Transcription
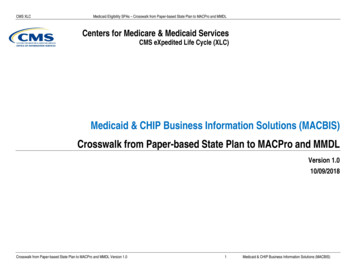
CMS XLCMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLCenters for Medicare & Medicaid ServicesCMS eXpedited Life Cycle (XLC)Medicaid & CHIP Business Information Solutions (MACBIS)Crosswalk from Paper-based State Plan to MACPro and MMDLVersion 1.010/09/2018Crosswalk from Paper-based State Plan to MACPro and MMDL Version 1.01Medicaid & CHIP Business Information Solutions (MACBIS)
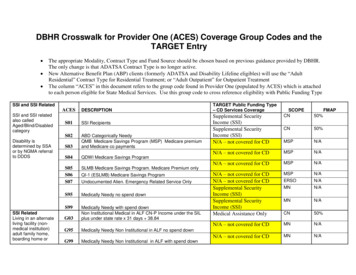
CMS XLCMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDL1. Medicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLThis document lists each provision in Section 2 of the base plan, Attachment 2.2-A, and Attachment 2.6-A of the traditional paper-basedMedicaid state plan. For each provision, you will find a crosswalk to the Medicaid Model Data Lab (MMDL) PDF templates andMACPro reviewable units (RUs) that now contain that information. Because the paper-based state plan has changed over time, thenumbering and language of each provision in this table may not match exactly with the numbering and language in a specific state’sMedicaid state plan. Whenever possible, the statutory and regulatory citations are included to help you identify the provision.Table 1: Crosswalk from Paper-based State Plan to MACPro and MMDLBase Plan/AttachmentSectionPaper-based State Plan ProvisionMMDLPDF Name(s)MACProRU Name(s)Base PlanN/AN/AN/AN/ABase Plan2.1S94: Eligibility ProcessEligibility ProcessBase Plan2.1NoneFuture DevelopmentBase Plan2.1NoneQualified Medicare BeneficiariesBase Plan2.1a. The Medicaid agency meets all requirements of 42 CFRPart 435, Subpart J for processing applications, determiningeligibility, and furnishing Medicaid (435.10 and Subpart J)b.1. Except as provided in b.2. and b.3., individuals areentitled to Medicaid services under the plan during the 3months preceding the month of application (435.914,1902(a)(34))b.2. For individuals eligible as Qualified MedicareBeneficiaries, coverage is available for services furnishedafter the end of the month in which the individual is firstdetermined to be a QMB (1902(e)(8) and 1905(a))b.3. Pregnant women are entitled to ambulatory prenatalcare during a presumptive eligibility period (1902(a)(47))Base PlanBase Plan2.12.1Base Plan2.1S28: Eligibility Groups– MandatoryCoverage: PregnantWomenc. REMOVEDN/Ad. The Medicaid agency has procedures to take applications, S94: Eligibility Processassist applicants, and perform initial processing ofapplications from low-income pregnant women andchildren at outstationed locations (1902(a)(55))e. Express Lane EligibilityNoneCrosswalk from Paper-based State Plan to MACPro and MMDL Version 1.02Presumptive Eligibility forPregnant WomenN/AEligibility ProcessFuture DevelopmentMedicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase Plan/AttachmentBase PlanMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSection2.2Base Plan2.2Base Plan2.2Base Plan2.3Base Plan2.4Base Plan2.5Base Plan2.6Paper-based State Plan ProvisionMMDLPDF Name(s)MACProRU Name(s)Coverage and Conditions of EligibilityMedicaid is available to the groups specified in Attachment2.2-A.NoneThe conditions of eligibility that must be met are specifiedin Attachment 2.6-A.All applicable requirements of 42 CFR Part 435 and sections1902(a)(10)(A)(i)(IV), (V), and (VI), 1902(a)(10)(A)(ii)(XI),1902(a)(10)(E), 1902(l) and (m), 1905(p), (q) and (s), 1920,and 1925 of the Act are met.ResidenceMedicaid is furnished to eligible individuals who areresidents of the state under 42 CFR 435.403, regardless ofwhether or not the individuals maintain the residencepermanently or maintains it at a fixed address.BlindnessAll of the requirements of 42 CFR 435.530 and 42 CFR435.531 are met. The more restrictive definition ofblindness in terms of ophthalmic measurement used in thisplan is specified in Attachment 2.2-A.DisabilityAll of the requirements of 42 CFR 435.540 and 435.541 aremet. The state uses the same definition of disability usedunder the SSI program unless a more restrictive definitionof disability is specified in Item A.13.b. of Attachment 2.2-Aof this plan.Financial Eligibilitya. The financial eligibility conditions for Medicaid-onlyeligibility groups and for persons deemed to be cashassistance recipients are described in Attachment 2.6-A.