Transcription
MAYO CLINIC SCHOOL OF HEALTH SCIENCES ALUMNI ASSOCIATION SPRING 2020Connections
FROM THE ALUMNIASSOCIATIONpresidentThe year as president of the MCSHSAlumni Association has flown by. There’smuch more to be accomplished, and I’mexcited to keep the momentum going.I can’t say enough about our AlumniAssociation. Working with so manywonderful people makes my time aspresident worthwhile and memorable.I encourage everyone to get involved inthe Alumni Association. At a minimum,pay your 10 annual dues; this helpsto support programs and activities foralumni. For greater involvement, nominateyourself to be on the Alumni AssociationBoard of Directors. It’s only a three-yearcommitment and doesn’t demand toomuch of your time. If you’re curious aboutwhat’s expected, contact the Alumni Centeror one of the Board members listed in theback of this issue.All alumni are invited to attend the April 17annual program and dinner. There willbe a dinner at each Mayo Clinic site and atelecast of the keynote speaker, businessmeeting and award presentation inRochester. We’re also trying to organizean annual Alumni Day at each site likethe one we’ve had in Jacksonville for thelast two years (page 27). Watch for moreinformation about that.We’ve all had beloved mentors whotrained at MCSHS. The AlumniAssociation’s Recognition of OutstandingContribution award honors an alum eachyear. We’re always interested in yourthoughts about who should receive thisaward. Please nominate deserving alumni:mshsalumni.mayo.edu/people/awards.Pamela Lovett, APRN, CRNA, DNP (NA ’03)Certified registered nurse anesthetistDepartment of Anesthesiology andPerioperative MedicineAssistant professor of anesthesiologyMayo Clinic in FloridaHave a healthy 2020!
TABLE OFcontentsDistinguished Allied Health Educatorof the Year, MCSHS in Arizona.2Distinguished Allied Health Educatorof the Year, MCSHS in Florida.4From rad tech to operations administrator.6A home base: Mayo Clinic’s Transgenderand Intersex Specialty Care Clinic .8Know your Board.14Brain tumor experience givesPT student perspective.18HELP! Second victim peer supportprogram helps providers in distress.20News briefs.25On the cover:Social worker Katie Ubl, LGSW, MSW, and physician assistantJustine Herndon, PA-C, see patients in the Mayo Clinic Transgenderand Intersex Specialty Care Clinic, which started in 2016. Ubl sayspatients express their excitement that Mayo Clinic is involved intransgender care. “That Mayo is willing and open to providing thiscare has an impact on this group.”SPRING 2020 1
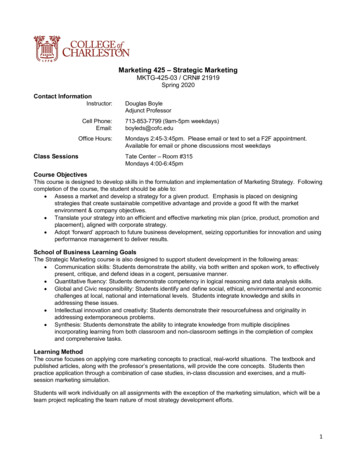
Anthony Mendez, PA-C, MSDistinguished Allied HealthEducator of the YearMCSHS IN ARIZONAAnthony Mendez, PA-C, MS (PA ’08, ENT ’09),didn’t set out to teach. It wasn’t until he wasa trainee in the MCSHS Physician AssistantFellowship in Otolaryngology/Head & NeckSurgery that he considered teaching.“I was inspired by the surgeons and physicianassistants who taught me, and I wanted to be partof that environment,” says Mendez, an instructorin otolaryngology in the Mayo Clinic College ofMedicine and Science.Fast forward a decade, and Mendez is programdirector for the fellowship and recipient of the2019 Distinguished Allied Health Educator of theYear award for MCSHS in Arizona. Departmentchair Michael Hinni, MD, nominated Mendez forthe award, describing him as a consummateprofessional, patient, enthusiastic, a joy to bearound, and a truly special provider and teammate.“Tony never hesitates to take time to teachothers including PA students, medical students,residents, ASU students and patients,” saysDr. Hinni. “Other staff members seek him outfor his expertise, and he drops whatever he’sdoing to help. His positive attitude is infectious.Every day, patients say, ‘Where’s Tony?’ and ‘TellTony I asked about him.’ Their fondness for Tonyenhances their experience immeasurably.”2 MAYO CLINIC SCHOOL OF HEALTH SCIENCES ALUMNI ASSOCIATIONMendez describes his teaching style asenergetic, spontaneous and organic. “In asurgical specialty, you learn on the fly — onthe floor, during rounds, crowded around thepatient in the OR, in the clinic, in hallwaysand in between being paged. Every momentpresents a teaching opportunity.”When he was associate program director ofthe fellowship, Mendez helped then-programdirector Carrlene Donald, PA-C, MS (PA ’07,ENT ’08), obtain program accreditation fromthe PA governing body, including formalizingthe curriculum and organizing a site visit. ThePA ENT fellowship was the first of its kindin the U.S. to earn accreditation. Mendez hascontinued to strengthen the program with newdidactic courses, increased access to educationalmaterials, and more PAs and physiciansinvolved in the program.Mendez says he’s motivated by wanting to makesure future generations of PAs are set up to beexcellent providers. “It’s fulfilling to pass alongwhat others have taught me so everyone canperform at the highest level possible. EverythingI do is for our patients.”
