Transcription
MEDICAID SERVICES MANUALTRANSMITTAL LETTERJuly 28, 2020TO:CUSTODIANS OF MEDICAID SERVICES MANUALFROM:CODY L. PHINNEY, DEPUTY ADMINISTRATORSUBJECT:MEDICAID SERVICES MANUAL CHANGESCHAPTER 1200 – PRESCRIBED DRUGSBACKGROUND AND EXPLANATIONRevisions to Medicaid Services Manual (MSM), Chapter 1200 – Prescribed Drugs, Appendix A,are being proposed to reflect recommendations approved on January 23, 2020 by the Drug UseReview (DUR) Board. The proposed changes include addition of new prior authorization criteriafor Nucala (mepolizuman) and Dupixent (dupilumab) to the Monoclonal Antibody Agentssection, addition of new prior authorization criteria for Lemtrada (alemtuzumab), Mavenclad (cladribine), Ocrevus (ocrelizumab) agents for Multiple Sclerosis (MS) section, addition of newprior authorization criteria for Zelnorm (tegaserod) to the existing Functional GastrointestinalAgents section, addition of new prior authorization criteria for Sunosi (solriamfetol) to theNarcolepsy Agents section and addition of new prior authorization criteria for Nayzilam (midazolam) to the existing Anticonvulsants policy section.Revisions to MSM Chapter 1200 – Appendix A are also being proposed to the Diabetic SupplyProgram policy by adding language specific to preferred and non-preferred diabetic products andsupplies, adding clarification language for when a prior authorization is required/not required andproviding language specific to Continuous Glucose Monitors with special features for recipientswith an impairment. Lastly, it is proposing revisions to Antihepatitis Agents policy by updatingthe age indication for Epclusa based on updated FDA indications.Throughout the chapter, grammar, punctuation and capitalization changes were made, duplicationsremoved, acronyms used and standardized and language reworded for clarity. Renumbering andre-arranging of sections was necessary.Entities Financially Affected: No Entities are anticipated to be financially affected.Financial Impact on Local Government: No Impact of Local Government known.These changes are effective August 3, 2020.MATERIAL TRANSMITTEDOL 05/20/2020MSM Ch 1200 – Prescribed DrugsMATERIAL SUPERSEDEDMTL N/AMSM Ch 1200 – Prescribed DrugsPage 1 of 2
Background and Explanation of PolicyChanges, Clarifications and UpdatesManual SectionSection TitleAppendix ASection PMonoclonalAntibody AgentsUpdated Food and Drug Administration (FDA) ageindication for Nucala . Added new priorauthorization criteria for Nucala for the treatment ofsevere asthma and Eosinophilic Granulomatosis withPolyangiitis (EGPA). Added new prior authorizationcriteria for Dupixent .Appendix ASection CCAmpyra Updated section title to “Multiple Sclerosis (MS)Agents.” Added new prior authorization criteria forLemtrada , Mavenclad and Ocrevus .Appendix ASection HHAnti-HepatitisAgentsRevisions to existing criteria for Epclusa were madebased on updated FDA age indications.Appendix ASection WWFunctionalGastrointestinalDisorder AgentsAdded new prior authorization criteria for Zelnorm .Appendix ASection AAAXyrem (sodiumoxybate), Provigil (modafinil),Nuvigil (armodafinil)Updated section title to “Narcolepsy Agents,” addednew prior authorization criteria for Sunosi .Appendix ASection BBBBAnticonvulsantsAdded newNayzilam .Appendix BSection 4Diabetic SupplyProgramRevisions to existing prior authorization criteria forDiabetic Supply Program. These revisions includeadding clarifying language regarding preferred andnon-preferred diabetic products and supplies andlanguage specific to Continuous Glucose Monitors(CGMs) with special features for recipients with animpairment.Page 2 of 2priorauthorizationcriteriafor