(435.10 and Subparts G & H)NoneSee relevant eligibility group RUsNoneSee relevant eligibility group RUsS88: State ResidencyState ResidencyNoneFuture DevelopmentNoneFuture DevelopmentNoneSee relevant eligibility group RUsCrosswalk from Paper-based State Plan to MACPro and MMDL Version 1.0Mandatory Eligibility GroupsOptional Eligibility Groups3Medicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase Plan/AttachmentMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionBase Plan2.7Attachment2.2-AN/AAttachment2.2-AA – MandatoryCoverageGroupsPaper-based State Plan ProvisionMMDLPDF Name(s)Medicaid Furnished Out of StateMedicaid is furnished under the conditions specified in 42CFR 431.52 to an eligible individual who is a resident of thestate while the individual is in another state, to the sameextent that Medicaid is furnished to residents in the state.NoneFuture DevelopmentN/AN/AN/A1. Recipients of AFDC (435.110)S28: Eligibility Groups– MandatoryCoverage: PregnantWomenPregnant WomenS30: Eligibility Groups– MandatoryCoverage: Infants andChildren under Age19Attachment2.2-AA – MandatoryCoverageGroupsMACProRU Name(s)2. Deemed recipients of AFDC (1902(a)(10)(A)(i)(I))Crosswalk from Paper-based State Plan to MACPro and MMDL Version 1.0S25: Eligibility Groups– MandatoryCoverage: Parentsand Other CaretakerRelativesNoneInfants and Children under Age 19Parents and Other CaretakerRelativesExtended Medicaid due to SpousalSupport CollectionsChildren with Title IV-E AdoptionAssistance, Foster Care orGuardianship Care4Medicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase Plan/AttachmentMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLMMDLPDF Name(s)MACProRU Name(s)SectionPaper-based State Plan ProvisionAttachment2.2-AA – MandatoryCoverageGroupsN/A – obsoleteN/A – obsoleteAttachment2.2-AA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroups3. Qualified Family Members who would be eligible toreceive AFDC under section 407 of the Act because theprincipal wage earner is unemployed (407(b),1902(a)(10)(A)(i) and 1905(m)(1))4. TMA - Families terminated from AFDC solely because ofearnings, hours of employment, or loss of earned incomedisregards (1902(a)(52) and 1925)5. Individuals who are ineligible for AFDC solely because ofeligibility requirements that are specifically prohibitedunder Medicaid. (435.113)6. Individuals who would be eligible for AFDC except for theincrease in OASDI benefits under PL 92-336 (435.114)NoneTransitional Medical AssistanceN/A – obsoleteN/A – obsoleteN/A – obsoleteN/A – obsolete7. Qualified pregnant women and children(1902(a)(10)(A)(i)(III), 1905(n))S28: Eligibility Groups– MandatoryCoverage: PregnantWomenPregnant Attachment2.2-AA – MandatoryCoverageGroups8. Pregnant women and infants under 1 year of age withfamily incomes up to 133 percent of the FPL(1902(a)(10)(A)(I)(iv) and 1902(l)(1)(A) and (B))S30: Eligibility Groups– MandatoryCoverage: Infants andChildren under Age19S28: Eligibility Groups– MandatoryCoverage: PregnantWomenInfants and Children under Age 19Pregnant WomenInfants and Children under Age 19S30: Eligibility Groups– MandatoryCoverage: Infants andChildren under Age19Crosswalk from Paper-based State Plan to MACPro and MMDL Version 1.05Medicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase Plan/AttachmentMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionPaper-based