“It’s fulfilling to passalong what others havetaught me so everyonecan perform at thehighest level possible.”Anthony Mendez, PA-C, MSSPRING 2020 3
“ To be nominated bycolleagues I hold inhigh regard is veryspecial to me."Joshua Propst, PA-C4 MAYO CLINIC SCHOOL OF HEALTH SCIENCES ALUMNI ASSOCIATION
Joshua Propst, PA-CDistinguished Allied HealthEducator of the YearMCSHS IN FLORIDAIn 2009 Joshua Propst, PA-C (PA ’11), reacheda fork in the road. His then-fiancée, Jody, sathim down and told him she realized he wasn’tcompletely happy. Knowing he was interested inhealth care, Jody presented the education pathsfor physician assistant and physician. She saidhe should pick one and she’d support him onwhichever path he chose.Propst chose the PA path, completing thetraining program at Nova SoutheasternUniversity in Fort Lauderdale, Florida,and a clinical rotation at MCSHS in Florida.Health care had always figured prominentlyin Propst’s life. His mother was a phlebotomistfor 25 years. When Propst was a child, hisolder brother received a kidney transplant. Hisfather had a lung transplant when Propst wasa young adult. After college Propst conductedneurochemistry research at Mayo Clinic in Floridabut found it didn’t hold his interest for a longterm career. So he took a health care-adjacentsales and marketing job.He’s grateful that Jody, now his wife, urged himto face what was missing in his life — a careerin health care. “I probably wouldn’t be in healthcare if she hadn’t helped me find direction,” saysPropst, who received the 2019 DistinguishedAllied Health Educator of the Year award forMCSHS in Florida.Propst is a physician assistant in the Department ofCritical Care Medicine, associate program directorof the NP/PA Critical Care Fellowship, and aninstructor of medicine in the Mayo Clinic Collegeof Medicine and Science. He has precepted the50 to 60 PA students who have rotated throughCritical Care since 2012, and received the 2019Preceptor of the Year award from the FloridaAcademy of Physician Assistants.“The first few days in the ICU can be overwhelming for our trainees,” says Propst, whodescribes his teaching style as hands-on andtailored to each student’s needs. “It’s gratifying tosee them transition to understanding things andsharing their knowledge with others. Teachinghelps keep my knowledge base fresh.”Propst was instrumental in developing thecurriculum for the fellowship’s 2016 launch.“I want to make sure our PAs understand whatthey need to know to be excellent critical careproviders so they can practice anywhere in thecountry and be regarded by their institutions andcolleagues as exceptional,” he says.Propst says he’s humbled by the teaching award.“To be nominated by colleagues I hold in highregard is very special to me.”Propst isn’t the only one in his family to followhis heart’s desire. Jody had been a teacherand returned to school. She’s now a pediatricpsychiatric nurse practitioner at NemoursChildren’s Hospital in Jacksonville.SPRING 2020 5
From rad tech tooperations administratorCHRISTOPHER GULDEN ON HIS ADVANCEMENTIN MAYO CLINIC HEALTH SYSTEMChristopher Gulden, MA (RAD ’99), became familiar withMayo Clinic at an early age. He had surgery for a congenitalheart condition, coarctation of the aorta, at age 3. He grewup in Rochester, Minnesota, and at age 17 visited MCSHSas part of a Boy Scouts program to learn about health carecareers. He was drawn to radiography.Gulden completed the MCSHS Radiography Program andreceived an associate’s degree from Rochester Communityand Technical College along with a certificate in radiography.Employment as a radiologic technologist at Mayo Clinicfollowed. After a year, he began a bachelor’s degreeprogram in organizational management and communicationat Concordia University in St. Paul, Minnesota, whilecontinuing to work at Mayo Clinic.“Radiography was moving toward bachelor’s degreeprograms,” says Gulden. “I’d have more opportunitiesfor advancement with an undergraduate degree.”With his new degree, Gulden transferred to Mayo ClinicHealth System in Lake City, Minnesota, where he waspromoted to director of radiology. He also embarked on amaster’s degree in organizational management at Concordia.Four years later he was appointed operations manager oflaboratory, radiology and surgery at Mayo Clinic HealthSystem in Lake City. For the first time he was out of directpatient care and in charge of areas besides radiology.Gulden’s career advanced, and he gained responsibility. Hebecame site operations administrator at Mayo Clinic HealthSystem in Lake City and operations administrator for the6 MAYO CLINIC SCHOOL OF HEALTH SCIENCES ALUMNI ASSOCIATIONMayo Post Acute Care Program (MPAC). MPAC focuses ontransitions of patients from the four large Mayo hub locations(Eau Claire and La Crosse, Wisconsin; and Mankato andRochester, Minnesota) to the 10 smaller Mayo critical-accesshospitals across Iowa, Minnesota and Wisconsin.Two years later, Gulden attained his current position —operations