Transcription
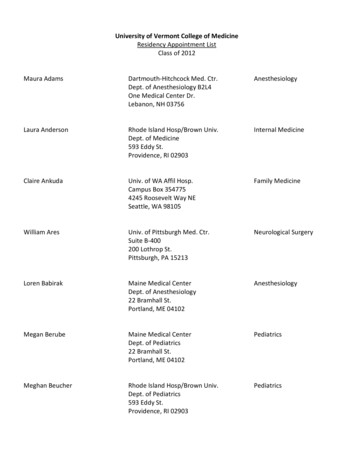
NEUROTRANSMISSIONSSPRING 2018DEPARTMENT OF NEUROLOGYADMINISTRATIONBruce R. Ransom, M.D., Ph.D.Warren and Jermaine Magnuson Professorand Chair,Department of NeurologyService Chief, Neurology,UW Medical CenterMark Wainwright, M.D., Ph.D.Herman and Faye Sarkowsky Chair,Child NeurologyProfessor of Neurology and PediatricsDivision Head, Pediatric Neurology, SeattleChildren’s HospitalWill Longstreth, M.D.Professor of NeurologyService Chief, Neurology,Harborview Medical CenterJana Pettit, M.B.A.DirectorKass KlemzAssistant to the ChairNEUROTRANSMISSIONSEDITORIAL BOARDBruce R. Ransom, M.D., Ph.D.Nicholas P. Poolos, M.D., Ph.D., editor in chiefMegan SchadeDEPARTMENT OF NEUROLOGYUNIVERSITY OF WASHINGTONSCHOOL OF MEDICINE1959 NE Pacific St.RR650 Box 356465Seattle, WA 98195Phone 206.543.2340Fax 206.685.8100depts.washington.edu/neurologFrom the ChairJust as the blossoming trees andincreasing daylight mean that Springhas come to the Pacific Northwest,so too arrives the Spring 2018 issue ofNeurotransmissions, the UW Departmentof Neurology’s newsletter for colleagues,alumni and friends. I am proud to sharethe latest exciting developments in ourdepartment, including news on research,clinical resources, and education.In this issue we spotlight the UWMultiple Sclerosis Center Clinic, basedat Northwest Hospital. The Center isco-directed by Dr. Annette Wundesfrom Neurology and Dr. Gloria Hou fromRehabilitation Medicine. The evaluationand treatment of MS has changed atbreakneck speed in the past 10 years,with the introduction of many newpotent biologic therapies. Dr. Wundesand her team of neurologists, physiatrists,and other allied professionals possessthe expertise to assess each patientwith MS and create an individualizedtreatment plan that best takes advantageof the improved efficacy these noveldrugs offer—whileskirting potentialcomplicationsthey may bring.Read about thistremendous groupof clinicians onpage two.We welcome thenewest memberof UW Neurology leadership on pagefour. Mark Wainwright, MD, PhD hasarrived in Seattle from NorthwesternUniversity in Chicago to take on the roleof Head of Pediatric Neurology at SeattleChildren’s, a position ably filled by SidGospe, MD, PhD for many years untillast June. Mark brings to the Divisionexpertise in pediatric neurocriticalcare, an area that is achieving growingrecognition and importance, especiallywith the increasing use of bedsideelectrophysiological monitoring in theICU setting. Mark is a great additionto our faculty and we look forward tofurther growth in the pediatric divisionunder his leadership.Bruce R. Ransom,MD, PhDContinued on page 8INSIDE THIS , PhDPAGEPAGE45FacultyAwards!a
The UW Multiple Sclerosis Center:at the cutting edge of a rapidly changing fieldThe field of multiple sclerosis (MS)and other CNS demyelinating diseasesis rapidly evolving. The advent ofnewer, more potent disease-modifyingtreatments (DMTs) for MS thathave become available can presenta dizzying array of choices for thenon-specialist clinician. And withnew information that has emerged onthe molecular basis of demyelinatingdisease, MS can now be more readilydifferentiated from its mimics, such asneuromyelitis optica spectrum diseaseor myelin oligodendrocyte glycoprotein(MOG)-antibody associated entities.The UW Medicine Multiple SclerosisCenter is a multi-disciplinary clinicspecialized to meet these challengesposed by patients with MS and otherCNS demyelinating diseases. Since2012, the UW MS Center, at its newlocation at the Northwest Hospitalcampus, has been providing services topatients and collaborating with localproviders across the entire WWAMIregion to address the needs of thiscomplex patient cohort.A team of providers with extensivetraining and experience in MSand related disorders provide acomprehensive focus on the patient,beginning with accurate diagnosis,continuing to optimal DMT choice andmanagement, and including symptommanagement and rehabilitation. Theysee patients ranging from those atinitial diagnosis to those with