Transcription
HHS Risk Adjustment DataValidation (HHS-RADV):Proposed Rule on Amendmentsto RADVJune 24, 2020This communication was printed, published, or produced and disseminated at U.S. taxpayer expense. The information in this presentation is only intendedto be a general informal summary of technical legal standards. It is not intended to take the place of regulations that it is based on. We encourage audiencemembers to refer to the applicable regulations for complete and current information about the requirements that apply to them.
Session Agenda Session GuidelinesWebinar and Audio Access TipsIntended AudienceSession PurposeBackgroundHierarchical Condition Category (HCC) Grouping MethodologyPayment Cliff and Sliding Scale AdjustmentsNegative Failure Rate ConstraintSwitching to the Benefit Year Being AuditedQuestion and Answer (Q&A)ResourcesClosing Remarks2
Session Guidelines This is a 60-minute webinar session Stakeholders may now listen to today’s event via their computerspeakers or telephone‒ To listen through your computer speakers, please ensure yourcomputer volume is not muted‒ To listen through your telephone, dial (866) 442-5690 and enter yourunique six (6)-digit Personal Identification Number (PIN) If you cannot hear today’s audio or are having other technicalissues, please contact the Registrar at registrar@regtap.info or (800)257-95203
Session Guidelines (continued) To submit a question during today’s webinar‒ Type into the Q&A panel on the lower, right-hand side of your screen‒ Hit the Send button to submit your question to The Centers forMedicare & Medicaid Services (CMS) Subject Matter Experts Please email additional content questions toCCIIOACARADataValidation@cms.hhs.gov For questions regarding logistics and registration, please contactthe Registrar at registrar@regtap.info or (800) 257-95204
Webinar and Audio Access Tips Hardwire your computer as opposed to using Wi-Fi Close unnecessary applications and browser sessions on your device forbetter connectivity Reduce simultaneous streaming activities by others in your currentworkplace/home to increase your bandwidth Disconnect from any Virtual Private Network (VPN) if able andapplicable for the best experience Switch to phone if you lose web connectivity or sound when listeningthrough your computer The telephone number is (866) 442-5690 and your individual PIN isincluded in your meeting reminder email5
Intended Audience Issuers subject to the HHS-RADV Audit requirementsunder 45 CFR § 153.630 State Regulators/State Agencies Initial Validation Audit (IVA) Entities Third Party Administrators (TPA) and Support Vendors6
Background
BackgroundPatient Protection and Affordable Care Act (PPACA):– Section 1343: Established a permanent risk adjustment (RA)program to provide payments to health insurance issuers thatattract higher-risk enrollees to reduce the incentives for issuers toavoid those enrollees, and to lessen the potential influence of riskselection on the premiums that issuers charge– Section 1321: Directs HHS to operate the RA program on behalf ofStates that do not elect to do so8
Background (continued)Department of Health and Human Services - RiskAdjustment Data Validation (HHS-RADV):– Serves as an audit of the information used in establishing anenrollee’s risk score for purposes of calculating the issuer’s planliability risk score (PLRS) under the HHS-operated RA program– Uses a multi-step process called error estimation to calculateerror rates that are used to adjust outlier issuers’ risk scores,resulting in an adjustment in RA transfers for the applicablestate market risk pool(s)9
Background (continued) 2015 & 2016 benefit years HHS-RADV were pilot years 2017 benefit year* and beyond HHS-RADV will be used toadjust risk scores and RA transfers* 2017 was a pilot year for Massachusetts issuers. See the 2020 PaymentNotice Final Rule, 84 FR 17454 at 17508.10
Background (continued) May 2019: Released 2017 Benefit Year HHS-RADV error rate results Summer 2019: Conducted a series of stakeholder listening sessionson HHS-RADV August 2019: Released 2017 Benefit Year HHS-RADV transfer results December 2019: Released HHS-RADV White Paper for comment May 2020: Released HHS-RADV proposed rule June 2020: Released 2018 Benefit Year HHS-RADV error rate results11
