Transcription
Maghsoomi et al. BMC Cancer(2021) SEARCH ARTICLEOpen AccessEfficacy and safety of peptide receptorradionuclide therapy in advancedradioiodine-refractory differentiated thyroidcancer and metastatic medullary thyroidcancer: a systematic reviewZohreh Maghsoomi1 , Zahra Emami1 , Ramin Malboosbaf1 , Mojtaba Malek2 and Mohammad E. Khamseh1*AbstractBackground: It has been shown that a subgroup of patients with differentiated thyroid cancer (DTC) andmedullary thyroid carcinoma (MTC) would progress to advanced stages of thyroid cancer. Therefore, the presentstudy was done to systematically review available evidence in order to investigate efficacy and safety of peptidereceptor radionuclide therapy (PRRT) in the patients with advanced radioiodine refractory differentiated thyroidcancer (RR-DTC) and metastatic MTC.Methods: For this purpose, relevant studies investigated safety and efficacy of PRRT in the patients with advancedRR-DTC and metastatic MTC were identified by searching Medline (Pubmed, Ovid, and Ebsco), Scopus, Embase,Web of Science, and Cochrane Library databases (from database inception to March 24, 2021). The review wasperformed according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA)statement. Searching was done independently by two investigators. Two researchers independently extracted thedata and any disagreement was adjudicated by consensus. Quality of the studies was assessed using the tool ofcase reports/series in systematic reviews.Results: Among 2284 related papers, 41 papers met the inclusion criteria. A total of 157 patients with RR-DTC weretreated with PPRT. Biochemical and objective responses (partial and complete) were observed in 25.3 and 10.5% ofpatients, respectively. Among 220 patients with metastatic MTC, biochemical and objective responses wereobserved in 37.2 and 10.6% of the patients, respectively.Forty-six deaths were reported in 95 patients with advanced RR-DTC. In addition, 63 deaths were observed in 144patients with metastatic MTC. Major side effects were reported in 124 patients treated with 90Y -based agent. In thepatients treated with 177Lu-DOTA-TATE and 111In-Octreotide, mild and transient hematologic or renalcomplications were reported.(Continued on next page)* Correspondence: khamseh.m@iums.ac.ir1Endocrine Research Center, Institute of Endocrinology and Metabolism, IranUniversity of Medical Science (IUMS), No. 10, Firoozeh St, Vali-asr Ave, Vali-asrSq, Tehran 1593716615, IranFull list of author information is available at the end of the article The Author(s). 2021 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License,which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you giveappropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate ifchanges were made. The images or other third party material in this article are included in the article's Creative Commonslicence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commonslicence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtainpermission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.The Creative Commons Public Domain Dedication waiver ) applies to thedata made available in this article, unless otherwise stated in a credit line to the data.
