “Enrollment Application/Provider Agreement”hyperlink located to the right of the provider type. On page 5 of the application, the section called “2.Action Request. Check Boxes That Apply” has been modified to include the option to select “Revalidation”.Completed applications along with all required documentation and change request forms, if applicable, canbe remitted to ODP one of three ways:Email: RA-odpproviderenroll@pa.govFax:717-783-5141Mail: Office of Developmental Programs – IDAttn: Provider Enrollment - RevalidationRoom 413 Health and Welfare BuildingHarrisburg, PA 17101If you have not already done so, please plan on submitting your provider application well in advance of therevalidation date found in the system to allow for sufficient processing time.NOTE: ODP has a four (4) week timeframe to review applications before submitting them to the Office ofMedical Assistance Programs (OMAP). OMAP takes approximately 16 weeks to finalize enrollmentapplications in the provider enrollment system. It is strongly recommended that providers submitrevalidation applications at least 20 weeks in advance of their revalidation due date in order to assureOMAP has time to process the application prior to the revalidation due date and to avoid the automaticexpiration of the service location code.Is revalidation required for each enrolled service location?Yes. Revalidation is required for each enrolled service location.ISSUE DATE: 6/20/2014ODP Communication Number: Memo 041-14page 4 of 7
Is ODP currently accepting applications for revalidation?Yes. ODP is currently accepting revalidation applications.Why do my service locations have different revalidation due dates?If service locations were enrolled in PROMISeTM at different times, then they will have different revalidation duedates in the system. However, providers are permitted to begin submitting “PROMISeTM Provider EnrollmentBase Applications” for revalidation now and all at once for every active service location found in PROMISeTMeven if the service locations show different due dates in the system. By submitting all service locationenrollment applications all at once, the service locations will all have the same re-enrollment date for every fiveyear revalidation cycle.Providers can view their provider types and revalidation dates associated with each of their service locations inPROMISe through ePEAP (Provider Enrollment Automation Project). To access ePEAP, go to the PROMISeInternet Portal. Next, click the “ePEAP (Provider Enrollment Automation Project)” link, located in the “OtherLinks” box. A listing of the sites and associated provider types will be displayed based on the provider ID used tolog into ePEAP. Once in the provider portal, the revalidation date will be displayed on the top area of the screenfor each service location. This is also the current expiration date for that service location for that servicelocation based on the most recent application on file with DPW.Providers will need to complete a full new enrollment application per provider type for each service location.Once a completed application is submitted, ODP and OMAP will conduct the required screening.For more detailed instructions on how to view provider type and service location enrollment information,please reference pages 5‐7 of the ePEAP Manual. The link to the ePEAP webpage is: ePEAP Manual WebpageHow often do a provider’s service location(s) need to be revalidated?When a provider submits a “PROMISeTM Provider Enrollment Base Application” for revalidation, the nextrevalidation date is typically five (5) years from the effective date found on the revalidation base enrollmentapplication. The effective date of the Provider Enrollment Profiles (PEPs) assigned to the service location andthe specialty codes listed on the revalidation base enrollment application will always be the same date as theenrollment effective date. However, if ODP determines during the revalidation base enrollment applicationreview process that either the qualification effective date or effective dates associated with licensingrequirements2 are different than what is found on the revalidation enrollment base application, the enrollmentdate and the effective dates for the PEPs and specialties in PROMISeTM will be adjusted to align with thequalification and licensing dates.Note: ODP employs the same review process during revalidation as is done for an initial enrollment. See thefollowing examples on the next page for further clarification.2This applies to Providers with sites licensed or may be licensed under 55 Pa Code § 2380, 2390, 6400, and 6500 regulations and providerssubject to 55 Pa Code § 5310, 3800 regulations. See the Health-Related Boards on the Pennsylvania Department of State website for licensingregulations related to nursing, therapy and psychology. See the PA Department of Health website for home health licensure information.ISSUE DATE: 6/20/2014ODP Communication Number: Memo 041-14page 5 of 7