Provisions in the Proposed Rule Based on the feedback we received and our experience from the initial yearsof HHS-RADV, we propose three (3) modifications to the error rateestimations methodology:– Changes to the methodology for determining HCC Failure Rate Groups– Introduction of sliding scale adjustments to certain outlier issuers’ risk scores– Constraint on risk score adjustments for negative failure rate issuers We additionally propose to transition from the current prospectiveapplication* to apply HHS-RADV results to the RA transfers of the benefityear being audited* The current exception is for exiting issuers, whose HHS-RADV results are applied to the risk scores andtransfers of the benefit year being audited. See, e.g., the 2020 Payment Notice, 84 FR at 17503.12
HCC Grouping Methodology
HCC Grouping MethodologyMedical conditions are grouped in distinct ways for HHSoperated RA and the HHS-RADV processes For HHS-operated RA model development:––––Hierarchies of HCCs,HCC coefficient estimation groups,A priori stability constraints, andHierarchy violation constraints For HHS-RADV:– HHS-RADV HCC failure rate groups14
HCC Grouping Methodology (continued) Interactions among these groupings can lead to greater or lesserHHS-RADV adjustments to risk scores than may be warranted incertain circumstances based on the HCC failure rate groupings thatthe HCCs are sorted into This could lead to HHS-RADV adjustments for certain HCCs inHHS-RADV that reflect the classification and grouping of theHCCs, rather than risk differences between the HCCs The effects of this interaction could be especially pronounced forHCCs in the same HCC coefficient estimation group15
HCC Grouping Methodology (continued) For example, HCC 54 Necrotizing Fasciitis and HCC 55 Bone/Joint/MuscleInfections/Necrosis share a hierarchy and an HCC coefficient estimation groupin risk adjustment, resulting in risk score coefficients constrained to be equal– However, for 2017 benefit year HHS-RADV, HCC 54 was in the high failure rate HCCgrouping, while HCC 55 was in the medium failure rate HCC grouping In validating an enrollee with HCC 54 in HHS-RADV, the IVA or SVA Entity may find that anenrollee with HCC 54 reported in External Data Gathering Environment (EDGE) is not validatedas having HCC 54, but the enrollee may have been found to have HCC 55 in issuer’s HHS-RADVaudit data– In this case, when taken together with the issuer’s other HHS-RADV results, HCCs inthe same HCC coefficient estimation group could contribute to an issuer’s failure ratein a HCC failure rate grouping, even though the HCCs do not have different risk scoresand an adjustment to risk scores is not conceptually warranted16
HCC Grouping Methodology (continued) To address the influence of HCC hierarchies and coefficientestimation groups, we propose:– To modify the creation of HHS-RADV HCC failure rate groupings andplace all HCCs that share an HCC coefficient estimation group in theadult RA models into Super HCCs prior to sorting the HCCs into HHSRADV failure rate groups Combining the HCC coefficient estimation groups into Super HCCsfor HHS-RADV as proposed would prevent mis-codings betweenrelated HCCs with the same risk score from contributing to thenational metrics and issuer failure rates17
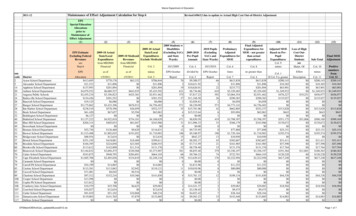
HCC Grouping Methodology (continued) HCC Coefficient Estimation Groups that would be used to create Super HCCsfor 2019 benefit year HHS-RADV would be:HHSV05 HHS-HCC LABELHCC19Diabetes with Acute Complications20Diabetes with Chronic Complications21Adult Model HCCCoefficientEstimation GroupHHSV05 HHS-HCC LABELHCC106Traumatic Complete Lesion Cervical Spinal Cord107QuadriplegiaDiabetes without Complication108Traumatic Complete Lesion Dorsal Spinal s and Glycogenosis117Muscular Dystrophy29Amyloidosis, Porphyria, and Other Metabolic Disorders30Adrenal, Pituitary, and Other Significant Endocrine Disorders119Parkinson's, Huntington's, and Spinocerebellar Disease, and OtherNeurodegenerative Disorders54Necrotizing Fasciitis126Respiratory Arrest55Bone/Joint/Muscle Infections/Necrosis127Cardio-Respiratory Failure and Shock, Including Respiratory Distress