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUALP.Monoclonal Antibody AgentsTherapeutic Class: Respiratory Monoclonal Antibody AgentsFasenra reviewed by DUR Board: April 26, 2018Xolair previously reviewed: October 19, 2017Last Reviewed by the DUR Board: January 23, 2020July 28, 2016Monoclonal Antibody AgentsXolair (Omalizumab) is are subject to prior authorization andquantity limitations based on the Application of Standards in Section 1927 of the SSA and/orapproved by the DUR Board. Refer to the Nevada Medicaid and Check Up Pharmacy Manual forspecific quantity limits.1.Coverage and Limitationsa.Xolair (Omalizumab)1.November 5, 2018Approval will be given if all the following criteria are met and documented:a.1.The recipient will not use the requested antiasthmaticmonoclonal antibody in combination with other antiasthmaticmonoclonal antibodies.b.All of the following criteria must be met and documented for adiagnosis of moderate to severe persistent asthma:1.The recipient must be six years of age or older; and2.The recipient must have a history of a positive skin test orRadioallergosorbent (RAST) test to a perennialaeroallergen; and3.The prescriber must be either a pulmonologist or allergist/immunologist; and4.The recipient must have had an inadequate response, adversereaction or contraindication to inhaled, oral corticosteroids;and5.The recipient must have had an inadequate response, adversereaction or contraindication to a leukotriene receptorantagonist; and6.The recipient must have had a pretreatment serum totalImmunoglobulin E (IgE) level between 30 IU/mL and 700IU/mL; and7.The recipient's current weight must be recorded; andPRESCRIBED DRUGSAppendix A Page 35
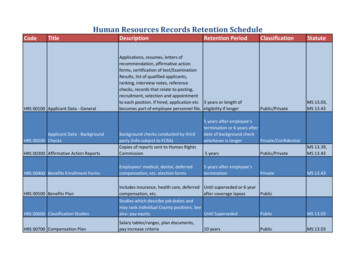
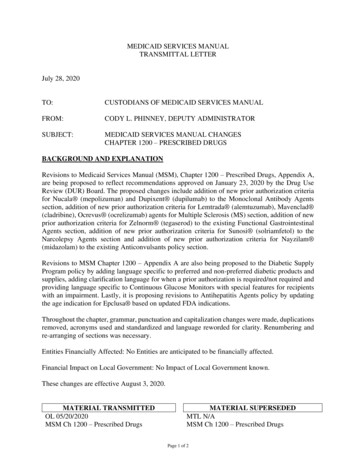
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUAL8.2.The requested dose is appropriate for the recipient’s pretreatment serum IgE and body weight (see Table 1).All the following criteria must be met and documented for diagnosis ofchronic idiopathic urticaria (CIU):a.The recipient is 12 years of age or older; andb.The recipient must have had an inadequate response, adversereaction or contraindication to two different oral second-generationantihistamines; andc.The recipient must have had an inadequate response, adversereaction or contraindication to an oral second-generationantihistamine in combination with a leukotriene receptor antagonist;andd.The prescriber must be either an allergist/immunologist,dermatologist or a rheumatologist or there is documentation in therecipient’s medical record that a consultation was done by anallergist/immunologist, dermatologist or a rheumatologist regardingthe diagnosis and treatment recommendations; ande.The requested dose is:1.Initial therapy: 150 mg every four weeks or 300 mg everyfour weeks and clinical rationale for starting therapy at 300mg every four weeks has been provided.2.3.2.Continuation of therapy: 150 mg or 300 mg every fourweeks.Prior Authorization Guidelinesa.Prior authorization approval will be for 12 months.b.Prior Authorization forms are available .aspxTable 1: Dosing for Xolair (omalizumab)*Pre-treatmentSerum IgE30-60(IU/mL) 30-100150 mg 100-200300 mg 200-300300 mg 300-400225 mg 400-500300 mg 500-600300 mg 600-700375 mgEvery 2 Weeks DosingApril 27, 2017Body Weight (kg) 60-70 70-90150 mg300 mg225 mg225 mg300 mg375 mgPRESCRIBED DRUGS 90-150150 mg300 mg225 mg300 mg375 mg300 mg225 mg300 mgDO NOT DOSEAppendix A Page 36
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUALEvery 4 Weeks Dosingb.Nucala (mepolizumab), Cinqair (reslizumab)1.2.c.a.The recipient will not use the requested antiasthmatic monoclonalantibody in combination with other antiasthmatic monoclonalantibodies; andb.The recipient must have a diagnosis of severe eosinophilicphenotype asthma; andc.The recipient must be of FDA indicated an appropriate age:1.Mepolizumab: 12 six years of age or older2.Reslizumab: 18 years of age or olderd.And, the prescriber must be either a pulmonologist or allergist/immunologist; ande.The recipient must be uncontrolled on current therapy includinghigh dose corticosteroid and/or on a secondary asthma inhaler; andf.There is documentation of the recipient’s vaccination status; andg.The requested dose is appropriate:1.Mepolizumab: 100 mg subcutaneously every four weeks.2.Reslizumab: 3 mg/kg via intravenous infusion of 20 to 50minutes every four weeks.Prior Authorization Guidelinesa.Prior authorization approval will be for 12 months.b.Prior Authorization forms are available .aspx.Nucala (mepolizumab) for the treatment of severe asthma1.May 6, 2019All the following criteria must be met and documented:Approval will be given if all the following criteria are met and documented:a.The recipient must have a diagnosis of severe asthma; andb.The asthma is an eosinophilic phenotype as defined by one of thefollowing:PRESCRIBED DRUGSAppendix A Page 37