Maghsoomi et al. BMC Cancer(2021) 21:579Page 2 of 14(Continued from previous page)Conclusion: Findings of the study revealed that in the absence of the established treatment for the patients withRR-DTC and metastatic MTC, PRRT could be effective with few adverse events.Trial registration: PROSPERO registration number: CRD42019125245.Keywords: Peptide receptor radionuclide therapy, Radioiodine refractory-differentiated thyroid Cancer, Medullarythyroid carcinoma, Papillary thyroid carcinoma, Yttrium-90, 177Lu-DOTATATE, Indium-111, Systematic reviewBackgroundThyroid cancer is the most common endocrine malignancy and its incidence has increased by 4.4% per yearduring 2007–2011 [1, 2]. Differentiated thyroid cancer(DTC), is the most frequent subtype of thyroid canceraccounting for 85–95% of the cases [3, 4]. Medullarythyroid cancer (MTC) originating from parafollicular orC cells of the thyroid gland accounts for approximately5% of all thyroid cancer cases [5].The standard of treatment for most patients with DTCincludes thyroidectomy followed by radioiodine treatment. A 10-year overall survival rate of 80–99% has beenreported among these patients [6]. However, in spite ofhighly effective treatment strategies, there is a chance ofrecurrence in 20% of the subjects. Radioactive iodineplays a major role in diagnosis and treatment of recurrent disease [7]. However, some thyroid cancers are resistant to radioiodine despite the elevated level ofthyroglobulin [8]. Radioiodine refractory-DTC (RRDTC) has shown aggressive clinical behavior and a 10year survival rate of 10% [9, 10]. Surgery and externalbeam radiation therapy can be used to manage local disease but not in case of widespread metastases. Moreover,chemotherapeutic agents have shown limited efficacywith considerable side effects [11, 12].MTC is inherently non-sensitive to radioactive iodine.Hence, its management is more difficult and its prognosis is worse than DTC [7]. The overall survival rate is between 75 and 85% during 10 years for individuals withMTC [13]. In spite of aggressive surgical treatment,there is almost a 50% of chance for persistent or recurrent disease, with deleterious effects on quality of lifeand the reduced 10-year survival rate by 40% [7, 13]. Reoperation, embolization, and perhaps radiotherapy couldimprove outcomes [14]. Meanwhile, response to conventional chemotherapy is limited with life-threatening toxicity [7]. Currently, other therapeutic options are scarceand not widely available.There are few alternative treatments in the patientswith advanced RR-DTC. Somatostatin receptor (SSTR)expression on cell surface of neuroendocrine and thyroidtumors regulates cell proliferation [15]. Targeting SSTRwith radiotracer in peptide receptor radionuclide therapy(PRRT) can induce tumor cell death. Overexpression ofsomatostatin receptor subtypes on surface of cells isrequired for PRRT and therefore, tumor remission canbe predicted based on the results of scintigraphy onsomatostatin receptor. Thus, PRRT could be a therapeutic option based on scintigraphy results of somatostatin receptor. It has been used previously for treatmentof metastatic neuroendocrine tumor and advanced pheochromocytomas and paragangliomas with high efficacy,tolerability, and low toxicity [16, 17].Accordingly, the present study was conducted to systematically review available evidence in order to investigate efficacy and safety of PRRT in the patients withadvanced RR-DTC and metastatic MTC.MethodsSearch strategy and selection criteriaA systematic review was performed on the publishedworks to investigate safety and efficacy of PRRT in thepatients with advanced RR-DTC and metastatic MTC,according to the preferred reporting items for systematicreviews and meta-analyses (PRISMA) statement [18].The study was registered before completing formalscreening of