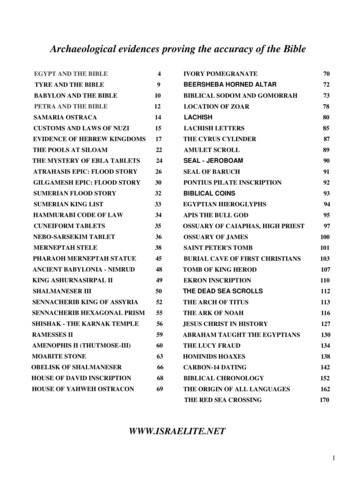
Transcription
ARTICLEAccuracy of the Barrett True-K formulafor intraocular lens power prediction afterlaser in situ keratomileusis or photorefractivekeratectomy for myopiaAdi Abulafia, MD, Warren E. Hill, MD, Douglas D. Koch, MD, Li Wang, MD, PhD,Graham D. Barrett, MDPURPOSE: To compare the accuracy of the Barrett True-K formula with other methods available onthe American Society of Cataract and Refractive Surgery (ASCRS) post-refractive surgeryintraocular lens (IOL) power calculator for the prediction of IOL power after previous myopiclaser in situ keratomileusis (LASIK) or photorefractive keratectomy (PRK).SETTING: Cullen Eye Institute, Baylor College of Medicine, Houston, Texas, and private practice,Mesa, Arizona, USA.DESIGN: Retrospective case series.METHODS: The accuracy of the Barrett True-K formula was compared with the Adjusted Atlas(4.0 mm zone), Masket, modified-Masket, Wang-Koch-Maloney, Shammas, and Haigis-Lmethods to calculate IOL power. A separate analysis of 2 no-history methods (Shammas andHaigis-L) was performed and compared with the Barrett True-K no-history option.RESULTS: Eighty-eight eyes were available for analysis. The Barrett True-K formula had asignificantly smaller median absolute refraction prediction error than all other formulas exceptthe Masket, smaller variances compared with the Wang-Koch-Maloney, Shammas, and Haigis-L,and a greater percentage of eyes within G0.50 diopter (D) of predicted error in refractioncompared with the Adjusted Atlas, Masket, and modified Masket methods (all P .05). In eyeswith no historical data, the Barrett True-K no-history formula had a significantly smaller medianabsolute refraction prediction error and a greater percentage of eyes within G0.50 D of thepredicted error in refraction than the Shammas and the Haigis-L formulas (both P .05).CONCLUSION: The Barrett True-K formula was either equal to or better than alternative methodsavailable on the ASCRS online calculator for predicting IOL power in eyes with previous myopicLASIK or PRK.Financial Disclosures: Dr. Barrett has licensed the Barrett True-K formula to Haag-Streit. Dr. Hill isa paid consultant to Haag-Streit and Alcon Surgical, Inc. None of the other authors has a financial orproprietary interest in any material or method mentioned.J Cataract Refract Surg 2016; 42:363–369 Q 2016 ASCRS and ESCRSIntraocular lens (IOL) power calculations for patientswho have had refractive myopic correction surgeryare a clinical challenge of growing importance.1–4The sources of the prediction errors in these eyes arewell known.1,5,6 Nevertheless, IOL power predictionfor these eyes remains problematic.7,8 The use of multiple formulas or calculations for these eyes can beQ 2016 ASCRS and ESCRSPublished by Elsevier Inc.difficult to execute and time consuming. The AmericanSociety of Cataract and Refractive Surgery (ASCRS)online calculatorA was developed to facilitate this process. An evaluation of the post-myopic laser in situkeratomileusis (LASIK) or photorefractive keratectomy (PRK) ASCRS calculator2 led to a recent revisionthat excluded methods that require pre-LASIK or 6-3350363
364BARRETT TRUE-K FORMULA FOR PREDICTING IOL POWER AFTER LASIK OR PRKkeratometry and included some new promisingmethods, such as the Potvin-Hill Scheimpflug device(Pentacam, Oculus),8 optical coherence tomography(OCT)–based formulas,7,9 and the Barrett True-Kformula.7,BThe Barrett True-K formula is based on the BarrettUniversal II formula.10 It calculates a modified keratometry (K) value for patients who have had myopicor hyperopic LASIK or PRK or radial keratotomy(RK) and requires the measured keratometries andthe before and after laser refraction values. It also provides a double-K solution5,6 to address the problem ofaccurately calculating corneal height when central keratometries have been altered. In addition, the formulacan predict the required power of the IOL when norefractive history is available (no-history formula).The purpose of this study was to compare theBarrett True-K formula with the current methodsavailable on the updated online ASCRS IOL powercalculator.PATIENTS AND METHODSStudy Groups and ProtocolThis retrospective case series was performed with ethicscommittee approval. The case records of consecutive patients who had previously had LASIK or PRK for myopiaand subsequently had cataract surgery between December22, 2008, and February 28, 2013, at East Valley Ophthalmology, Mesa, Arizona, USA (Center 1, pooled data), andbetween January 2010 and November 2013 at the Baylor College of Medicine, Houston, Texas, USA (Center 2, 1 surgeon,D.D.K.), were reviewed. Inclusion criteria were no complications during or after cataract surgery, corrected distancevisual acuity of 20/32 or better measured at least 3 weeksafter surgery, and availability of manifest refraction valuesbefore and after LASIK or PRK (Center 1). Patients whohad a Crystalens IOL (Bausch & Lomb) implanted wereexcluded from the study because of concerns about the predictability of the effective lens position. Cataract surgerieswere performed using a temporal clear corneal incisionand phacoemulsification. Various methods were used forcorneal power estimation and IOL power calculation beforesurgery. The surgeon used his judgment to select the IOL power to be implanted.Submitted: June 12, 2015.Final revision submitted: November 9, 2015.Accepted: November 22, 2015.From the Department of Ophthalmology, Assaf Harofeh MedicalCenter, Zerifin, and the Ein-Tal Eye Center (Abulafia), Tel-Aviv,Israel; East Valley Ophthalmology (Hill), Mesa, Arizona, and theCullen Eye Institute (Koch, Wang), Baylor College of Medicine,Houston, Texas, USA; The Lions Eye Institute (Barrett), Nedlands,Western Australia, Australia.Corresponding author: Adi Abulafia, MD, Department of Ophthalmology, Assaf Harofeh Medical Center, Zerifin, Israel. E-mail: adi.abulafia@gmail.com.METHODSThe Adjusted Atlas 9000 method (4.0 mm zone),C Masketformula,11 Modified Masket formula,D Wang/Koch/Maloney formula,C Shammas with regression analysis,12 HaigisL formula,13 Barrett True-K formula7,B and the average valueof all formulas (average) were evaluated. The Potvin-HillScheimpflug device and the OCT-based formulas were notincluded because the data required for these methods werenot available.The Barrett True-K formula can be used with or withoutconsidering the surgically induced change in refraction(change in manifest refraction) because it uses an internalregression formula to calculate an estimated change in manifest refraction when those data are not entered. However,this internal regression formula was partly derived fromdata in the database of Center 1. Therefore, patients weredivided into 2 groups; that is, Group A from Center 1 andGroup B from Center 2. All formulas or methods were evaluated for Group A, and the Barrett True-K formula wascompared with the Shammas and Haigis-L no-history formulas (ie, using no change in manifest refraction data) inGroup B. A mean prediction error was calculated for eachgroup.The error in the predicted refraction was calculated as thedifference between the actual postoperative refractiveoutcome and the predicted refraction for each formula ormethod. The mean numerical error, median absolute error,mean absolute error, and percentages of eyes within G0.50diopter (D) and G1.00 D from the target refraction werecalculated for each formula or method.Statistical AnalysisThe 1-sample t test was used to determine whether themean numerical refraction prediction errors produced bythe various methods were significantly different fromzero. Analysis of variance was performed to compare differences in refractive prediction errors between methods.The variances in the mean numerical refractive predictionerrors were tested using the Fisher F test for variances toassess the consistency of the prediction performance bydifferent methods. The absolute refractive prediction errors