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUALc.d.1.Baseline (pre-treatment) peripheral blood eosinophil levelgreater than or equal to 150 cells/microliter; or2.Peripheral blood eosinophil levels were greater than or equalto 300 cells/microliter within the past 12 months; andOne of the following:1.The recipient has had at least one or more asthmaexacerbations requiring systemic corticosteroid within thepast 12 months; or2.The recipient has had prior intubation for an asthmaexacerbation; or3.The recipient has had prior asthma-related hospitalizationwithin the past 12 months; andThe recipient is currently being treated with one of the following(unless there is a contraindication or intolerance to thesemedications)1.2.2.a.High-dose inhaled corticosteroid (ICS) (e.g., ay); andb.Additional asthma controller medication (e.g.,leukotriene receptor antagonist, long acting beta-2agonist [LABA], theophylline); orOne maximally dosed combination ICS/LABA product(e.g., Advair [fluticasone propionate/salmeterol], /formoterol]); ande.The recipient age is greater than or equal to six years; andf.The medication must be prescribed by or in consultation with one ofthe following:1.Pulmonologist; or2.Allergist/Immunologist.Recertification request (the recipient must meet all the criteria):a.May 6, 2019Both the following:Documentation of positive clinical response to therapy (e.g.reduction in exacerbations, improvement in forced expiratoryPRESCRIBED DRUGSAppendix A Page 38
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUALvolume in one second [FEV1], decreased use of rescuemedications); andb.The recipient is currently being treated with one of the followingunless there is a contraindication or intolerance to thesemedications:1.2.c.3.d.a.ICS; andb.Additional asthma controller medication (e.g.,leukotriene receptor antagonist, long acting beta-2agonist [LABA], theophylline); orA combination ICS/LABA product (e.g., Advair [fluticasonepropionate/salmeterol], Dulera [mometasone/formoterol],Symbicort [budesonide/formoterol]); andThe medication must be prescribed by or in consultation with one ofthe following:1.Pulmonologist; or2.Allergist/Immunologist.Prior Authorization Guidelinesa.Initial authorization will be approved for six months.b.Recertification will be approved for 12 months.c.Prior Authorization forms are available .aspx.Nucala (mepolizumab) for the treatment of Eosinophilic Granulomatosis withPolyangiitis (EGPA)1.May 6, 2019Both the following:Approval will be given if all the following criteria are met and documented:a.The recipient must have a diagnosis of EGPA; andb.The recipient’s disease has relapsed or is refractory to standard ofcare therapy (i.e. corticosteroid treatment with or withoutimmunosuppressive therapy); andc.The recipient is currently receiving corticosteroid therapy; andd.The medication must be prescribed or in consultation with one ofthe following:PRESCRIBED DRUGSAppendix A Page 39