search results (PROSPERO registrationnumber: CRD42019125245).Eligibility criteriaAll the original studies containing data related to PRRTwere considered eligible to be included in the reviewstudy. Exclusion criteria were irrelevant papers (basedon screening of titles and abstracts), papers with insufficient data available, duplications, and review papers. Allthe eligible studies were included to assess efficacy, and/or safety of PRRT.Study identificationFor this systematic review, the Cochrane Central Register of Controlled Trials (Central), Medline (PubMed,Ovid, and Ebsco), Scopus, and Embase databases weresearched (from database inception to March 24, 2021).Search terms for English-language publications included:“peptide receptor radionuclide therapy”, “PRRT”, “radionuclide therapy”, “radiolabeled somatostatin analogues”,“thyroid cancer”, “thyroid carcinoma”, “thyroid neoplasm”, “differentiated thyroid cancer”, “differentiatedthyroid carcinoma”, “differentiated thyroid neoplasm”,“medullary thyroid cancer”, “medullary thyroid
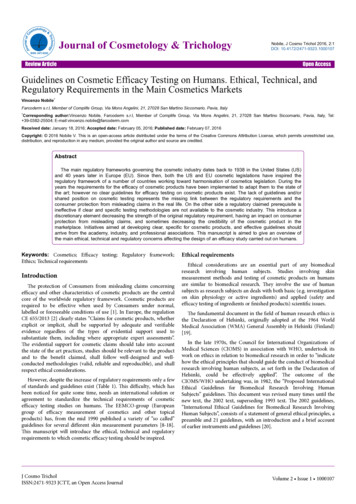
Maghsoomi et al. BMC Cancer(2021) 21:579carcinoma”, and “medullary thyroid neoplasm”. Detailsregarding the search strategy are provided in the Supplementary Table 1.The first search was done independently by two investigators (ZE and ZM). Also, a complete updatedsearch was performed on all databases available andnew studies (if any exist) were identified to assess thedetails and incorporate findings in this review. Thesnowballing techniques were used to complete thesearch by screening reference lists of the included papers for relevant studies. Also, registry of prospectivestudies with accessible results was searched. Two authors (RM, ZM) independently determined studiesthat should be evaluated further by scanning the title,abstract, or both based on the inclusion/exclusion criteria, the reviewers were blinded to names of thejournals and authors. All the potentially relevant papers as full texts were assessed and any disagreementswere resolved by consensus or by arbitration of twoexperts (MK and MM). In case of duplicates or multiple publications of a primary study, yield of information was enhanced by collating all available data andusing the most complete data set aggregated acrossall the known publications.Data collection and managementTwo reviewers (RM and ZM) independently extractedthe data from the included trials and any disagreement was adjudicated by consensus or by arbitrationof other reviewers (MK and MM). Published reportswere obtained for every study, and standard information was extracted in a spreadsheet. The followingdata were extracted: author’s name; year of publication; country where the study was performed; numberof participants, sex and age of the participants; tumorclassification, site of metastases; prior treatments (cumulative radioiodine in RR-DTC); cumulative activity(GBq) of PRRT; response to treatment criteria; timeto progression (TTP); follow-up duration; response totreatment; complications (major/minor); mortalityrate; and time to death.Biochemical response was defined in the patientswith DTC based on serum thyroglobulin (Tg) leveland in the patients with MTC, it was defined basedon serum calcitonin and carcino- embryonic antigen(CEA) levels. Different criteria were used to evaluateradiological responses to treatment, namely worldhealth organization (WHO) criteria, response evaluation criteria in solid tumors (RECIST) criteria, andsouthwest oncology group (SWOG) criteria [19].Moreover, the