were evaluated using the Wilcoxon signed-rank test.The percentages of eyes within certain refractive prediction errors were compared using the chi-square test orthe Fisher exact test, as appropriate. The Bonferronicorrection was applied for multiple tests. Statistical analyses were performed with the Xlstat (version 2014.2.03,Addinsoft) and Sigmaplot (version 12.5, Systat Software,Inc.). A P value less than 0.05 was considered statisticallysignificant.RESULTSThe study included 88 eyes of 66 patients. GroupA had 58 eyes of 40 patients with an availablechange in manifest refraction data. Group B included30 eyes of 26 patients. Table 1 shows the patients'demographics.Refractive Prediction ErrorFigure 1 shows boxplots of the refractive predictionerrors according to the various methods. The meanJ CATARACT REFRACT SURG - VOL 42, MARCH 2016
365BARRETT TRUE-K FORMULA FOR PREDICTING IOL POWER AFTER LASIK OR PRKTable 1. Patient demographics.Group A (n Z 58)ParameterMean G SDAge (y)Pre-LASIK/PRK MRSE (D)Post-LASIK/PRK MRSE (D)Refractive correction (D)Axial length (mm)IOL power implanted (D)Post-cataract MRSE (D)*5.49 G 2.890.43 G 0.845.06 G 2.8925.85 G 1.3519.83 G 2.450.45 G 0.85Group B (n Z 30)Range*13.38, 0.632.00, 2.500.75, 14.0023.22, 28.3313.00, 26.503.00, 1.25Mean G SDRange58 G 7ddd25.69 G 1.2520.27 G 2.220.83 G 0.9034, 73ddd23.22, 28.9314.00, 25.002.88, 0.75IOL Z intraocular lens; LASIK Z laser in situ keratomileusis; MRSE Z manifest refraction spherical equivalent; PRK Z photorefractive keratectomy*Data not availableFigure 1. Refractive predictionerrors with the various testedcalculating methods in Group A(top) and Group B (bottom). The1-sample t test was used to determine whether the mean numerical refraction prediction errorsproduced by the various methodswere significantly different fromzero (P values are presented foreach method).J CATARACT REFRACT SURG - VOL 42, MARCH 2016
366BARRETT TRUE-K FORMULA FOR PREDICTING IOL POWER AFTER LASIK OR PRKTable 2. Mean numerical errors, mean absolute errors, and median absolute errors in all eyes in Group A with inclusion of previous refractive data (n Z 58).Refraction Prediction Error (D)NumericalFormula/MethodAdjusted AtlasMasketModified eMean G SD0.15 G 0.640.10 G 0.640.20 G 0.630.16 G 0.830.13 G 0.770.34 G 0.740.01 G 0.550.04 G 0.62AbsoluteRangeMean G SDMedianRange1.15, 1.641.26, 1.591.69, 1.161.52, 2.961.57, 2.871.65, 2.860.96, 1.531.24, 2.020.51 G 0.410.48 G 0.440.52 G 0.410.63 G 0.560.60 G 0.510.63 G 0.510.43 G 0.360.46 G 0.410.380.320.480.530.460.580.330.340.01, 1.640.01, 1.590.01, 1.690.02, 2.960.00, 2.870.00, 2.860.00, 1.530.00, 2.02Haigis-L (P Z .034) formulas. There were no significant differences between the various methods inGroup B (P Z .905) (Table 4).numerical error values in Group A ranged from 0.34to 0.16 D. The mean numerical errors were not significantly different from zero except for the modifiedMasket (P Z .021) and the Haigis-L (P ! .001)methods. The median absolute error ranged from0.32 to 0.58 D. The Barrett True-K median absolute error was significantly lower than the median absoluteerrors of all other methods (range P Z .002 toP Z .031) and similar to the Masket formula(P Z .09) and the average value (P Z .486) (Table 2).The mean numerical error values in Group B rangedfrom 0.20 to 0.50 D. The Shammas (P Z .017), theHaigis-L (P ! .001), and the average prediction errorvalue (P Z .020) produced a mean numerical errorthat was significantly different from zero. The medianabsolute errors ranged from 0.41 to 0.62 D. The BarrettTrue-K had the lowest median absolute error of allother tested methods (P Z .01) (Table 3).Refractive Prediction Error Within 0.50 Diopterand 1.00 DiopterIn Group A, the percentage of eyes with a refractiveprediction error within G0.50 D was significantlyhigher with the Barrett True-K formula than with theAdjusted Atlas, Masket, modified Masket, andaverage formulas (all P ! .001). Also, the percentageof eyes with a refractive prediction