administrator for Mayo Clinic Health System –Southeast Minnesota Region, which includes the hospitaland emergency medicine service line in Albert Lea, Austin,Cannon Falls, Lake City, Owatonna and Red Wing. Hecontinues to serve as MPAC Midwest administrator.Gulden encourages alumni to consider working at MayoClinic Health System’s community hospitals. “You can get toknow the providers, staff and senior leadership well becausethe sites are smaller. It’s a good training ground to learn howdepartments work. Some Mayo Clinic initiatives are pilotedin Mayo Clinic Health System because they’re easier to testin smaller environments before implementing them in thelarger organization.”Gulden has now spent half of his life at Mayo. “WhenI started training at MCSHS, I didn’t realize all theopportunities available,” he says. “If an area of practiceor business catches your eye, get more education to makeyourself a viable candidate. Get involved in and becomemore visible via projects, committees and initiatives.Having a clinical background has helped me make goodadministrative decisions because I can empathize with whatproviders and patients experience.”
“ Having a clinicalbackground hashelped me makegood administrativedecisions."Christopher Gulden, MASPRING 2020 7
A home baseMayo Clinic’s Transgender and Intersex Specialty Care Clinic providesfor mental health, hormonal and surgical needs of transgenderpatients and those with differences of sexual developmentMayo Clinic established a Transgender and IntersexSpecialty Care Clinic (TISCC) in 2015, based in the Divisionof Endocrinology, Diabetes, Metabolism, & Nutritionin Rochester. The clinic provides for the mental health,hormonal and surgical needs of transgender patients andthose with differences of sexual development (DSD) —sometimes called intersex.Mayo Clinic is one of the first major academic medicalcenters to offer multidisciplinary transgender care,including a gender-affirming surgery program. The surgicalprogram started in 2016 with breast and facial procedures;vaginoplasty surgery was introduced in 2017.The TISCC has seen more than 500 patients since 2015,with more than half coming from the five-state region,and one-third from central and southern Minnesota. TheMayo surgical team has performed approximately 150vaginoplasties in patients ranging in age from their 20s to70s. Not all transgender individuals choose to have surgicalprocedures to achieve gender congruence.“The transgender population faces major challenges inassessing and obtaining appropriate health care,” saysTodd Nippoldt, MD, medical director of the TISCC.“One-quarter of transgender individuals says they’veavoided going to the doctor for fear of discrimination.Mayo Clinic believes that all patients are best served witha multidisciplinary approach. We offer transgender patientsa home base for their care where they are appropriatelycared for and respected.“Some people erroneously think transgender patients makea choice to change their gender. Rather, it’s about confirmingtheir identity and wanting to live authentically. Beingtransgender indicates diversity, not pathology. Our goalis to relieve the distress associated with the incongruencebetween their gender identity and physical body. The TISCCpractice is the right thing to offer to this patient population,and it has enthusiastic support from Mayo Clinic’stop leadership.”BY THE NUMBERS0.58% 29%24%47%0.58% of U.S. adultpopulation identifiesas transgender, or 1.4million people24% of those who wereout or perceived astransgender in gradesK-12 were physicallyattacked because ofbeing transgender47% of transgenderindividuals have beenvictims of sexual assault29% of transgenderindividuals live inpoverty — 2 timesthe rate in the U.S.population8 MAYO CLINIC SCHOOL OF HEALTH SCIENCES ALUMNI ASSOCIATION
The Transgender and IntersexSpecialty Care Clinic’s clinical director,Cesar Gonzalez, PhD, and medicaldirector, Todd Nippoldt, MD.70%78%40%55%70% of transgenderindividuals havehad some form ofmaltreatment at thehands of medicalproviders78% of adult patientsseen for gender-relateddiagnoses report havingdepressionStudies suggest that40% of transgenderpeople have tried tocommit suicide — afigure 9 times higherthan the general publicWhen appropriate healthcare has been denied toindividuals who identifyas transgender, thesuicide attempt raterose to 55%SPRING 2020 9
