Transcription
TOOL KITPatient Controlled Analgesia(PCA) Guidelines of CareFor the Opioid Naïve PatientRevised: December 2009May 2014 (Disclaimer updated)
About This DocumentThe purpose of this document is to provide San Diego County Acute Care settings with recommendations for thestandardization of intravenous Patient Controlled Analgesia (PCA) medication administration in the care of theopioid naïve patient. These recommendations exclude the use of epidural PCA (PCEA), subcutaneous PCA use, thepalliative care environment, and patients experiencing chronic pain.Intended AudienceThe document is intended for the Acute Care Clinical Leader.Organization of This DocumentThe document is organized into two main sections: recommended clinical guidelines for Opioid PCA usage, andrecommended plan for implementing the guidelines in your institution.AcknowledgementThe San Diego Patient Safety Council wishes to acknowledge the financial contribution and in-kind supportprovided by Cardinal Health, Inc./CareFusion, as well as each of the institutions listed on the cover thatcontributed the valuable time of its expert clinicians in the creation of this document.San Diego Patient Safety Council: PCA MembersFacilitator: Nancy Pratt, RN, MSN, Senior Vice President, Clinical Effectiveness, Sharp HealthCareAlvarado HospitalPalomar Pomerado HealthSharp HealthCarePeg Tilley, RN, BSNDiana Schultz, RPh, MHSAJohn H. Eastham, PharmDCatherine Konyn, RN, CNSBunny Krall, RN, MSN, CNSCheryl Dailey, RN, MSJohn Engelbert, PharmDSteve Leary, RNPaul Neves, RNAlbert Rizos, PharmDCareFusionSteve Lewis, MDTim Vanderveen, PharmD, MSHospital Association of San Diegoand Imperial CountiesSapna Dharkar-Surber, MPHNaval Medical Center San DiegoYuet-Hing Lam, RPhRady Children’s Hospital San DiegoRebecca Bennett, RN, PNPCharles "Rich" Richards, PharmDScripps HealthSusan Dempsey, RN, MN, CNSChristine Low, PharmDMark Parmenter, PharmDContentsUCSDJulie Abraham, PharmDDiana Jung, PharmDVA Healthcare San DiegoJennifer Howard, PharmDKimberly Quicci-Roberts, MSKaren Carroll, RN, MS, CNSIntroduction . 3Current State . 3Goal Charter . 4Performance Improvement . 4The Pain Management Process . 4Guidelines for PCA Usage. 5Starting Standard Orders. 5Conversion Instruction/Table . 6Assessment for PCA Appropriateness . 6Monitoring . 9Adjuvant Therapies . 11Complementary Therapies . 12Guidelines for Implementing PCA Care . 12Mobilize Commitment. 12Define and Evaluate the Current State . 12Create a Shared Need . 12Standardize, Simplify, and Clarify . 13Appendices . 15Appendix A. Vendor Specific PCA Ordering/Programming Terms . 15Appendix B. Sample Standard IV PCA Order Set for Opioid Naïve ADULT Patients . 16Published December 2008; Revised December 2009. Disclaimer updated May 2014. This document is a collection of experience and learning from San Diego Patient Safety Council members incorporating referenced evidence-basedliterature, and is not intended to be a comprehensive source for all relevant information. The San Diego Patient Safety Council and its collaborating organizations are not responsible for any claims or losses arising from the use of, orfrom any errors or omissions in, this toolkit.A financial grant provided by Cardinal Health Foundation was administered by the Hospital Association of San Diego and Imperial Counties for facilitation and tool kit writing activities. No payment was made to any council member.Sharp HealthCare Foundation Patient Safety Fund received compensation for the facilitator’s time. CareFusion did not supervise, oversee, or influence any of the proceedings and does not accept any responsibility for the informationcontained in this document. SDPSC collaborating organizations are not responsible for any claims or losses arising from the use of, or from any errors or omissions in this tool kit.This document is in the public domain and may be used and reprinted without permission provided appropriate reference is made to the San Diego Patient Safety Council and the authors of the included tools and documents. Theinformation and tools in this document are also available in electronic format at www.hqinstitute.org. 2014 San Diego Patient Safety Council.San Diego Patient Safety CouncilPCA Guidelines of Care