veryadvanced disease; every effort is madeto address their individual needsaccording to their disease stage andseverity. The UW MS Center’s teamconsists of neurologists with expertise2 DEPARTMENT OF NEUROLOGYThe UW MS Center proudly supports the annual MS Walk in Seattle, and hasbeen awarded the “Largest Team Award” for multiple years in a rowin MS, a rehabilitation physician,a nurse practitioner, a vocationalcounselor, a social worker, MStrained nurses, infusion nurses, and apharmacist. A dedicated infusion suiteand pharmacy are integrated partsof the UW MS Center. A monthlypatient program available on-site andby webinar is offered. Because of thebreadth of clinical expertise available,the National MS Society has awardedthe UW MS Center the “Partners inMS Care” designation for the highestlevel of comprehensive MS care.and Annette Wundes, MD, AssociateProfessor of Neurology and co-directorof the UW MS Center, to guide patientsand partnering community providerstowards an individualized treatmentplan. Pamela Davies, ARNP, TeachingAssociate of Neurology, with extensiveexperience in chronic pain and chronicdisease management, has recently joinedthe team for optimal management andsafety surveillance of patients. Ourpharmacist Deborah Gallaro, RPh,supports providers and patients alikeregarding complex medication regimens.Disease modifying strategies for MShave become quite complex: neweragents offer opportunities to optimizedisease control, but may pose greaterrisks. Here a thorough analysis ofpatient-specific disease trajectory inthe context of patients’ other healthinformation allows our neurologistsGloria von Geldern, MD, AssistantProfessor of Neurology, MichaelPersenaire, MD, Acting Instructor ofNeurology, Gary Stobbe, MD, ClinicalAssociate Professor of Neurology,The neurology team works directly withother faculty of the interdisciplinaryteam, including physiatrist Gloria Hou,MD, co-director of the UW MS Center,rehabilitation psychologists KevinAlshuler, PhD, Adjunct AssistantProfessor of Neurology, SamanthaArtherholt, PhD, Tiara Dillworth, PhD,as well as vocational counselor JoeStuckey. Patients may be co-managedwith any of these providers for optimalpatient outcome. Community providerstaking care of patients with MS canContinued on page 8
Swanson’s History of NeurologyThe Bronze Age of UW Neurology: Part 4, 1975- 1980s.By Phillip D. Swanson, MD, PhD,Professor of NeurologyIn the 1970s, after one year of trainingin internal medicine and three years ofclinical neurology, neurologists usuallywould opt either for private practice orfor an academic career. Those planningfor an academic career often applied forfurther research fellowship training to beprepared to do both research and clinicalwork. In those days, at the University ofWashington, there was only one academictrack towards promotion, now calledthe clinician/scientist track. There arenow additional clinician/teacher, andclinician tracks. So in the early 1970s,most academic neurologists managedevery type of neurologic disorder in theclinics or on the wards. Changes tothis pattern occurred quite gradually, sothat at the present time it has becomethe norm for a neurological resident toseek fellowship training in a clinicalsubspecialty, such as multiple sclerosis orclinical neurophysiology, before movingon to practicing. At the University ofWashington, establishment of some ofthese subspecialties had to wait until theNeurology division became a departmentin 1996, as the need for appropriatelytrained faculty members had not yetbeen met.Neuro-oncology. Dr. Alexander (Alex)Spence joined the Division in 1974. Agraduate of the University of ChicagoSchool of Medicine, he trained as aneurologist in the Harvard Longwoodprogram, followed by a stint of militaryservice. He was doing a neuropathologyfellowship at Stanford, where he becameinterested in the pathogenesis of primarybrain tumors. He became the firstneuro-oncologist at the University ofWashington. Alex joined the Divisionat about the time that Richard Nixonresigned from the U.S. presidency. AlexSpence