Transcription
Summer 2010CLINICAL INFORMATION FOR THE GT PROFESSIONALIn This IssueCASE REPORTCASE REPORTSpeedskater’s Tensor FasciaLata Improved with GTBy Eric St. Pierre, DC,DACBSP, CSCS, South PointeMedical Center, Lafayette, COPage 1By Eric St. Pierre, DC, DACBSP, CSCS, South Pointe Medical Center, Lafayette, COVincent Leaves ‘Footprint,Legacy’Page 1Shakar Named GT ClinicalAdvisorPage 1CASE REPORTIASTM Used for Treatmentof Finger Joint SprainBy Evelina Gundeck, DPT,Amy Bayliss, DPT andM. Terry Loghmani, PT, PhD,Department of Physical Therapy,IU, Indianapolis, INPage 4CASE REPORT25-Year Post-TraumaticAchilles Tendon Injury HasExcellent ResponseBy Larry Smith, BPE, DC,Parksville, British ColumbiaPage 5Instructor Cites Importanceof Adhering to GT PrinciplesBy John W. Schrader, HSD,ATC/L, Clinical Professor,Departments of Kinesiologyand Athletics, IndianaUniversity and GT Instructor,Bloomington, INPage 6CASE REPORTAdhesive CapsulitisTreatment Gets ResultsBy C.J. Kleene, DC, Back inLine Family Chiropractic &Wellness, Hiawatha, IAPage 7Marketing HelpNew Customizable GT AdsPage 8GrastonTechnique.comSpeedskater’s Tensor Fascia Lata Improved with GTHistory:A male short-track speedskater presentedwith right lateral hip tightness after crashingin practice a week prior. The mechanismwas described as his skate “breaking out”from the ice at the apex of a left turningcorner at roughly 30 mph. A 20-foot, supineslide resulted in pelvic impact into abreak-away padding system, with his legsextended in the air. The athlete hadcompleted all ice- and land-based trainingsince the crash, but was experiencingprogressively worsening symptoms. Hedescribed minor tightness and ache to theright tensor fascia lata (TFL) while at rest,with moderate cramping in a skatingposition, worse when loaded onto the rightleg. Pain, paresthesia, popping, clicking,locking and instability of the extremity wereall denied. Also denied was previousdiagnosis of spinal, orthopedic and/orneurological injury and surgery.Examination:Initial examination generally found minortenderness and moderate hypertonicity ofboth hip complexes and lumbar spine. Theright TFL exhibited moderate tendernessand hypertonicity without visual signs ofContinued on page 2Vincent Leaves ‘Footprint, Legacy’Dr. Richard E. Vincent, the professionalface of Graston Technique since 2001,has stepped down from the position ofclinical advisor. Vincent, a nationallyrespected chiropractor, in Marchannounced his intention to leave GT in thespring to pursue private businessopportunities.Vincent, 81, is president of IntegrativeHealth Care Practice Resources (IHCPR),a web-based business that he co-foundedin 2006.“Dick Vincenthas left hisfootprint and hislegacy onGrastonTechnique ,” saidMichael I. Arnolt,GT president. “Itis in large partRichard E. Vincentbecause of Dick’svision, professional standing, leadershipand enthusiasm that we have reached aposition of prominence in the world of softContinued on page 3Professional and Academic Background CitedShakar Named GT Clinical AdvisorJacqueline (Jackie) J. Shakar, DPT, MS,ATC, has been named clinical advisor forGraston Technique . Shakar, who has 27years of clinical experience, started herposition June 1.Shakar, 50, has been using GT in a clinicalsetting since 2003 and has been a GTinstructor since late 2004. She is employedby Central Mass Physical Therapy &Wellness in Worcester, MA, and also is aprofessor in the physical therapist assistantprogram at Mount Wachusett CommunityCollege in Gardner, MA. She teacheskinesiology, orthopedic content and manualtherapy.Continued on page 3