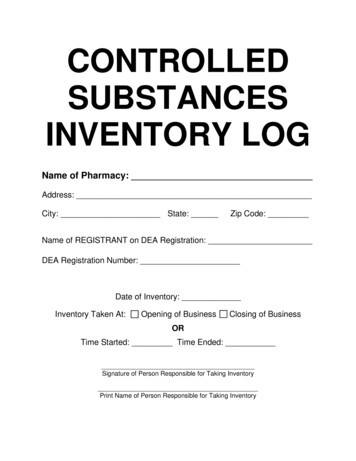
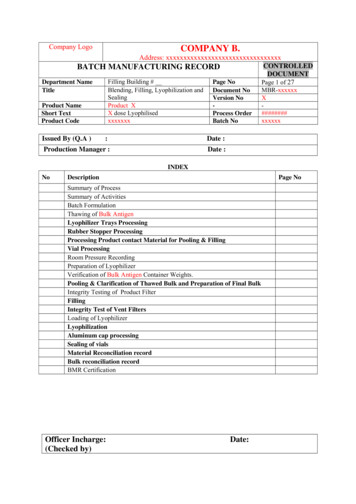
PCA Guidelines of Care Revised December 2009IntroductionPatient Controlled Analgesia (PCA) is aninteractive method of pain management that permitspatients to manage their pain by self-administeringdoses of analgesics, usually opioids.1 Current StatePatient Controlled Analgesia (PCA) can be an effectivetool in reducing pain. However, IV medications ingeneral are associated with the highest risk of harm topatients, and opioids are typically considered amongthe highest risk injectable medications.2PCA is a complicated, yet highly flexible means ofproviding opioids, consisting of several regimenelements addressed primarily in the Ordering andAdministration stages of the medication process.3For the purpose of this document, PCA prescriptionelements will respect the nomenclature outlined inVendor Specific PCA Ordering/Programming Terms (seeAppendix A). A cross-walk also is provided foravailable PCA devices.PCA errors involve many disciplines includingnurses, pharmacists, and physicians.PCA process is highly error prone and representsopportunities for improvement including the needto simplify, standardize, and clarify, as follows:Equipment-related issues present challengesincluding pump misprogramming, complexity,and confusion of PCA screens and drugselection options.Administration is especially vulnerable, with lessopportunity to intercept an error as there is noinherent redundancy in this stage. Landmarkmedication safety research has found only a 0-2percent medication error interception rate in theAdministration stage.6In 1999, the Joint Commission recommended thesepractice changes to improve opioid safety: Limit the opiates and narcotics available in floorstock.Educate staff about HYDROmorphone andmorphine mix-ups.Implement PCA protocols that include doublechecking of the drug, pump setting, and dosage.The use of PCA is a complex, high-risk treatment thatis associated with harmful events and death.4Extensive variability exists within and betweenhospital environments. Variability in patient response,clinical staffing, equipment, physician orders,medication dosages, and concentrations all contributeto risk for error.Other health care leaders also have strongly advocatedfor process simplification and standardization,including the Institute for Safe Medication Practice aspublished in their most recent safety improvementrecommendations (summarized here):7There is a shared need amongst hospitals to addressPCA Guidelines of Care for the Opioid Naïve Patient.Every clinician and hospital environment has a PCAstory5, such as is evident in the national MedMARXdatabase of voluntarily reported medication errors: PCA errors represent a four-fold higher risk thanother reported medication errors: PCA errors account for approximately onepercent of all medication errors, but 6.5 percentwere harmful.PCA errors occur in every phase of the medicationuse process. 1Pasero C, McCaffery M. (2004). Safe use of continuous infusion with IV PCA. JPeriAnesth Nurs. 19(1), 42-45.ISMP. List of high-alert medications. (2008). www.ismp.org/tools/highalertmedications.pdf.The Joint Commission. High-alert medications and patient safety. Sentinel Event Alert.Issue 11. Nov. 19, 1999.2 The Joint Commission. Standards Initiative Medication Management: MedicationManagement Practices B2-787C-4564-B408D3EB138EDB6D/0/HAP MM Outline.pdf.3Hicks RW, Sikirica V, Nelson W, Schein JR, Cousins, DD. (Mar 2008). Medicationerrors involving patient-controlled analgesia. Am. J. Health Syst. Pharm. 