was a superb clinician and adevoted researcher into the pathogenesisof brain tumors. He developed a model ofglioma in the rat, using tumor-inducingchemicals. He studied tumor metabolismusing PET scanning techniques, and thenbegan studies in humans, measuring tumormetabolism and the effects of treatments.He gained the respect of neurosurgeonsand radiation oncologists, and led theweekly tumor board meetings. His loss in2010 was deeply felt. Several neurologyresidents, including Rich Peterson, SoniaPartap, and Brian Vaillant, were inspiredby Alex to enter the field of neurooncology.disorders affectingthe neuromuscularand central nervoussystems. Manypreviously unreportedconditions have beenstudied in the clinic,including the findingof novel mutations forAlexander Spence, MDCharcot-Marie-ToothDisease, familial Alzheimer Disease, andspinocerebellar ataxias. Tom became Chiefof Neurology at the Seattle VA Hospitalin 1987, serving until 1997 when he wassucceeded by Bill Spain. Both SumieJayadev and Marie Davis were mentored byTom. (Please see page 7 for an additionaltribute to Tom.)Neurogenetics. Tom Bird finished hisMovement disorders. The finding in theneurology residency in 1974. He was agraduate of Cornell School of Medicine,and in 1970 started his training in Seattleas a rotating intern at the UniversityHospital. After his N1 year he was requiredto fulfill his military service obligation,having been deferred until then underthe Berry Plan. After two years at theNaval Hospital in San Diego, he returnedto Seattle and completed his residency.He then took the unusual (at that time)step of undergoing fellowship training inmedical genetics under Arno Motulsky,one of the founders of this field. Tomthen began his illustrious career withjoint appointments in the Divisions ofNeurology and Medical Genetics. Thoughhe was a full-time employee of the VAMC,at the UWMC he was allowed to establishthe first neurogenetics clinic in the USas a unique resource for neurologicalpatients with genetic diseases. This cliniccontinues to evaluate patients with geneticlate 1960s that levodopa could remarkablyimprove the symptoms of patients withParkinson’s Disease led to a worldwideexpansion of interest in movementdisorders. Before this time, medical therapyconsisted primarily of anticholinergicmedications such as trihexyphenidyl,although neurosurgical procedures suchas thalamotomy were often successfulin improving tremor, limb rigidity, andbradykinesia. At the UW, we participatedin clinical trials of other drugs acting toenhance dopaminergic activity, such asentacapone and ropinirole. We established aParkinson’s Information and Referral Centersponsored by the American ParkinsonDisease Association, which allowed thehiring of Maria Linde, a NeurologicalNurse Specialist who was instrumental inestablishing a local Parkinson’s chapter andpatient support groups. With the discoveryof the genetic mutation causing HuntingtonDisease, HD could now be diagnosedContinued on page 43
Update from the Division of Pediatric NeurologyWELCOMING MARK WAINWRIGHT, MD, PHD, DIVISION HEADPeter Huttenlocher, one of the greatfigures of child neurology.“I watched him get on the floor andplay with the kids with blocks, andrealized, that’s the kind of neurology Iwanted to do,” he said.Beginning in December 2017, MarkWainwright, MD, PhD, Professorof Neurology, became Head of theDivision of Pediatric Neurology,succeeding long-time Head SidGospe, MD, PhD, who retired inJune 2017. He originally hails fromLiverpool, England, and was motivatedto emigrate to the US for love: as acollege student, he met his futurewife in England while she was on anexchange program from the Universityof Rochester. In the US, he entered anMD/PhD program at the Universityof Chicago and pursued doctoralresearch on the molecular properties ofthe dopamine receptor. As a medicalstudent doing clinical rotations, he hadthe good fortune to be on-service withFollowing his graduation from Chicago,Dr. Wainwright entered the childneurology program at Duke. During hislast