European organization for research andtreatment of cancer (EORTC) has classified metabolicresponse to treatment based on the maximum standardized uptake value (SUVmax) [20].Page 3 of 14For further analysis, proportions of complete and partial radiologic response were integrated as “objectiveresponse”.Occurrence of adverse events was evaluated usingcommon terminology criteria for adverse events (CTCAE) [21]. Two reviewers (RM and ZM) independentlyassessed methodological quality of the included studiesusing the tool of systematic reviews [22], and any disagreement was resolved by consensus.ResultsSearch on the literature led to identification of 2284publications, of which 98 papers were reviewed in fulltext (Fig. 1. shows flow chart of literature search andpaper selection). The risk of bias of the included studieswas low (Supplementary Table 2). Inter-reviewer’s agreement was “excellent” for the selected papers (Cohen’stest κ 0.96). Among 41 publications met the inclusioncriteria, 12 papers were retrospective in terms of design;19 papers were prospective studies and remaining 10 papers were case reports. Tables 1 and 2 summarize characteristics of the included studies assessing efficacy ofPRRT in the patients with advanced RR-DTC, and metastatic MTC, respectively. Data regarding safety of PRRTare presented in Table 3. Cumulative activity of PRRTranged between 0.925–83.2 GBq. For 90Y -based agent,most of the studies had used this agent with an administered activity ranging from 0.925 to 5.9 GBq per cycleusually up to 4 cycles. For 177Lu-DOTA-TATE, the administered activity rate was between 5.5–7.7 GBq percycle usually up to 4 cycles. In terms of follow-up duration, in the patients with advanced RR-DTC, it was between 1 and 99 months after commencement of PRRT(median: 12 months). It was between 1 and 144 months(median: 17 months) in the patients with metastaticMTC. Death was recorded in 109 patients. Time todeath varied from 1 to 63 months (median: 11 months).It should be noted that more than one criterion wasused to evaluate efficacy of PRRT, and some patients didnot complete their full course of treatment.Efficacy of PRRT in RR-DTCOverall, 157 patients with advanced RR-DTC weretreated with PRRT. Based on biochemical response criteria, from 79 treated patients, 20 cases of partial response (PR), 22 cases of stable disease (SD), and 37cases of persistent disease (PD) were determined. Out of91 patients whose radiological response was assessed, 9cases of PR, 39 cases of SD, and 43 cases of PD were recorded. Metabolic response was evaluated in 48 patients.Six cases of PR, 20 cases of SD, and 22 cases of PD wereidentified.In 85 patients treated with 90Y -based agent; 44 patients were assessed based on biochemical response
Maghsoomi et al. BMC Cancer(2021) 21:579Page 4 of 14Fig. 1 Flow chart of literature search and article selectionamong whom 8 cases of PR, 14 cases of SD, and 22 casesof PD were observed. Seven cases of PR, 23 cases of SD,and 25 cases of PD were identified in 55 patientsassessed based on radiological response. Moreover, 2cases of PR, 5 cases of SD, and 4 cases of PD were reported in 11 patients assessed based on metabolicresponse.In 26 patients treated with Lutetium-177 -based agent,10 cases of PR, and 11 cases of PD showed biochemicalresponse. Considering 20 patients assessed for radiological response, 2 cases of PR, 9 cases of SD, and 9cases of PD were reported. Out of 9 patients assessed formetabolic response, 1 case of PR, 4 cases of SD, and 4cases of PD were