65, 429440.Assess vulnerability to serious errors. Medicationsafety teams should review current practices aroundthe use of custom concentrations.Limit concentrations. When possible, a single,standard concentration for each PCA drug shouldbe used. If more than one concentration is deemednecessary by the organization, the number ofstandard concentrations should be limited to twoat the most. Additionally, the use of customconcentrations should be minimized and, whenpossible, restricted to selected patient care areas.Distinguish custom concentrations. When acustom concentration is necessary, the containerlabel should be very distinctive and should not looklike the standard PCA syringe/bag label. Auxiliarylabels (e.g., “High-Potency”) and a different colorpharmacy label with specific instructions forprogramming the pump should be used for customconcentrations.Clarify the label. Institute for Safe MedicationPractices (ISMP) usually recommends presentingthe total drug concentration in the bag/syringefirst, followed by the amount of drug per mL belowthis within the same background or border on theproduct label.4Lotsch J, Dudziak R, Freynhagen R, Marschner J, Geisslinger, G. (2006). Fatalrespiratory depression after multiple intravenous morphine injections. ClinPharmacokinet. 45, 11. Adis Data Information BV.5San Diego Patient Safety Council6Leape L, Bates DW, Cullen DJ, et al. (1995) JAMA. 274(1), 35-43.Bates DW, Cullen DJ, Laird N, et al. (1995). JAMA. 274(1), 29-34.ISMP. Misprogramming PCA concentration leads to dosing errors. August 28, 2008issue. www.ismp.org/d/SpecialFollowUp.pdf.73
PCA Guidelines of Care Revised December 2009Depending on the PCA pump vendor, the user maybe prompted to enter the concentration in amg/mL strength. In these cases, it would be saferto indicate the concentration with the amount ofdrug per mL listed first, followed by the totalamount of drug/total volume in the syringe/bag. Match the MAR to the label. The concentrationon the Medication Administration Record (MAR)should be listed the same as the PCA label.Employ an independent double-check. Thenarcotics used for PCA are high-alert medications;thus, an independent double-check of the productand pump programming should be considered.When replacing an empty syringe/bag, the emptycontainer should be compared to the new containerto verify the concentration is the same.Use barcoding technology. Some infusion pumpsincorporate barcoding technology. Scanning thebarcode on the PCA bag would help ensure thecorrect concentration is entered during PCAprogramming.Use smart pumps. PCA pumps with Dose ErrorReduction System (DERS) should be usedwhenever possible. Because the significance of alow concentration alert during pump programmingis not fully appreciated, low concentration limitsshould always be set as hard limits. Additionally,clinical advisories should be in place to reinforcecaution when using custom concentrations.In 2000, the Institute of Medicine’s (IOM) originallandmark patient safety report, “To Err Is Human:Building a Safer Health System” concluded:wide patient safety improvements. San Diego Countyhospitals identified PCA as a significant opportunity toreduce morbidity and mortality.Goal CharterThe San Diego Patient Safety Council membersdesired to develop county-wide, evidenced-basedstandards of care for safe and effective painmanagement using PCA in opioid naïve patients.Performance ImprovementThe San Diego Patient Safety Council consists ofrepresentatives from county acute facilities anddisciplines. Council members reviewed literature,applied process improvement tools, and obtainedconsensus to build a comprehensive set ofrecommendations to prevent potential PCA errorsthroughout the county. The tool kit includes tools andinformation to assist acute care organizations inimplementing these recommendations.Success will be achieved when a safe, effectivestandard of care for PCA usage is implemented acrossSan Diego County, as evidenced by a reduction inpotential and actual harmful events.The Pain Management ProcessIn order to develop
PCA Guidelines of Care Revised December 2009 San Diego Patient Safety Council 3 Introduction Current State Patient Controlled Analgesia (PCA) can be an effective tool in reducing pain.