year in the program, he discoveredhe enjoyed practicing in the intensivecare environment, and also developeda research interest in neuroprotectionin critically ill children. Following hisrecruitment to Northwestern University(where he remained from 2000 untilhis move to the UW), he started a labfocused on neuroinflammation andtraumatic brain injury. In parallel, hestarted a pediatric neurocritical careprogram at Northwestern, which grewfrom a one-person operation to sixfaculty, a busy consult service, and atraining program which now trains twofellows each year. “Neurological issuesimpact every child in the ICU,” hesaid, “and what was key to our successwas building a partnership betweenneurologists and intensivists.”Dr. Wainwright came to SeattleChildren’s because he saw anopportunity “to build on strengths in analready excellent division.” Neurocriticalcare is one such area where he hopesto recapitulate his success story atNorthwestern. He cites other potentialgrowth opportunities in pediatricneuromuscular disease, neuro-oncology,and demyelinating disorders. A novelclinical and research focus will be ona “big data” approach to monitoringchildren in the ICU using real-timestreaming of multiple lines of physiologicdata, so to predict those patients at riskfor impending clinical deterioration.Since moving to Seattle from Chicago—albeit just in time for the dreary PacificNorthwest winter—he does laud theclimate for being appreciably milderthan that of the Windy City. Anotherdifference he noted was the fact that“people stop to let you cross the street—bizarre!” While getting a feel for theDivision and setting up a home inanticipation of the move of his wife andpossibly his two daughters in their 20s aswell to Seattle, Dr. Wainwright does nothave much free time at present. But heis harboring ambitions of taking up thebagpipes, so to import a bit of the UK tothe PNW.Continued from page 3definitively. Developing a movementdisorders program with fellowship traininghad to wait until Dr. Ali Samii joined usin 1996.Clinical neurophysiology. Withthe exception of Children’s Hospital,where Coldevin Carlson carried outelectromyography (EMG) on children,4 DEPARTMENT OF NEUROLOGYEMGs on the adult services were allperformed by the Department of PhysicalMedicine and Rehabilitation (nowRehabilitation Medicine). Neurologyresidents were welcomed for EMG trainingby Drs. Walter Stolov and George Kraft.For full fellowship training, however,trainees usually went elsewhere to programsat UCSD or University of Utah. Notuntil departmental status was achievedin 1996 was Neurology allowed to carryout EMGs. The first EMGer hired by theDepartment was Dr. Eric Yuen. He wassucceeded by Michael Weiss in 2001. Dr.Weiss has expanded the EMG services withthe help of Drs. B. Jane Distad, Eric Kraus,and Leo Wang, sharing the studies withRehabilitation Medicine.
Neurology Residency UpdateWe congratulate the 2018 graduating class of Neurology residents! We thought, How better to send them off into the world offellowship or practice than to give them each a parting shot? Below, we bring you our diverse cast of uniquely talented neurologists!Thomas Foutz, MDAnusha Mannava, MDEPILEPSY FELLOWSHIP,UNIVERSITY OFNORTH CAROLINAHEADACHEFELLOWSHIP, UWI’m so grateful to everyone for the support andeducation I have received these 5 (long) years. Ithas been an marvelous, arduous and life-alteringjourney. I will not miss Q4 call, but will miss prettymuch everything else. My wife, our three kids, andI will be moving to Chapel Hill, North Carolina forEpilepsy fellowship.Coming to UW as an R2 as opposed to other neuroresidents was scary initially, but soon realized not tobe! It’s been a smooth journey and was only possiblethrough the immense support of colleagues, seniorsand attendings. I am glad to stay back as a Headachefellow and cherish one more year of being with someof these awesome people!James Wang, MDVASCULAR NEUROLOGYFELLOWSHIP, UWThank you to everyone in the Department ofNeurology that have taught and shaped us intothe neurologists that