Page 2The EDGESpeedskater’s TFL Improved with GTContinued from page 1injury or palpable defect. Postural analysis presented anectomorph somatotype in sway-back form with anteriorpelvic tilt. High fascial tension was noted of the abdominalcavity and right anterior-lateral hip in supine and seatedpositions, with marked increases in tension duringpassive hip extension and horizontal adduction. Both hipcapsules exhibited multi-directional restriction andmoderate deficits into internal rotation and extension.Active pelvic tilting found rigid control and limitation intoextension. Neurologic and orthopedic examination of theextremity and spine were unremarkable.Standardized functional assessment confirmed poorcoordinated movement between the spine, hips andpelvis, with asymmetry in rotational spinal stability,compromised balance, recruitment of accessorymusculature and a dependency on breath. During powerand strength training maneuvers, a “sloppy” pelvis and“breaking” core were identified, often producing the chiefcomplaint. During right-sided “push-off” while skating,minimal hip extension, excessive lumbar extension androtation of the pelvis were identified. At high speeds andpressures associated with the corner’s apex, the athlete’spelvis would close in toward the right hip rather than stayfirm and level which dampened the transfer of energy,compromising his control of pressure, maintenance ofspeed and proper lean to ideally exit out of the turn.Diagnosis:Myofascial pain centralized around the right TFL.Findings:Compromised inter-spinal, pelvic and extremity stability;multi-directional femoral-acetabular capsular restriction;multi-planar myofascial restriction and dysfunctionalbreathing patterns.Treatment:The treatment goal was to decrease discomfort in theskating position, while complementing a high-volumetraining block so the athlete could peak at the end of aquadrennial training program and essentially his mostimportant competition. Graston Technique, incombination with movement rehabilitation and manualABC TV NewsSpotlights GTCLICKheretherapies, wasessential to therecovery andpreventativeprocess. GTwas used ondifferent musclegroups andincorporatedinto thetreatmentschedule up to four times a week. Because thecompetition was so close, the objective was to addressthe quality and maintenance of motion already available,rather than promote large changes in ROM andsymmetry. However, the athlete quickly found great reliefand improvement in his skating technique with largegains in ROM and aggressive myofascial work.In the mornings, a sport-specific warm-up was used withthe athlete participating in a guided routine of spinal andpelvic self-mobilizations, active muscular lengthening,passive hip mobilizations and quick, light soft tissue workto rigid musculature. GT1, GT4 and GT5 were used oftenacross large fascial areas, using light, linear strokes orquick, short, multi-directional attention to adhesions alongmultiple planes. Different ranges of motion and tensionsalong the most objectively and subjectively restrictedplanes were exploited, without producing ecchymosis.After completion of the day’s training, GT generally wasused with greater intensity, with more attention paid tosymptomatic tissue. An ice bath was required oftenbecause of the volume of training executed 6 days aweek. All end-of-day treatment sessions included anextensive self-mobilization routine to ensure quantity andquality of motion.The athlete quickly experienced a decreased“lock-down” effect when in the skating position and felt“smooth” control of the pelvis and hip. The TFL also feltless “swollen” when in position. A common approachconsisted of GT3 and GT4 to the abdominal fascia, alongthe anterior hip and quadriceps in changing hip rangesand tensions (neutral, lengthened, concentric, eccentric,bridge, lunge, etc.) in conjunction with spino-pelvicself-mobilization progressions and a regrooving of squatand lunge progressions. Significant improvements werediscovered in a kneeling upright lunge position within aContinued on page 8