error withinG1.00 D was significantly higher with the BarrettTrue-K formula than with the Adjusted Atlas(P Z .001), Masket (P Z .003), Wang/Koch/Maloney(P Z .005), Shammas (P Z .004), and average(P ! .001) formulas (Table 5). In Group B, the percentage of eyes with a refractive prediction error withinG0.50 D was significantly higher with the BarrettTrue-K formula than with all other cited methods(P % .002), whereas the percentage of eyes withinG1.00 D was highest using the average value(P ! .001) (Table 5).Variances in Refractive Numerical Prediction ErrorThe variance for the Barrett True-K formula inGroup A was significantly lower than for the Wang/Koch/Maloney (P Z .003), Shammas (P Z .013), andTable 3. Mean numerical errors, mean absolute errors, and median absolute errors in all eyes in Group B for which previous refractive datawere not available (n Z 30).Refraction Prediction Error erage (mean)Mean G SD0.34 G 0.720.50 G 0.650.20 G 0.640.31 G 0.67AbsoluteRangeMean G SDMedianRange1.75, 1.461.94, 1.031.55, 1.281.72, 1.320.63 G 0.480.68 G 0.450.52 G 0.430.59 G 0.440.530.620.410.530.01, 1.750.14, 1.940.00, 1.550.02, 1.72*Barrett true-K no history methodJ CATARACT REFRACT SURG - VOL 42, MARCH 2016
367BARRETT TRUE-K FORMULA FOR PREDICTING IOL POWER AFTER LASIK OR PRKTable 4. Variances in numerical refractive prediction errors.Variance (D2)Formula/MethodAdjusted AtlasMasketModified MasketWang/Koch/MaloneyShammasHaigis-LBarrett True-KAverageGroup A(n Z 58)Group B(n Z 10.45DISCUSSIONDetermining the most appropriate IOL power for eyesthat had previous corneal refractive surgery is challenging. Various methods have been proposed toaddress the relative lack of predictability in postLASIK or PRK myopic eyes.1,2,4,6–8,11–20 Hill et al.Adeveloped an Internet-based IOL power calculatorfor eyes with a history of LASIK, PRK, or RK to eliminate the need to perform multiple calculations foreach case.2 The online calculator has recently been updated, with less predictable methods having beeneliminated and several new methods of calculationincluded. The purpose of the current study was toevaluate 1 of those methods, the Barrett True-K formula, in comparison with alternative formulasincluded in the online calculator.All methods except for the modified Masket andHaigis-L produced mean numerical errors close tozero in Group A. Those 2 exceptions had a negativemean numerical error, with a tendency toward myopicoutcomes. All methods except the Barrett True-K formula had a significant negative mean numerical errorin Group B. Our data suggest that the IOL constantsfor those formulas might need minor adjustment forthe 2 centers. Nevertheless, the spread of a refractiveprediction error of a formula provides more meaningful information regarding its accuracy. In Group A, thevariance for the Barrett True-K was significantly lowerthan for the Wang/Koch/Maloney, Shammas, andHaigis-L formulas. In Group B, there were no significant differences in the variance between the differentmethods. Our data therefore suggest that the BarrettTrue-K is at least as accurate as the other formulastested.The introduction of partial coherence interferometrytechnology21 has improved the predictability of IOLpower calculation formulas, yielding a low predictionerror with a maximum absolute deviation from thetarget refraction of G0.50 D in 71% of eyes andG1.00 D in 93% of eyes.22 The Barrett True-K formulawith a change in manifest refraction data had the highest percentages of eyes with a refractive prediction error within G0.50 D and G1.00 D (67.2% and 94.8%,respectively) compared with all other methods. Itwas the only formula that was close to these updatedbenchmark criteria, suggesting that the prediction ofthe appropriate IOL power in this population is stillfar from optimum.In general, in our study the percentage of eyeswithin G0.50 D and G1.00 D of the refractive prediction error seems to be slightly worse than the values reported in a study by Wang et al.2 but