“In the past, many transgender and intersex individualshad to rely upon fragmented and incomplete health care,”says Dr. Hayes. “Few major academic medical centershad specialty programs for advanced care. These patientsnow can access the Mayo Clinic Transgender and IntersexSpecialty Care Clinic, where their health care teams workwith them to develop the right care plan for both optimalhealth and being true to themselves.”Sharonne Hayes, MDTISCC patients see behavioral health and endocrinologyproviders first. Those providers evaluate and optimize anysocial, mental health or medical issues.Before initiating hormonal or surgical therapies, patientsmust meet World Professional Association for TransgenderHealth (WPATH) standards of care, which outline the stepsnecessary to achieve the best outcomes. WPATH standardsvary for each surgical procedure and may include lettersof approval from the patient’s mental health professional,prior hormonal therapy and at least one year of living as thegender with which the patient identifies. Each patient’s caseis discussed at the multidisciplinary TISCC case conferenceand proceeds to surgery only after consensus that all issueshave been addressed and optimized.Sharonne Hayes, MD, medical director of the Mayo ClinicOffice of Diversity and Inclusion, says the TISCC is a perfectexample of what sets Mayo Clinic apart: a multidisciplinary,collaborative approach to care that meets all of the needs ofeach patient.In pursuit of evolving equity, diversity and inclusion, MayoClinic has made great efforts not just to get patient-affirmedpronouns right but also to modify the medical record —from how patient names are listed to what normal ranges arefor gender-specific lab reports.The TISCC is truly three shield. Mayo Clinic School ofContinuous Professional Development offers a CME course,“Principles in the Care of Transgender and Intersex Patients.”TISCC providers are involved in presentations at nationaland international meetings, and conducting research —with more than 15 manuscripts published in the last twoyears. The TISCC also shares its expertise with health careproviders in local communities who see patients who havehad gender-affirming surgery at Mayo Clinic.Studies show that after hormonal therapy and genderaffirming surgery, 80% of transgender individuals (notnecessarily treated at Mayo Clinic) report significantimprovement in their gender dysphoria, 80% reportsignificant improvement in quality of life, 78% reportsignificant improvement in psychological symptoms and72% report significant improvement in sexual function.Plastic and reconstructive surgeon Jorys Martinez-Jorge, MD,says TISCC patients are the most grateful patients he has.“They feel like they’re trapped in the wrong body, whichaffects all aspects of their lives. They just want to live lifelike I do. We can give that to them through medical careand technologies, and it’s professionally and personallyrewarding.”Learn more about working withgender-diverse patients and colleagues: lgbthealtheducation.org transhealth.ucsf.edu wpath.org10 MAYO CLINIC SCHOOL OF HEALTH SCIENCES ALUMNI ASSOCIATION
10 tips to become a transgender-friendly providerMost health care providers have had little or no formaltraining in addressing the needs of transgender patients,which can contribute to the stress that members ofthe transgender community may develop throughstigmatization, avoidance, discrimination and prejudice.1.If you have a question about your patient’sgender nonconformity, don’t be afraid to ask.2.Ask patients their preferred names and pronouns,and use them during the encounter. If you make amistake, apologize and continue.3.The preferred name and pronoun often willdiffer from what is in the medical record. Manytransgender people haven’t changed their nameand gender legally. Ask the patient if you can usethis preferred name and pronoun in the medicalrecord. Many patients have access to theirmedical records, and your sensitivity should bereflected in the notes.4.If possible, intake forms should include an optionto disclose transgender status.5.Sensitivity training should be required for allstaff members who interact with the patient. TheCenter of Excellence for Transgender Health atthe University of California, San Francisco, haspublished a helpful online course, transhealth.ucsf.edu/video/story.html.6.7.Public restrooms should include a unisex option.8.Include transgender health topics as part ofmedical school and training programs to increasethe competence of future leaders in transgenderhealth care.9.Provide faculty development in transgenderhealth. Many national and international meetingsinclude transgender health topics, and moreonline resources are available.Have local transgender resources, such assupport groups, available to help guide thepatient if needed.a friend: Be aware of qualified providers10. Phonein your area who you can contact abouttransgender-related questions.“ Few major academic medical centers had specialty programs foradvanced care. These patients now can access the Mayo ClinicTransgender and Intersex Specialty Care Clinic, where their healthcare teams work with them to develop the right care plan for bothoptimal health and being true to themselves.”Sharonne Hayes, MDSPRING 2020 11
ALLIED HEALTH ALUMNI IN THE
Justine Herndon, PA-C, see patients in the Mayo Clinic Transgender and Intersex Specialty Care Clinic, which started in 2016. Ubl says patients express their excitement that Mayo Clinic is involved in transgender care. “That Mayo is willing and open to providing this care has an impac