Page 3The EDGEVincent Leaves FootprintContinued from page 1tissue treatment.” Arnolt credits Vincent with successfullymelding professional clinicians from many disciplines—particularly, athletic trainers, chiropractors, occupationaltherapists and physical therapists—toward the commongoal of using Graston Technique to provide the finest ofsoft tissue treatment.He also is responsible for the entry of GT into theeducational offering of numerous chiropractic colleges.“It is because of the respect the top administrators havefor Dick Vincent that they were willing to listen and seethe value of adding a brand new component to treatmentto their curriculum,” Arnolt said. GT is a requirement orelective in 16 chiropractic colleges, the first two of whichwere added in 2002.Vincent, long an outspoken advocate of chiropractic,gained a large level of acclaim when Massachusetts in1966, after years of effort, passed a law to licensechiropractic. From 1950 to 1966, he practiced hisprofession in defiance of the Medical Practice Act. Hispresence and influence gained national attention as aboard member with the Federation of ChiropracticLicensing Boards and the National Board of ChiropracticExaminers.Vincent and his wife, Carla, reside in Falmouth, MA. Shecontinues to provide a cross-section of services,including training and continuing education, for GrastonTechnique . They jointly own and operate VincentManagement Inc., a consulting firm.Shakar Named Clinical AdvisorContinued from page 1Shakar has a doctorate in physical therapy (DPT) fromMGH Institute (2010), a master’s degree (MS) in physicaltherapy from Boston University (1983) and anundergraduate degree (MA) in psychology, with a minor insports medicine, from Worcester State College (1981).“The breadth of professional experience, her skills as aninstructor and ability to communicate made Jackie anexcellent choice,” said Michael I. Arnolt, GT president.The selection of Shakar was lauded by Richard E.Vincent, DC, previous clinical director for GT.“Jackie is an excellent appointment as clinical advisor,”Vincent said. “Her combination of clinical and academicexperiences make her well qualified for the position. Shewill work very well with the established inter-professionalculture of Graston Technique .”In making the announcement, Arnolt added, “Dick and Iagree Jackie is a professional and educator with respectthroughout the GT organization. I am very pleased sheaccepted the position.”Shakar, who will continue as a GT instructor in M1 andM2, will be the liaison with GT’s instructors, as well asclinicians in the field. Additionally, she will work with theadministrative, education and research components ofGT. Among her goals is to provide “clinicians and patientswith the most accurate and evidence-based solutions totheir questions.” Shakar also will guide the continueddevelopment of the Graston Technique as it emerges asthe premier method to deliverinstrument-assisted soft tissuemobilization.Instructor Base to ExpandOne of Shakar’s priorities willbe to create a regionalized baseJackie Shakarof instructors, across alldisciplines, to handle the increasing load of scheduledcourses and on-site trainings.“We have extraordinary instructors, and I believe it isimportant for us to be keenly aware of the importance ofproviding them with every opportunity to instruct, whilebeing cognizant of their desire to balance theirprofessional and personal lives. Seeking new instructorsto complement our trained staff is a key to our continuedsuccess,” Shakar said. She is counting onrecommendations from current instructors, along withother trained clinicians who have an interest in beinginstructors, to contact her concerning staff expansion.Shakar, who resides in Sutton, MA, has the distinction ofbeing trained in and using ASTYM for nearly three yearsbefore being trained in GT. Her clinic was one of the firsttwo in the nation to switch from the ASTYM system to theGraston Technique .Shakar DiscussesGT in PodcastsPT SportsTalker Rehab
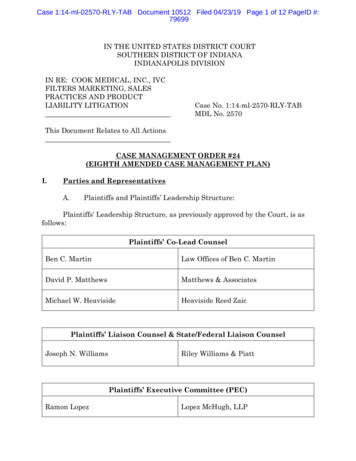