identified.Moreover, in 18 patients treated with Indium-111, biochemical response was assessed in 14 patients. Two patients with PR, 8 cases with SD, and 4 cases with PDwere reported. Seven SD cases and 9 PD cases were recorded based on radiological response in 16 patients.Among 157 patients with RR-DTC, biochemical andobjective responses (partial and complete) were observedin 25.3 and 10.5% of the patients, respectively.Efficacy of PRRT in metastatic MTCIn total, 220 patients with metastatic MTC were treatedwith PRRT. Based on biochemical response to the treatment in 145 patients, 7 cases of complete response (CR),47 cases of PR, 20 cases of SD, and 71 cases of PD wererecognized.Radiologic response was evaluated among 134 patients.Four cases of CR, 9 cases of PR, 75 cases of SD, and 46cases of PD were observed. Considering metabolic response among 46 patients, 7 cases of PR, 29 cases of SD,and 10 cases of PD were identified.Sixty-nine patients were treated by 90Y-DOTATOC,88 patients were treated with 177Lu-DOTA-TATE, and12 patients were treated with 111 Indium -based agent.Type of treatment was unknown in other patients.In 69 patients treated with 90Y-DOTATOC, 1 case ofCR, 15 cases of PR, 4 cases of SD, and 35 cases of PD(based on biochemical response criteria in 55 patients)as well as 2 cases of CR, 21 cases of SD and 15 cases ofPD (based on radiological response criteria in 38 patients) and 1 case of PR and 1 case of PD (based onmetabolic response criteria in 2 patients) were reported.Out of 74 patients treated with 177Lu-DOTA-TATE, 5cases of CR, 26 cases of PR, 14 cases of SD, and 29 casesof PD were observed based on biochemical response criteria. Moreover, 9 cases of PR, 50 cases of SD, and 26cases of PD were achieved in 85 patients based on radiological response criteria. Furthermore, SD was found in3 patients based on metabolic response criteria. In thepatients treated with 111 Indium -based agent; 1 case ofCR, 2 cases of SD, and 4 cases of PD (in 7 patients
PolandItalySwitzerlandAustriaGermanyCzepczynski Ret al. (2014) [15]Versari A et al.(2014) [23]Iten F et al.(2009) [24]Gabriel M et al.(2004) [25]Gorges R et al.(2001) urkeyCinkir, H. Y et al.(2020) [31]Roll. W et al.(2018) [32]Oliván-Sasot. Pet al. (2017) [33]Elboğa, U et al.(2016) [34]MFM/F:(4/1)M/F:(3/1)M/F:(5/3)B/Lu/M3FTC, 2PTC17FTC, 5PTC, 2No specifiedB/Lu/MNA6469PTC (tall cell variant)FTCMedian: 75 3FTC, 1PTC, 1HCTC(62 89)B/ Lu/MB/LiNALu/BB/Lu/MLu1FTC, 1PTC1FTCB/LuNANA1FTC, 1HCTCNA4PTC, 3FTCMedian: 64 1FTC, 3PTC(49,67)57 83Median:66NAMedian:60(44 74)Median: 68 1papillary-oxyphilic, 1follicular- Li/B/Lu/M(51 72)oxyphilic, 1Hürthle cellcarcinomaMedian:59(51 72)Median:58.8 DOTATOCTT/ND/RIT (27.75)TT/ND/C/RIT TOC90Y-DOTALanerotideTT/ND/EBR/RIT/C/EN 90Y-DOTATOCTT/ND/EBR/RITTT/ND/RIT (9.2529.91 (18.87))TT/ND/RITTT/ND/RIT (5.55–33.3 90Y-DOTATOC(12.95))TT/ND/EBR/RIT (3.1)Site ofPrior treatmentsLigandmetastasis (Iodine cumulative (Radionuclideactivity GBq (med)) ChelatorPeptide)Median: 59 5PTC, 1Oxiphilic, 3FTC, 2Insular Li/B/Lu(19–78)Median: 65 3FTC, 3HCTC(47–81)Age (year) Tumor Classification7.42.6Mean: 7.0 0.714.8 30.85.5 25.41.85 3.77.2 7.40 .925 7.061.7 14.81.7 9.625.55 7.45.6–30.34.329 17.953.7 14.85NANANA8NA5.5 (1.7 9.4)Biochemical NABiochemical NAAftersecondcycle6PRPR3PD, 2SDEORTC1FTC PR,4PD1PD, 2SD,1PR6PD, 2SD5PD, 3PRPD4PD3PR,11SD,11PD2SD, 5PD1SD, 2PD2SD,1PD5SD7PR, 17PD2PR, 5SD,4PD2PR, 4SD,4PD, 1NA11SD2PD, 2SD,1PR6 (3 9)13.8 (4.023.7)34(7 52)(4 12)(22 27)3615 (1 31)20 (16 31)NA16.8 (1.899.1)7.75 (3.511.5)2PD, 2SD.1PR4PD, 1PR,1SDRECISTBiochemical NAEORTCRECISTBiochemical NAImagingImagingWHOWHORECISTBiochemical NANABiochemical NAEORTCRECISTBiochemical NARECIST21 (2 68)TTP inFollow-Up ResponseSD (month) durationmedian:(months)Biochemical NACumulative Responseactivitycriteria(GBq)(2021) 21:57911548IndiaBasu. S et al.