slightly betterthan those in a study by Potvin and Hill.8 In comparison with the figures in the literature, in our study thepercentage of eyes within G0.50 D and G1.00 D ofthe refractive prediction error seems to be betterthan,23 worse than,13,18 or comparable to3 those forthe Haigis-L and the Shammas formulas. The differences are probably related to differences in the studiedpopulation groups. Different formulas have to beTable 5. Percentage of eyes within G0.50 D and G1.00 D from the target refraction in Groups A and B.PercentageGroup A (n Z 58)Formula/MethodAdjusted AtlasMasketModified eGroup B (n Z 30)Within G0.50 DWithin G1.00 DWithin 0.50 DWithin G1.00 083.3J CATARACT REFRACT SURG - VOL 42, MARCH 2016
368BARRETT TRUE-K FORMULA FOR PREDICTING IOL POWER AFTER LASIK OR PRKcompared on the same dataset for a valid analysis ofrelative predictability.One limitation of our study is that the BarrettTrue-K formula was not tested both with andwithout a change in manifest refraction data for thesame patients. This limitation arises from the retrospective nature of this study in which eyes fromCenter 1 were used to generate a regression analysisto determine a predicted refractive change of the procedure based on the measured parameters for theBarrett True-K formula when the change in manifestrefraction is not available. Another limitation of ourstudy is that new formulas that use direct measurements of the posterior cornea were not evaluatedbecause those data were not available for our studypopulation. A third limitation of our study is that itwas confined to formulas and methods available onthe ASCRS online calculator. Further studies thatcompare the Barrett True-K formula with andwithout a change in manifest refraction informationwith additional formulas and methods includingray tracing15 and intraoperative aberrometry4,14 arewarranted. Finally, no subgroup prediction analysiswas performed for eyes with different axial lengthsand mean K values.In conclusion, our results show that for eyes withprevious myopic LASIK or PRK correction, the BarrettTrue-K formula gave results better than or similar tothose of various methods and formulas from theASCRS online calculator. Further studies are neededto evaluate the Barrett True-K formula in eyes thathad previous RK or hyperopic LASIK or PRK.WHAT WAS KNOWN Determining IOL power for eyes that have had cornealrefractive surgery is difficult compared with current accuracy standards for virgin eyes. Methods that use corneal measurements at the time ofpresentation for cataract surgery, either with or withoutknowledge of surgically induced changes in refraction,are more accurate than methods that rely solely on preLASIK or PRK K values and surgically induced changesin refraction for calculating corneal power.WHAT THIS PAPER ADDS The Barrett True-K formula was applicable for eyes with orwithout previous data of the surgically induced changes inrefraction. The Barrett True-K formula gave better or similar resultsto those with various methods and formulas from theASCRS online calculator.REFERENCES1. Hoffer KJ. Intraocular lens power calculation after previouslaser refractive surgery. J Cataract Refract Surg 2009;35:759–7652. Wang L, Hill WE, Koch DD. Evaluation of intraocular lenspower prediction methods using the American Society of Cataract and Refractive Surgeons post-keratorefractive intraocularlens power calculator. J Cataract Refract Surg 2010; 36:1466–14733. McCarthy M, Gavanski GM, Paton KE, Holland SP. Intraocularlens power calculations after myopic laser refractive surgery: acomparison of methods in 173 eyes. Ophthalmology 2011;118:940–9444. Ianchulev T, Hoffer KJ, Yoo SH, Chang DF, Breen M, Padrick
the American Society of Cataract and Refractive Surgery (ASCRS) post-refractive surgery intraocular lens (IOL) power calculator for the prediction of IOL power after previous myopic laser in situ keratomileusis (LASIK) or photorefractive keratectomy (PRK). SETTING: Cullen Eye Institute, Ba