Effective Date onPROMISeTMBase EnrollmentRevalidationApplicationEntered by tionDate Date forPreviouslyQualifiedService4/15/2014Effective Date entered byODP Enrollment UnitUsing Date Found OnPROMISeTM BaseEnrollmentRevalidation evalidationDate InPROMISeTM4/6/20194/15/20194/1/20196/15/2019What happens if I miss the revalidation date?If an active service location in PROMISeTM is not revalidated by the revalidation date specified in ePEAP, the servicelocation will be automatically end dated/closed. An end dated/closed enrollment attached to a service location inPROMISeTM will prevent Consolidated and P/FDS providers from receiving payment for services rendered at theexpired service location during the period the service location is inactive in the system regardless of whether or notservices have been authorized on the Individual Support Plan. When a Base provider submits a claim(s) throughPROMISeTM for an end dated/closed service location, those claims will be denied and show as denied on theirremittance advices. In order to make an end dated/closed service location active again, a provider will have tocomplete and submit a new “PROMISeTM Provider Enrollment Base Application” to ODP. Processing time tocomplete the entire enrollment process is approximately six months. During the six (6) month period, providerswill be unable to receive payment for services rendered regardless of whether or not services have beenauthorized on the Individual Support Plan.!ODP recommends that Administrative Entities ensure the effective date associated with the provider’s profile inPROMISeTM is valid before authorizing services on the ISP.I am a licensed residential provider. Am I required to submit my Approved Program Capacity (APC)letter in order to revalidate each service location?Providers who render waiver funded licensed or unlicensed residential habilitation service are required to requestand receive a decision from ODP before opening a new or closing an existing location. After ODP has approved thenew waiver residential habilitation service location, providers who render services in a 6400 licensed service locationmust obtain an ODP decision notice for approved program capacity, also known as an APC letter. A request for anAPC is also needed when the provider of the 6400 licensed service location is requesting a change to the current APCfor an existing residential habilitation waiver service location.Providers who render services in a 6400 licensed service location are not required to submit an APC letter duringrevalidation.See Informational Packet # 055-12 for more information regarding ODP approval of residential services locations andapproved program capacity.ISSUE DATE: 6/20/2014ODP Communication Number: Memo 041-14page 6 of 7
REMINDERSProviders are reminded of the ongoing requirement to inform the Department of any changesin their provider enrollment application, such as changes in direct or indirect ownership andcontrolling interest five (5) % or greater interest, contact information changes, address changes(including email addresses), closed or invalid service locations, or any changes to theinformation provided on their provider enrollment application, that would otherwise renderthe information in their current provider file inaccurate or incorrect3.RESOURCESODP has received many inquiries from stakeholders regarding the ACA and revalidation. Belowis a summary of resources: See MA Bulletin # 99-14-06 for the procedure to use to determine your revalidationdeadline and additional details regarding revalidation. See Medical Assistance Provider Quick Tips #172 for details regarding the ProviderRevalidation Date Fields on the Provider’s Profile Providers can review the ACA website to receive up to date information concerning eact/index.htm Providers can sign up for the ACA Provider Enrollment and Screening Listserv for the latestannouncements and news on implementation activities der-enroll-screening.htmlINQUIRIESProviders and stakeholders may e-mail questions related to the provisions found in thiscommunication to:Office of Developmental Programs (ODP)Provider Enrollment:RA-odpproviderenroll@pa.gov3See CHAPTER 51. OFFICE OF DEVELOPMENTAL PROGRAMS HOME AND COMMUNITY-BASED SERVICES, § 51.47. Reporting requirements forownership change. Hyperlink: ap51toc.html#51.47.ISSUE DATE: 6/20/2014ODP Communication Number: Memo 041-14page 7 of 7
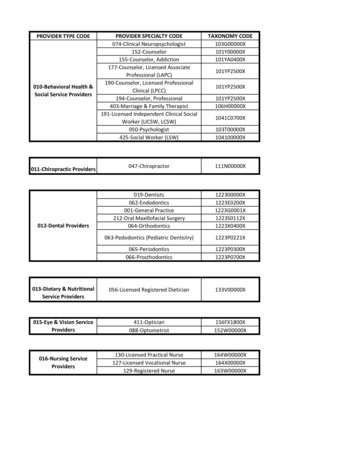
Once you reach the “Enrollment Information” screen of the DPW PROMISe provider enrollment website, scroll down until you find your provider type. lick on the “Enrollment Application/Provider Agreement” hyperlink loca