(2020) [30]NA25 NA73524 F/M:(12/12)4UKF/M:(9/2)Sex11 F/M6NTraub-Weidinger AustriaT et al. (2011)[29]Virgolini I et al.(2002) [28]Waldherr C et al. Switzerland(2001) [27]CountryReference(Publish Year)Table 1 Efficacy of peptide receptor radionuclide therapy (PRRT) in patients with advanced RR-DTCaMaghsoomi et al. BMC CancerPage 5 of 14
Netherlands 5IndiaItalyNetherlands 5Netherlands 1Netherlands 11 F/M:(7/4)GermanyItalyParihar AS et al.(2018) [37]Campenni Aet al. (2015) [38]Valkema R et al.(2002) [39]Krenning E et al.(1999) [40]Stokkel MP et al.(2004) [41]Budiawan Het al. (2013) [6]Scalorbi F et al.(2017) [42]F/M:(5/2)NANAMFPTCMedian:64.5 (2677)Median:67(44–69)NAMedian:70.8 b/RITNATT/ND/BT/RITTT/ND/RIT (3.7)TT/ND/RIT (18.5)TT/ND/EBR/C/RIT(1.9 16.7 (12.9))TT/ND/EBR/RIT (NA)NA90Y-DOTATATEand TATATE177Lu-DOTATATESite ofPrior treatmentsLigandmetastasis (Iodine cumulative (Radionuclideactivity GBq (med)) ChelatorPeptide)NANA14.3 33.120 7529.51 Biochemical NAimaging4SD, 5PD,2NA7SD, 3PD,1NA1SDNA2PR, 9PD,10SD50.4 (34.8– 1SD, 5PD,66)1PR12 (1 12)2415.8 (13.2 1SD, 4PD28.2)SWOG1SD, 1PD,1PR, 2NASDPRSD2SD, 1PD,1PR,1MRe2PD, 3PR15.8 (1516.6)54(4 48)SDPRBiochemical NARECISTBiochemical 5RECISTBiochemical Median:22(4 43)WHOImaging3TTP inFollow-Up ResponseSD (month) durationmedian:(months)Biochemical NACumulative Responseactivitycriteria(GBq)aAbbreviations: NA Not Available, FTC Follicular Thyroid Carcinoma, RR-DTC Radioiodine-Refractory Differentiated Thyroid Cancer, PTC Papillary Thyroid Carcinoma, HCTC Hurtle Cell Thyroid Carcinoma, TTPTime To ProgressionMetastatic Site: A Adrenal, Li Liver, Lu Lung, B Bone, M MediastinumPrior treatments: TT Total Thyroidectomy, ND Node Dissection, EBR External Beam Radiation, C Chemotherapy, I Radioactive Iodine therapy, BT Biotherapy with octreotide, LITT Laser- inducedthermotherapy, REDIFF Redifferentiation Using RoaccutaneResponse: CR Complete Response, PR Partial Remission, SD Stable Disease, PD Progressive Disease, MR Minor RemissionNA4FTC,3HCTC6PTC, 5FTCPTC4PTC, 1FTCPTCPTCMedian: 52 3HCTC, 1FTC, 1PTC(52 74)NAAge (year) Tumor Classification21 F/M: NA(13/8)711F/MNATeunissen JJet al. (2005) [36]1IndiaSexJois B et al.(2014) [35]NCountryReference(Publish Year)Table 1 Efficacy of peptide receptor radionuclide therapy (PRRT) in patients with advanced RR-DTCa (Continued)Maghsoomi et al. BMC Cancer(2021) 21:579Page 6 of 14
Switzerland 31 F/M:10/21ItalyChinaSwitzerland 12 F/M:5/7Iten F et al. (2007)[45]Bodei L et al.(2004) [46]Gao ZR et al.(2004) [47]Waldherr C et al.(2001) [27]MIndiaCanadaBrazilTurkeyNetherlands 10 F/M:Makis W et al.(2015) [51]Vaisman F et al.(2015) [52]Soydal Ç et al.(2014) [53]Beukhof, C et al.F/MNANAMedian: 62Median: 41Median: 35.8(20 54)Median: 56.5(38,75)Median: 48(25,80)Median: 53(38,59)32 8765Median: 60(24 72)58Median: 53(31–78)Mean: MLu/Li/B/MNANALu/ MLu/Li/B/MNAB/M/ D/RFTT/ND/CSite ofPriormetastasis OTA-TOC90Y-DOTA-TOC90Y-DOTA-TOC90Y-DOTA-TOCLigand (RadionuclideChelator Peptide)27.8 29.629.629.622.25.55 33.314.8 44.46.5 52.39.25 9.621.7 vity (GBq)TTP in SD(month)NANAWHOEORTCNANA10 (3 14)37.3 (17.656.9)NANABiochemical 8.4 (3.6RECISTRECISTWHOBiochemical NARECISTBiochemical 24 (15.132.9)EORTCImagingBiochemical NAWHOWHOWHOBiochemical 6SWOGBiochemical NABiochemical NANARECISTBiochemical NA16.88 (4.8 144)6 weeks Afterfourth cycle129.5 (9,10)26 (16.6 35.3)24.2 (0 48.8)NA2415 (1 31)10.54015.7 (1.4 107)73SD, 4PR,2SD3PR, 3SD,1PD2SD1PR, 1PD22SD, 4PR,17PD5CR, 4SD,13PR, 21PD3SD15SD, 2PR,2PD7SD, 8PR,4PD2SD5SD, 7PDSDPR12SD, 7PD,2CR3SD, 12PD,5PR, 1CR9R, months)RECISTBiochemical NAResponsecriteria(2021) 21:57927243 F/M:8/35MParghane, R. Vet al. (2020) [50]3TurkeyCinkir, H. Y et al.