we are today. Best to all goingforward. Cheers!Yujie Wang, MDHuan Li, MD, PhDGENERAL NEUROLOGYPRACTICE,KADLEC REGIONALMEDICAL CENTERWe came from near and farTo form a great teamAs proud neuro residentsTo pursue the same dreamWe have amazing attendingsWho help us take flightGreat neurologists we’ll becomeRising together to show our mightHand in hand we can laugh and cryStill working hard in all this timeAchieving objectivesOur work is sublimeGraduation’s coming soon,Lift your hands up to the skyWe grew our wings and now we fly!Anisha ChandraSchwarz, MDNEUROMUSCULARFELLOWSHIP, UWIt turns out that pediatric neurology residency isa wonderful thing to have done. Thanks to all thepatients (ages one minute to ninety years), mentors,and peers who taught me, encouraged me, andshaped the past five years. What an amazing groupI trained with. You made it worthwhile to come inevery day. Favorite attending remark: “It is better toround with an empty bladder than a full mind.”(Dr. Kollros). I’m looking forward to neuromuscularfellowship at UW next year. Do keep in touch, andplease keep sending me good papers. I have plans toread them.Thanks for the memories UW, it was a blast.Residency has flown by, from the first Botoxinjection at the VA to the last Stroke Code atHarborview. It has been quite a rewarding andhumbling experience, and I will forever be gratefulto my co-residents and the faculty members forbeing there every step of the way. It is bittersweetto be leaving Seattle and the UW Neurology family,but I know that I have made lifelong colleaguesand friends. For the next step of my career, I will bepursuing a fellowship in Neuro-immunology, andam excited to continue to learn.Jennifer Wax, MDBreana Taylor, MDHEADACHE FELLOWSHIP,UWVASCULAR NEUROLOGYFELLOWSHIP, UWJustin Low, MDNEURO-ONCOLOGYFELLOWSHIP, DUKENEURO-IMMUNOLOGYFELLOWSHIP,JOHNS HOPKINSAt first it was a big adjustment moving to Seattle fromChicago, but my co-residents and incredible facultyteachers and mentors have made my experienceat UW unforgettable. I am excited for the VascularNeurology fellowship next year. I am thankful for theopportunity to continue to grow, and become the bestneurologist I can!Thank you to my co-residents and many facultymentors for their support during residency. Andthank you to my family, without whom I'd neverhave made it to - much less through - these pastfew years. Another doctor once said, "all of timeand space.where do you want to start?" I'mgrateful to have received my start in neurology atUWMC, and to be continuing the journey as oneof the Headache fellows next year.5
Selected Recent Publications by Neurology FacultyCompiled by Nadine Waldmann,Budget/fiscal analyst leadNovotny EJ Jr. Early genetic testing forneonatal epilepsy: When, why, and how?Neurology. 2017.Berg AT, Coryell J, Saneto RP, Grinspan ZM,Alexander JJ, Kekis M, Sullivan JE, WirrellEC, Shellhaas RA, Mytinger JR, GaillardWD, Kossoff EH, Valencia I, Knupp KG,Wusthoff C, Keator C, Dobyns WB, Ryan N,Loddenkemper T, Chu CJ, Novotny EJ Jr, KohS. Early-Life Epilepsies and the Emerging Roleof Genetic Testing. JAMA Pediatr 2017.Wang AC, Ibrahim GM, Poliakov AV, Wang PI,Fallah A, Mathern GW, Buckley RT, Collins K,Weil AG, Shurtleff HA, Warner MH, Perez FA,Shaw DW, Wright JN, Saneto RP, Novotny EJ,Lee A, Browd SR, Ojemann JG. Corticospinaltract atrophy and motor fMRI predictmotor preservation after functional cerebralhemispherectomy. J Neurosurg Pediatr 2018.Weaver KE, Poliakov A, Novotny EJ,Olson JD, Grabowski TJ, Ojemann JG.Electrocorticography and the early maturationof high-frequency suppression within thedefault mode network. J Neurosurg Pediatr 2018.Grinspan ZM, Shellhaas RA, Coryell J, SullivanJE, Wirrell EC, Mytinger J
DEPaRTMENT OF NEUROLOGY UNIVERSITY OF WaSHINGTON SCHOOL OF MEDICINE 1959 NE Pacific St. RR650 Box 356465 Seattle, Wa 98195 Phone 206.543.2340 Fax 206.685.8100 depts.washington.edu/neurolog DEPaRTMENT OF NEUROLOGY aDMINISTR aTION SPRING 2018 INSIDE THIS ISSUE PaGE 2 Faculty Awards! Multiple Sclerosis Clinic PaGE 5 Continued on page 8