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUAL2.c.Pulmonologist; or2.Rheumatologist; or3.Allergist/Immunologist.Recertification Requests (the recipient must meet the following criteria)a.3.1.Documentation of positive clinical response to therapy (e.g. increasein remission time).Prior Authorization Guidelinesa.Initial authorization will be approved for 12 months.b.Recertification request will be approved 12 months.c.Prior Authorization forms are available .aspx.Fasenra (benralizumab)1.All the following criteria must be met and documented:a.The recipient must be 12 years of age or older; andb.The recipient will not use the requested antiasthmatic monoclonalantibody in combination with other antiasthamtic monoclonalantibodies; andc.The recipient must have a diagnosis of severe eosinophilicphenotype asthma; andd.One of the following:e.1.Patient has had at least two or more asthma exacerbationsrequiring systemic corticosteroids within the past 12 months;or2.Any prior intubation for an asthma exacerbation; or3.Prior asthma-related hospitalization within the past 12months.Patient is currently being treated with one of the following unlessthere is a contraindication or intolerance to these medications:1.May 6, 2019Both a high-dose inhaled corticosteroid (ICS) (e.g., greaterthan 500 mcg fluticasone propionate equivalent/day) and anadditional asthma controller medication (e.g., leukotrienePRESCRIBED DRUGSAppendix A Page 40
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUALreceptor antagonist, long-acting beta-2 agonist (LABA),theophylline); or2.f.2.d.1.Pulmonologist; or2.Allergy/Immunology specialist.a.There is documentation of a positive clinical response (e.g.,reduction in exacerbation).b.Patient is currently being treated with one of the following unlessthere is a contraindication or intolerance to these medications:1.Both an inhaled corticosteroid (ICS) (5,E) and an additionalasthma controller medication (e.g., leukotriene theophylline); or2.A combination ICS/LABA product (e.g., Advair (fluticasonepropionate/salmeterol), Dulera (mometasone/formoterol),Symbicort (budesonide/formoterol)).Prescribed by or in consultation with one of the following:1.Pulmonologist; or2.Allergy/Immunology specialist.Prior Authorization Guidelinesa.Initial prior authorization will be for 12 months.b.Recertification request will be for 12 months.c.Prior Authorization forms are available .aspx.Dupixent (dupilumab)1.August 6, 2018Prescribed by or in consultation with one of the following:Recertification Request: Authorization for continued use shall be reviewedat least every 12 months when the following criteria are met:c.3.One maximally dosed maximally-dosed propionate/salmeterol), Dulera (mometasone/formoterol),Symbicort (budesonide/ formoterol)).Atopic DermatitisPRESCRIBED DRUGSAppendix A Page 41
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUALa.Approval will be given if all the following criteria are met anddocumented:1.The recipient must have a diagnosis of moderate to severeatopic dermatitis; and2.One of the following:3.b.2.b.Trial and failure or intolerance to one of thefollowing, unless the recipient is not a candidate fortherapy (e.g. immunocompromised)1.Elidel (pimecrolumus) topical cream; or2.Tacrolimus topical ointment; andThe medication must be prescribed by or in consultationwith one of the following:a.Dermatologist; orb.Allergist/Immunologist.Documentation of positive clinical response to Dupixent therapy.Prior Authorization Guidelines1.Initial authorization approval will be for 12 months.2.Recertification approval will be for 12 months.3.Prior Authorization forms are available .aspx.Eosinophilic Asthmaa.April 27, 2017Trial and failure, contraindication, or intolerance toone medium to high potency topical corticosteroid(e.g. betamethasone, tramcinolone); orRecertification request (the recipient must meet all criteria):1.c.a.Approval will be given if all the following criteria are met anddocumented:PRESCRIBED DRUGSAppendix A Page 42