(2020) [31]19 F/M:6/13TurkeyFMBilgic, S et al.(2020) [49]Otte A et al. (1999) Switzerland 2[48]121 F/M:8/131USABertagna F et al.(2009) [44]NASwitzerland 1SexÖksüz M et al.(2014) [43]NCountryReference(Publish Year)Table 2 Efficacy of peptide receptor radionuclide therapy in patients with metastatic MTCaMaghsoomi et al. BMC CancerPage 7 of 14
Netherlands 5PolandNetherlands 3Valkema R et al.(2002) [39]Caplin M et al.(2000) [57]Krenning E et al.(1999) [40]9UKIndiaGermanyItalyHayes AR et al.(2019) [59]Puranik A et al.(2019) [60]Budiawan H et al.(2013) [6]Scalorbi F et al.(2017) [42]NANANAFF/M:(4/3)F/M:3/4NAMedian: 66.5(21 68)Mean: 47.9(26 72)NAMedian: 52(46–58)NA46Median: 57.4(27.7 -DOTATATE and177Lu-DOTATATE90Y-DOTATATE ide177Lu-octreotideLigand (RadionuclideChelator Peptide)NANATT/ND/EBR/ 90Y-DOTATATE TTT/ND/CNASite ofPriormetastasis treatmentNANANANA25 75NA11.425.14 87.2811.954NACumulativeactivity (GBq)NA144)TTP in SD(month)NANANAEORTCEORTCNANANABiochemical 14 (8–20)RECISTImaging6PD24NA5SD, 2PD4SD, 1PD,1PR5PR7250.4 (34.8–66)17SD6PR, 3PD2CR1SD, 2PDCR3SD, 2PD2SD, 3PDPD2SD4SD, 6PD3PDResponse36NA27.5 (22,33)24NA7.8 (2.76 26.8)SWOGBiochemical NA7.8 (2.76 26.8)97 weeks After lastcycleFollow-Upduration(months)Biochemical NASWOGBiochemical NAImagingRECISTResponsecriteriaaAbbreviations: NA Not Available, MTC Medullary Thyroid Carcinoma, TTP Time To ProgressionMetastatic Site: A Adrenal, Li Liver, Lu Lung, B Bone, M MediastinumPrior treatments: TT Total Thyroidectomy, ND Node Dissection, EBR External Beam Radiation, C Chemotherapy, BT Biotherapy with Octreotide, LITT Laser Induced Thermotherapy, REDIFF RedifferentiationUsing RoaccutaneResponse: CR Complete Response, PR Partial Remission, SD Stable Disease, PD Progressive Disease, MR Minor Remission7728 F/M:14/142Buscombe JR et al. UK(2003) [58]1NAMCanadaPasieka JL et al.(2004) [56]1NA2IndiaSexMathew, D et al.(2018) [55]N6/4Country(2019) [54]Reference(Publish Year)Table 2 Efficacy of peptide receptor radionuclide therapy in patients with metastatic MTCa (Continued)Maghsoomi et al. BMC Cancer(2021) 21:579Page 8 of 14
Maghsoomi et al. BMC Cancer(2021) 21:579Page 9 of 14Table 3 Safety of Peptide Receptor Radionuclide Therapy in patients with Advanced RR-DTC & Metastatic MTCaReferenceKind ofPRRTNumber &Kind ofTumorCumulative HematologicactivityToxicity(GBq)Gastrointestinal& Genitourinary n timeto deathsince thefirst courseof PRRT(months))Bertagna Fet al. [44]90YDOTATOC1MTC9.01NoneNoneNoneNone1 (NA)Bodei Let al. [46]90YDOTATOC21MTC7.5–19.215NANoneNA4 (NA)Bodei Let al. [61]90YDOTATOC4MTC3.8 19.2NoneNoneNoneNoneNoneCzepczynskiR et al. [15]90YDOTATOC3FTC, 3HCTC3.7 14.86None2None1 (63)Gorges Ret al. ilic,1Hürthle cellcarcinoma1.7 9.623mildLymphocytopeniaNoneNoneNone1 (16)Iten F et penia4nausea4permanentrenal toxicityNone11FTC, 4PTC,2No (13.7)Iten F et ansientThrombocytopenia5Nausea6NA22 (25.8)Versari Aet al. [23]90YDOTATOC5PTC,1Oxiphilic,3FTC,2Insular4.329 17.95 2Transient ase oftransaminase1permanentrenal toxicity2AstheniaNoneWaldherr Cet al. [27]90YDOTATOC12MTC, 4PTC, 1.7 143FTC6Anemia,10TransientLymphocytopeniaNANANA1 (1)7.2 