Page 4The EDGECASE REPORTIASTM Used for Treatment of Finger Joint SprainBy Evelina Gundeck, DPT, Amy Bayliss, DPT and M. Terry Loghmani, PT, PhD, Department of Physical Therapy, IU, Indianapolis, INTreatment Protocol:The initial assessment, treatment and reassessment wereperformed by a single GT experienced physical therapist.He was seen during a 6-week period for a total of 6treatment sessions. Significant admit and final findings aresummarized in Table 1. Each treatment session lastedapproximately 30 minutes and consisted of IASTM (10 min)(Figure 2), joint mobilization, therapeutic exercise and icemassage (5 min). His home program included cross-frictionmassage, joint ROM, ice and compression wrapping asneeded.Clinical Outcome:Significant gains in decreased pain, improved function andPIP ROM in a performing artist were achieved using anIASTM treatment approach. Most notably, the patient wasable to play the guitar with minimal to no pain. Demonstratedchanges were likely due to treatment, since the patient hadpain and limitation for 6 months prior to treatment.The most significant limitation of the case study was theinability to isolate the effect of IASTM. Nonetheless, IASTMmay offer a deeper, more specific treatment to the involvedstructures, while providing a mechanical advantage to theclinician.Given the prevalence of upper extremity overusesyndromes and related postural dysfunction in musicians,the use of IASTM provides a promising treatment option.IASTM applications in the performing arts patient populationwarrants future exploration.Figure 2. The tip of GT6 can be used for cross fiber massage to thePIP joint.FINDINGSSubjectiveHistory:A 55-year-old male guitarist presented with pain in the leftindex finger, primarily along the proximal interphalangeal(PIP) joint line due to a fall 6 months prior. He had notreceived any other treatment interventions. X-rays werenegative for fracture. Before and after treatment pictures aredepicted in Figure 1.Figure 1. Initial (A) and discharge (B) hook grip of left index fingerare displayed. Discharge (B) demonstrates significant gain in ROMto near normal.InitialFinalAssessment AssessmentPain rating(scale 0-10)Average: 4/10Average: 1/10DASH score475% disability6.3% disabilityFlex: 80 /85 slight painExt: -20 /-15 Flex: 9 5 /100 no painExt: -5 /0 (R) 85lbs (L) 60lbs(R) 15 lbs (L) 11lbs(R)85lbs (L)78lbs(R)13lbs (L)13 lbsMedium-sizedfibrotic, painfulnodules on forearmflexor surface.Marked tendernessat PIP joint line.Minimal fibrotic,non-painful noduleson forearm flexorsurface. Minimaltenderness atPIP joint line.Active/Passive (L)ROM: PIPObjectiveIntroduction:A guitarist with a chronic finger sprain was treated withinstrument-assisted soft tissue mobilization (IASTM), i.e. theGraston Technique. The purpose of the study was toillustrate how the IASTM multifaceted approach mayimprove the therapeutic outcomes of a musician with achronic index finger joint sprain and meet the treatmentgoals in an efficient and cost-effective manner.Strength:Hook GripLateral Key GripPalpationTable 1. Summary of significant subjective and objectivefindings from initial and final assessments. Decreased painand increased ROM were demonstrated, along with improvedfunction, especially when playing a guitar.REFERENCES1. Loghmani MT, Warden SJ. Instrument-assisted cross fiber massage accelerates kneeligament healing. JOSPT. 39(7): 2009.2. Davidson CJ, Ganion L, Gehlsen G, Roepke J, Verhoestra B, Sevier TL: Morphologic andfunctional changes in rat achilles tendon following collagenase injury and GASTM. Journal of theAmerican College of Sports Medicine 27(5): 1995.3. Sevier TL, Gehlsen GM, Wilson JK, Stover SA, and Helfst RH: Traditional physical therapy vs.Graston Technique Augmented Soft Tissue Mobilization in treatment of lateral epicondylitis.Journal of the American College of Sports Medicine. 27(5): 1995.4. DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or theparts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Handoutcome measure in different regions of the upper extremity. J Hand Ther. 2001 Apr-Jun;14(2):128-46.