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUAL1.The recipient has a diagnosis of moderate to severe asthma;and2.Asthma is an eosinophilic phenotype as defined by abaseline (pre-treatment) peripheral blood eosinophil levelgreater than or equal to 150 cells per microliter; and3.Age is greater or equal to 12 years; and4.One of the following:5.a.The recipient has had at least one or more asthmaexacerbations requiring systematic corticosteroidwithin the past 12 months; orb.The recipient has had prior intubation for an asthmaexacerbation; orc.The recipient has had prior asthma-relatedhospitalization within the past 12 months; andThe recipient is currently being treated with one of thefollowing unless there is a contraindication or intolerance tothese medications:a.b.6.April 27, 2017Both the following:1.High-dose ICS [e.g., greater than 500 mcgfluticasone propionate equivalent/day]; and2.Additional asthma controller medication[e.g., leukotriene receptor antagonist, longacting beta-2 agonist (LABA), theophylline];orOne maximally dosed combination t[budesonide/formoterol]); andThe medication must be prescribed by or in consultationwith one of the following:1.Pulmonologist; or2.Allergist/Immunologist.PRESCRIBED DRUGSAppendix A Page 43
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUALb.Recertification request (recipient must meet all the criteria):1.Documentation of a positive clinical response to CRSwNPtherapy (e.g., reduction in exacerbations, improvement inFEV1, decreased use of rescue medications); and2.The recipient is currently being treated with one of thefollowing unless there is a contraindication or intolerance tothese medications:a.b.3.c.3.1.Inhaled corticosteroid (ICS); and2.Additional asthma controller medication[e.g., leukotriene receptor antagonist, longacting beta-2 agonist (LABA), theophylline];orA combination ICS/LABA product (e.g., ol]); andThe medication is prescribed by or in consultation with oneof the following:a.Pulmonologist; orb.Allergist/Immunologist.Prior Authorization Guidelines1.Initial prior authorization will be for six months.2.Recertification approval will be for 12 months.3.Prior Authorization forms are available .aspx.Oral Corticosteroid Dependent Asthmaa.Approval will be given if all the following criteria are met anddocumented:1.April 27, 2017Both the following:The recipient must have a diagnosis of moderate to severeasthma; andPRESCRIBED DRUGSAppendix A Page 44
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUAL2.The recipient is greater or equal to 12 years of age; and3.The recipient is currently dependent on oral corticosteroidsfor the treatment of asthma; and4.The recipient is currently being treated with one of thefollowing unless there is a contraindication or intolerance tothese medications:a.b.5.b.Both the following:1.High-dose ICS [e.g., greater than 500 mcgfluticasone propionate equivalent/day]; and2.Additional asthma controller medication[e.g., leukotriene receptor antagonist, longacting beta-2 agonist (LABA), theophylline];orOne maximally dosed combination t[budesonide/formoterol]); andThe medication must be prescribed by or in consultationwith one of the following:a.Pulmonologist; orb.Allergist/Immunologist.Recertification Request (the recipient must meet all criteria):1.Documentation of a positive clinical response to Dupixent therapy (e.g., reduction in exacerbations, improvement inFEV1, reduction in oral corticosteroid dose); and2.The recipient is currently being treated with one of thefollowing unless there is a contraindication or intolerance tothese medications:a.Both the following:1.April 27, 2017PRESCRIBED DRUGSICS; andAppendix A Page 45
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUAL2.b.3.c.4.A combination ICS/LABA product (e.g., ol]); andThe medication must be prescribed by or in consultationwith one of the following:a.Pulmonologist; orb.Allergist/Immunologist.Prior Authorization Guidelines1.Initial prior authorization approval will be for six months.2.Recertification approval will be 12 months.3.Prior Authorization forms are available .aspx.Chronic Rhinosinusitis with Nasal Polyposis (CRSwNP)a.Approval will be given if all the following criteria are met anddocumented:1.2.April 27, 2017Additional asthma controller medication[e.g., leukotriene receptor antagonist, longacting beta-2 agonist (LABA), theophylline];orThe recipient must have a diagnosis of CRSwNP; andUnless contraindicated, the recipient has had an inadequateresponse to two months of treatment with an intranasalcorticosteroid (e.g., fluticasone, mometasone) [Documentdrug(s), dose, duration and date of trial]; and3.The medication will not be used in combination with anotheragent for CRSwNP; and4.The medication must be prescribed by or in consultationwith an Allergist/Immunologist.PRESCRIBED DRUGSAppendix A Page 46