7.4NoneNone1renal toxicityNone1 (22)1.85 3.72TransientThrombocytopenia5.5 25.4NoneNone1 transientNone2 (7 raub90Y1FTC, 1PTCWeidinger T DOTATOCet al. [29]90Y-DOTA- 1FTC, 1HCTCLanerotideNone2 (4 12)Basu. S et al. 177Lu[30]DOTATATE8 DTCBeukhof, Cet al. [54]177LuOctreotate10MTCCinkir, H. Yet al. [31]177LuDOTATATE3MTC, 3PTC,1FTC14.8 44.42Transient rghane, R. 177LuV et al. [50] DOTATATE43MTC5.55 33.31Transient1NauseaNoneNone20Teunissen Jjet al. [12]177LuDOTATATE3HCTC, 1FTC, 22.4–30.11PTCNANANANA1 (48), 1 (4)Vaisman Fet al. [52]177LuDOTATATE7MTCNANANANA1transient sexualdysfunction,2mild hair Loss,1hypersensitivitydermatologiclesions2 (1/7 beforethe end ofthe protocol)Valkema R1111n-5MTC, 5DTCNANoneNoneNoneNone4MTC (11.22
Maghsoomi et al. BMC Cancer(2021) 21:579Page 10 of 14Table 3 Safety of Peptide Receptor Radionuclide Therapy in patients with Advanced RR-DTC & Metastatic MTCa (Continued)ReferenceKind ofPRRTet al. [39]OcterotideStokkel Mpet al. [41]111InDTPAOctreotideNumber &Kind ofTumorCumulative HematologicactivityToxicity(GBq)Gastrointestinal& Genitourinary n timeto deathsince thefirst courseof PRRT(months))(2.76 26.8)),5DTC (15.8(13.2 28.2))6PTC, 5FTCBudiawan H 90Y7MTC, 4FTC,et al. [6]DOTATATE 3HCTCand 177LuDOTATATE14.3 33.11thrombocytopenia NoneNoneNone1 (5), 2nonrelated (1, 3)NA8minorhematology,5Anemia,1Leukopenia5mild renaltoxicityNone1MTC (12),2FTC (12),1HCTC (24)6transientincrease oftransaminaseAbbreviations: Na Not Available, RR-DTC Radioiodine-Refractory Differentiated Thyroid Cancer, FTC Follicular Thyroid Carcinoma, PTC Papillary Thyroid Carcinoma,HCTC Hurtle Cell Thyroid Carcinoma, MTC Medullary Thyroid Carcinomaassessed based on biochemical response) and also, 2cases of CR, 4 cases of SD, and 5 cases of PD (in 11 patients assessed based on radiological criteria) werereported.Overall, in the patients with metastatic MTC, biochemical and objective responses were observed in 37.2and 10.6% of the patients, respectively.Safety of PRRTSafety of PRRT was assessed in 19 studies (totally, 239patients). Death was observed in 109 patients. Inaddition, time to death varied from 1 to 63 months.In 95 patients with advanced RR-DTC, 46 patientsdied. Time to death ranged from 1 to 63 months fromcommencement of PRRT. Based on type of PRRT, deathoccurred in 29/55 patients treated with 90Y -based agent,6/17 patients treated with 177Lu-DOTA-TATE, and 8/16 patients treated with 111In-Octreotide. Among 44patients with metastatic MTC, 63 patients died. Time todeath ranged from 1 to 26.8 months since initiating thefirst course of PRRT. Based on the type of PRRT, deathoccurred in 27/69 patients treated with 90Y-DOTATOC,31/63 patients treated with 177Lu-DOTA-TATE, and 4/5 patients treated with 111In- Octreotide. Major side effects were reported in 124 patients treated with 90Y-based agent. Fourteen patients developed renal toxicity(2 cases of grade 4, 2 cases of grade 3, 2 cases of grade 2,and 8 cases of grade 1). Furthermore, hematologic toxicity was observed in 64 patients (3 cases developedgrade 4 of thrombocytopenia, and 1 patient reported tosuffer from grade 4 of anemia). Moreover, in 80 patientstreated with 177Lu-DOTA-TATE, mild and transienthematologic and ren
cases of CR, 26 cases of PR, 14 cases of SD, and 29 cases of PD were observed based on biochemical response cri-teria. Moreover, 9 cases of PR, 50 cases of SD, and 26 cases of PD were achieved in 85 patients based on radio-logical response criteria. Furthermore, SD was found in 3 patients based on metabolic response criteria. In the