Page 5The EDGECASE REPORT25-Year Post-Traumatic Achilles Tendon Injury Has Excellent ResponseBy Larry Smith, BPE, DC, Parksville, British ColumbiaHistory:A 47-year-old malemarina worker initiallypresented withtemporal headachesof a very severenature.After the headaches resolved through traditionalchiropractic treatments, the patient inquired aboutreceiving Graston Technique for a left Achilles tendoninjury. He suffered a complete rupture in the left Achillestendon 25 years earlier and required immediate surgicalrepair. Twelve years later, he stated that he sustainedanother injury to the same ankle and it had been totally“crushed.”Previous treatment during the past 25 years includedmedications such as Tylenol #3, NSAIDS, ultrasound andlaser therapy. He also completed a work-conditioningprogram. None of these treatments seemed to decreasehis pain level or increase ankle function. He complainedof having very little movement in the ankle, was extremelysensitive to touch and had considerable difficulty bearingweight.Exam Findings:Relevant physical examination findings included pelvicasymmetry with the left iliac crest measuring 2 cm lowerthan its right counterpart. There was also a major fixationof the left sacroiliac joint and a minor fixation of the rightsacroiliac joint. Active and passive range of motiondemonstrated moderate to severe decrease ofdorsiflexion, plantarflexion, eversion and inversion of theleft ankle as compared to the right. Joint mobility testingshowed a moderate to severe decrease in talocruralmobility on the left. There was a healed surgical scarlocated on the medial aspect of the Achilles tendon withprominent hypertrophy of the entire tendonous sheath.The patient walked with an obvious limp favoring the leftankle and was unable to perform even one bilateral calfraise (flat feet to toes via plantar flexion). GT examinationrevealed very “gritty” dense scar tissue of the entireAchilles tendon and surrounding sheath and theGastrocnemius-Soleus complex.Treatment Goals:The two major treatment goals were to increase mobilityand function of the left ankle joint and to decrease thepain intensity.Treatment Protocol:With the patient in a prone position, GT4 was used tosweep the plantar fascia and also sweep the Achillestendon, Gastrocnemius-Soleus complex right to the top ofthe knee. The foot was placed in static plantar flexion,dorsi flexion, inversion and eversion. Once adhesionswere isolated, GT3, GT2 and GT6 were used to break upthe restrictions. In addition to the above, GT2 was used tomobilize the soft tissue around the talocrural joint, distaltibiofibular joint and tissues surrounding the medial andlateral malleolus. The GT treatment was followed bystretching in all ranges of motion. The patient wasinstructed to perform these stretches at home, followedby icing.After the first 2 treatments, the patient stated that he hada mild increase of dorsi flexion, plantar flexion, eversionand inversion. He also experienced mild to moderate painand bruising of the left lateral head of gastrocnemius justproximal to his post-surgical scar.After a phone consultation, it was decided to perform thesame GT protocol with added active and passive anklemotion. After the 4th treatment, the patient noticed greatimprovement. He experienced pain relief and was able tomove his foot and ankle without discomfort.The next 5 treatments involved the above protocol plusthe addition of standing on a chair next to the wall andperforming dorsi and plantar flexion. The patient couldonly perform 2-3 repetitions initially, but was able toperform 5-6 repetitions within a few weeks. He also wasinstructed to perform resisted stretching at home withsurgical tubing followed by icing.After 10 treatments, a full re-examination was performed.Objectively, there was a 60-70% increase in all foot andankle ROM and the patient could now perform 6 calfraises without pain. The tissue and musculaturesurrounding the post-surgical scar was no longer tenderContinued on page 6
Page 6The EDGEWhen Changing Treatment, Speed Doesn’t Pay DividendsInstructor Cites Importance of Adhering to GT Princ
elective in 16 chiropractic colleges, the first two of which were added in 2002. Vincent, long an outspoken advocate of chiropractic, gained a large level of acclaim when Massachusetts in 1966, after years of effort, passed a law to license chiropractic. From 1950 to 1966, he practiced his profession in defiance of the Medical Practice Act. His