Syndromes61Osteogenesis Imperfecta and Other Osteodystrophies128Heart Assistive Device/Artificial Heart62Congenital/Developmental Skeletal and Connective Tissue Disorders129Heart Transplant67Myelodysplastic Syndromes and Myelofibrosis160Chronic Obstructive Pulmonary Disease, Including Bronchiectasis68Aplastic Anemia161Asthma69Acquired Hemolytic Anemia, Including Hemolytic Disease ofNewborn187Chronic Kidney Disease, Stage 5188Chronic Kidney Disease, Severe (Stage 4)70Sickle Cell Anemia (Hb-SS)G01G02AG03G04G06G0771Thalassemia Major204 Miscarriage with ComplicationsCombined and Other Severe Immunodeficiencies205 Miscarriage with No or Minor Complications74Disorders of the Immune Mechanism81Drug Psychosis82Drug DependenceG09G10G11G12G13G14G15G16203 Ectopic and Molar Pregnancy, Except with Renal Failure, Shock, or Embolism73G08Adult Model HCCCoefficientEstimation GroupG17207 Completed Pregnancy With Major Complications208 Completed Pregnancy With ComplicationsG18209 Completed Pregnancy with No or Minor Complications18
Payment Cliff andSliding Scale Adjustments
Payment Cliff and Sliding Scale Adjustments Current Methodology: Group Adjustment Factor (GAF) is the difference between issuer’sgroup failure rate (GFR) and the national weighted mean group failure rate:𝐺𝐺𝐺𝐺𝐺𝐺𝐺𝐺,𝑖𝑖 𝐺𝐺𝐺𝐺𝑅𝑅𝐺𝐺,𝑖𝑖 𝜇𝜇{𝐺𝐺𝐺𝐺𝑅𝑅𝐺𝐺 }, Two (2) issuers may have very similar failure rates, but will be impacted very differentlydepending on their outlier status:20
Payment Cliff and Sliding Scale Adjustments (continued) This scenario has been described as a “payment cliff” effectwhere:– an outlier issuer that has a group failure rate slightly outside theconfidence intervals is adjusted by a potentially large amount (basedon its distance from the weighted mean group failure rate) and– an issuer that is slightly inside the confidence interval is not adjusted21
Payment Cliff and Sliding Scale Adjustments (continued) To promote fairness and predictability, we propose to createa sliding scale adjustment from /-1.645 to 3 standarddeviations to mitigate the “payment cliff” effect– Applies a sliding scale formula that would decrease the error ratesfor outlier issuers that are slightly outside the confidence intervalsand– Changes the confidence intervals such that more outliers wouldbe identified22
Negative Failure RateConstraint
Negative Failure Rate Constraint An issuer may be identified as a negative error rate outlier for anumber of reasons– For example, an issuer may be identified as a negative error rate outlierbecause the issuer is much better at reporting accurately to EDGE andvalidating diagnoses in HHS-RADV as compared to other issuers– Alternatively, an issuer with incomplete EDGE data submissions couldbe identified as a negative failure rate outlier because additional HCCswere found during HHS-RADV that the issuer did not originally reporton its EDGE server24
Negative Failure Rate Constraint (continued) To improve predictability and mitigate the impact of HHS-RADVadjustments due to negative error rate outliers, we propose to applya constraint to the error rate calculation for negative error rateissuers with negative failure rates so that the group failure rate forwhich they are credited is equal to zero (0)– This proposal would limit the financial benefit for issuers whose IVAEntities find large quantities of HCCs in HHS-RADV that were notreported on the EDGE server25
Switching to the Benefit YearBeing Audited26
Switching to the Benefit Year Being Audited Currently, HHS-RADV results are generally applied on a prospectivebenefit year basis– For example, 2017 benefit year HHS-RADV results generally adjusted 2018benefit year risk scores and transfers– The exception is for exiting issuers, whose 2017 HHS-RADV results were usedto adjust 2017 risk scores and transfers We propose to transition to an approach that would apply HHS-RADVresults to the risk adjustment benefit year being audited for all issuers– This proposal:o is intended to address stakeholder concerns about maintaining actuarial soundnessin applying an issuer’s HHS-RADV error rate if an issuer’s risk profile, enrollment, ormarket participation changes substantially from benefit year to benefit yearo has the potential to provide more stability for issuers of RA covered plans andimprove predictability of HHS-RADV results27