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUALb.c.2.Recertification request (the recipient must meet all criteria):1.Documentation of a positive clinical response to therapy;and2.The medication will not be used in combination with anotheragent for CRSwNP; and3.The medication is prescribed by or in consultation with anallergist/Immunologist.Prior Authorization Guidelines1.Initial prior authorization approval will be for 12 months.2.Recertification approval will be for 12 months.3.Prior Authorization forms are available .aspx.Prior Authorization Guidelinesa.Prior authorization approval will be for 12 months.b.a.Prior Authorization forms are available .aspxTable 1: Dosing for Xolair (omalizumab)*Pre-treatmentSerum IgE30-60(IU/mL) 30-100150 mg 100-200300 mg 200-300300 mg 300-400225 mg 400-500300 mg 500-600300 mg 600-700375 mgEvery 2 Weeks DosingEvery 4 Weeks DosingApril 27, 2017Body Weight (kg) 60-70 70-90150 mg300 mg225 mg225 mg300 mg375 mgPRESCRIBED DRUGS 90-150150 mg300 mg225 mg300 mg375 mg300 mg225 mg300 mgDO NOT DOSEAppendix A Page 47
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUALCC.Multiple Sclerosis (MS) AgentsAmpyra (dalfampridine)Therapeutic Class: Agents for the treatment of Neuromuscular Transmission DisorderLast Reviewed by the DUR Board: January 23, 2020July 25, 2013MS Agents areAmpyra (dalfampridine) is subject to prior authorization and quantity limitationsbased on the Application of Standards in Section 1927 of the SSA and/or approved by the DURBoard. Refer to the Nevada Medicaid and Check Up Pharmacy Manual for specific quantity limits.1.Coverage and LimitationsAmpyria (dalfampridine)Approval for Ampyra (dalfampridine) will be given if all of the following criteria are metand documented:a.Ampyra (dalfampridine)Approval will be given if all the following criteria aremet and documented:The recipient must meet all of the following:b.2.1.The recipient must have a diagnosis of Multiple SclerosisMS; and2.The medication is being used to improve the recipient’s walking speed; and3.The medication is being prescribed by or in consultation with a neurologist;and4.The recipient is ambulatory and has an EDSS score between 2.5 and 6.5;and5.The recipient does not have moderate to severe renal dysfunction (CrCL 50 ml/min); and6.The recipient does not have a history of seizures; and7.The recipient is not currently pregnant or attempting to conceive.Prior Authorization Guidelines1.Initial prior authorization approval will be for three months.2.Request for continuation of therapy will be approved for one year.Relapsing Forms of MS Agents:a.Approval will be given if all the following criteria are met and documented:1.October 1, 2015The recipient must have a diagnosis of a relapsing form of MS (e.g.,relapsing-remitting MS, secondary-progressive MS with relapses).PRESCRIBED DRUGSAppendix A Page 69
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUALb.Lemtrada (alemtuzumab)1.Approval will be given if all the following criteria are met anddocumented:a.The recipient must have a diagnosis of a relapsing form of MS; andone of the following:1.2.October 1, 2015Both the following:a.The recipient has not been previously treated withalemtuzumab; andb.The recipient has had failure after a trial of at leastfour weeks; a contraindication or intolerance to twoof the following disease-modifying therapies forMS:1.Aubagio (teriflunomide)2.Avonex (interferon beta-1a)3.Betaseron (interferon beta-1b)4.Copaxone/Glatopa (glatiramer acetate)5.Extavia (interferon beta-1b)6.Gilenya (fingolimod)7.Lemtrada (alemtuzumab[CK1])8.Mayzent (siponimod)9.Ocrevus (ocrelizumab)10.Plegridy (peginterferon beta-1a)11.Rebif (interferon beta-1a)12.Tecfidera (dimethyl fumarate)13.Tysabri (natalizumab); orBoth the following:PRESCRIBED DRUGSAppendix A Page 70