Switching to the Benefit Year Being Audited (continued)To transition to this policy, starting with the 2020 and 2021 benefityears, we propose to: Separately calculate and apply 2020 and 2021 HHS-RADV risk scoreadjustments using these three (3) steps:a. Apply 2020 HHS-RADV risk score adjustments to 2021 RA PLRSb. Apply 2021 HHS-RADV risk score adjustments to the previously adjusted 2021PLRS (reflecting the 2020 benefit year HHS-RADV results) andc. Apply the final adjusted PLRS (reflecting both the 2020 and 2021 HHS-RADVresults) to adjust 2021 benefit year RA transfersAlternatively, we seek comment on whether HHS should use an averageerror rate approach to make this transition28
Switching to the Benefit Year Being Audited (continued)On April 13, 2020, CMS announced the postponement of 2019Benefit Year HHS- RADV activities due to Coronavirus 2019(COVID-19) In light of the delay of 2019 HHS-RADV, we also seek comment onwhether we should switch to adjusting the benefit year beingaudited beginning with 2020 HHS-RADV, therefore requiring thecombination of 2019 and 2020 HHS-RADV results, rather thanmaking this change beginning with 2021 HHS- RADV29
Next Steps The Proposed Rule (85 FR 33595) went on displayMay 29, 2020– Federal Register publication date: June 2, 2020– Comment Deadline: July 2, 2020 The proposed rule is available 2/pdf/2020-11703.pdf30
Q&A
Q&A To submit a question during today’s webinar– Type into the Q&A panel on the lower, right-hand side of yourscreen– Hit the Send button to submit your question to CMS32
Resources
Locating HHS-RADV Documents in REGTAP Stakeholders can accessadditional documents in theREGTAP library athttps://www.REGTAP.info– Under Program Area, select HHSRisk Adjustment Data Validation(HHS-RADV)34
Upcoming WebinarTopicDate2018 Benefit Year HHS-RADVReviewing D&E and RXCJuly 1, 202035
Resources: LinksResourceResource LinkU.S. Department of Health & Human Services (HHS)http://www.hhs.gov/Centers for Medicare & Medicaid Services (CMS)The Center for Consumer Information & Insurance Oversight(CCIIO)Consumer Website on Health Reformhttp://www.cms.gov/Registration for Technical Assistance Portal t Protection and Affordable Care Act re.gov/36
Resources: Links (continued)ResourceHHS Notice of Benefit and Payment Parameters for 2014HHS Notice of Benefit and Payment Parameters for 2015HHS Notice of Benefit and Payment Parameters for 2016HHS Notice of Benefit and Payment Parameters for 2017HHS Notice of Benefit and Payment Parameters for 2018HHS Notice of Benefit and Payment Parameters for 2019HHS Notice of Benefit and Payment Parameters for 2020HHS Notice of Benefit and Payment Parameters for 2021Resource 37
Resources: Links (continued)ResourceResource Link2018 Benefit Year HHS-RADV Protocolshttps://www.regtap.info/reg librarye.php?i 29042018 Benefit Year HHS-RADV Timeline (4/13/20)https://www.regtap.info/reg librarye.php?i 3206Issuer Exemption and Participation Requirements(3/11/20)Issuer SO Designation and Maintenance (3/11/20)Conflict of Interest and Issuer IVA Entity Designation(3/11/20)2018 SVA Findings Report Attestation and DiscrepancyReporting & MR Recommendations on Abstraction(3/25/20)2018 Benefit Year Error Estimation (5/20/20)https://www.regtap.info/reg librarye.php?i 3207https://www.regtap.info/reg librarye.php?i 3208https://www.regtap.info/reg librarye.php?i 3209https://www.regtap.info/reg librarye.php?i 3224https://www.regtap.info/reg librarye.php?i 330238
Resources: Contact InformationResourceContact InformationFor RADV policy questions, contact the RADV TeamCCIIOACARADataValidation@cms.hhs.govFor EDGE server questions, please contact yourEDGE server data@cms.hhs.govFinancial Management (FM) Service Representativeand copydirectly and copy the Centers for Medicare & MedicaidCMS FEPS@cms.hhs.govServices (CMS) Help DeskTo contact us within the HHS-RADV Audit Tool, useHHS-RADV Audit Toolthe Inquiries tab and select “Submit Inquiry”39
Closing Remarks
For questions regarding logistics and registration, please contact the Registrar at registrar@regtap.info or (800) 257-9520. 5 . Summer 2019: Conducted a series of stakeholder listening sessions on HHS-RADV . HCCs, rather th