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUAL3.2.c.The recipient has previously received treatmentwith alemtuzumab; andb.The recipient has had at least 12 months elapsed orwill have elapsed since the most recent treatmentcourse with alemtuzumab; andThe medication will not be used in combination withanother disease-modifying therapy for MS.Prior Authorization Guidelinesa.Initial authorization approval will be for 12 months.b.Recertification approval will be for 12 months.c.Prior Authorization forms are available .aspx.Mavenclad (cladribine)1.Approval will be given if all the following criteria are met anddocumented:a.The recipient must have a diagnosis of a relapsing form of MS(e.g., relapsing-remitting MS, secondary-progressive MS withrelapses); and one of the following:1.October 1, 2015a.Both the following:a.The recipient has not been previously treated withcladribine; andb.The recipient has had failure after a trial of at leastfour weeks; contraindication, or intolerance to twoof the following disease-modifying therapies forMS:1.Aubagio (teriflunomide)2.Avonex (interferon beta-1a)3.Betaseron (interferon beta-1b)4.Copaxone/Glatopa (glatiramer acetate)PRESCRIBED DRUGSAppendix A Page 71
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUAL2.b.2.d.Extavia (interferon beta-1b)6.Gilenya (fingolimod)7.Lemtrada (alemtuzumab)8.Mayzent (siponimod)9.Ocrevus (ocrelizumab)10.Plegridy (peginterferon beta-1a)11.Rebif (interferon beta-1a)12.Tecfidera (dimethyl fumarate)13.Tysabri (natalizumab); orBoth the following:a.The recipient has previously received treatment withcladribine; andb.The recipient has not already received the FDArecommended lifetime limit of two treatment courses(or four treatment cycles total) of cladribine; andThe medication will not be used in combination with anotherdisease-modifying therapy for MS.Prior Authorization Guidelinesa.Prior authorization approval will be for one month.b.Prior Authorization forms are available .aspx.Ocrevus (ocrelizumab)1.Approval will be given if all the following criteria are met and documented:a.October 1, 20155.The recipient has a diagnosis of a relapsing form of MS (e.g.,relapsing-remitting MS, secondary-progressive MS with relapses);andPRESCRIBED DRUGSAppendix A Page 72
APPENDIX A – Coverage and LimitationsDIVISION OF HEALTH CARE FINANCING AND POLICYMEDICAID SERVICES MANUAL2.3.3.b.The medication must not be used in combination with anotherdisease-modifying therapy for MS; andc.The medication must not be used in combination with another Bcell targeted therapy (e.g., rituximab [Rituxan], belimumab[Benlysta], ofatumumab [Arzerra]); andd.The medication must not be used in combination with anotherlymphocyte trafficking blocker (e.g., alemtuzumab [Lemtrada],mitoxantrone).Recertification Request (the recipient must meet all criteria):a.Documentation of a positive clinical response to Ocrevus therapy;andb.The medication must not be used in combination with anotherdisease-modifying therapy for MS; andc.The medication must not be used in combination with another Bcell targeted therapy (e.g., rituximab [Rituxan], belimumab[Benlysta], ofatumumab [Arzerra]); andd.The medication must not be used in combination with anotherlymphocyte trafficking blocker (e.g., alemtuzumab [Lemtrada],mitoxantrone).Prior Authorization Guidelinesa.Initial prior authorization approval will be 12 months.b.Recertification approval will be for 12 months.c.Prior Authorization forms are available .aspx.Primary Progressive Forms of Multiple Sclerosis (PPMS) Agents:a.Ocrevus (ocrelizumab)1.Approval will be given if all the following criteria are met and documented:a.October 1, 2015The recipient must have a diagnos
100-200 300 mg 300 mg 300 mg 225 mg 200-300 300 mg 225 mg 225 mg 300 mg 300-400 225 mg 225 mg 300 mg 400-500 300 mg 300 mg 375 mg 500-600 300 mg 375 mg 600-700 375 mg DO NOT DOSE Every 2 Weeks Dosing April 27, 2017 PRESCRIBED DRUGS Appendix A Page 36