State Plan ProvisionAttachment2.2-AA – MandatoryCoverageGroupsAttachment2.2-AA – MandatoryCoverageGroupsAttachment2.2-AA – MandatoryCoverageGroups9. Children (a) who have attained 1 year of age but have notattained 6 years of age, with family incomes at or below 133percent of the FPL; and (b) born after September 30, 1983,who have attained 6 years of age but have not attained 19years of age, with family incomes at or below 100 percentof the FPL (1902(a)(10)(A)(I)(iv) and (vii) and 1902(l)(1)(C)and (D))10. Individuals other than qualified pregnant women andchildren under A.7. who are members of a family thatwould be receiving AFDC if the state had not exercised theoption under 407(b)(2)(a)(i) to limit the number of monthsfor which a family may receive AFDC (1902(a)(10)(A)(i)(V)and 1905(m))11a. 60 days postpartum coverage for pregnant women(1902(e)(5))Attachment2.2-AA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – 2-AAttachment2.2-AAttachment2.2-AMMDLPDF Name(s)MACProRU Name(s)S30: Eligibility Groups– MandatoryCoverage: Infants andChildren under Age19Infants and Children under Age 19N/A – obsoleteN/A – obsoletePregnant Women11b. continuous eligibility for pregnant women (1902(e)(6))S28: Eligibility Groups– MandatoryCoverage: PregnantWomenNone12. deemed newborns (1902(e)(4))NoneDeemed Newborns13a. SSI recipients (435.120)NoneSSI Beneficiaries13b. 209(b) group (435.121)None14. Qualified severely impaired blind and disabledindividuals under age 65 (1902(a)(10)(A)(i)(II) and 1905(q))NoneIndividuals in 209(b) States WhoAre Age 65 or Older or Who haveBlindness or a DisabilityWorking Individuals Under 1619(b)Crosswalk from Paper-based State Plan to MACPro and MMDL Version 1.06Future DevelopmentMedicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase 2.2-AAttachment2.2-AMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsAttachment2.2-AA – MandatoryCoverageGroupsAttachment2.2-AA – MandatoryCoverageGroupsPaper-based State Plan ProvisionMMDLPDF Name(s)15. Except in states that apply more restrictive eligibilityNonerequirements for Medicaid than under SSI, blind or disabledindividuals who lose SSI due to OASDI child’s benefits16. Except in states that apply more restrictiveN/A – obsoleterequirements, individuals who are ineligible for SSI oroptional state supplements due to requirements that do notapply under title XIX (435.122)17. Individuals receiving mandatory state supplementsNone(435.130)18. Individuals eligible as essential spouses in December1973 (435.131)None19. Institutionalized individuals eligible in 1973 (435.132)None20. Blind and disabled individuals who were eligible in 1973(435.133)None21. Individuals who would be SSI/SSP eligible except for theincrease in OASDI benefits in 1972 (435.134)None22. Individuals who are receiving OASDI and were receiving NoneSSI/SSP but became ineligible for SSI/SSP as a result ofOASDI cost-of-living increases received after April 1977(435.135)23. Disabled widows and widowers who would be eligibleNonefor SSI/SSP except for the increase in their OASDI benefits asa result of the elimination of the reduction factor requiredby section 134 of P.L. 98-21 and who are deemed to beSSI/SSB beneficiaries under section 1634(b) of the ActCrosswalk from Paper-based State Plan to MACPro and MMDL Version 1.07MACProRU Name(s)Individuals Deemed To BeReceiving SSI – Adult Children withDisabilitiesN/A – obsoleteClosed Eligibility Groups –Individuals Receiving MandatoryState SupplementsClosed Eligibility Groups –Individuals Who Are EssentialSpousesClosed Eligibility Groups Institutionalized IndividualsContinuously Eligible Since 1973Closed Eligibility Groups –Individuals Eligible in 1973 WhoHave Blindness or a DisabilityClosed Eligibility Groups Individuals Who Lost Eligibility forSSI/SSP Due to an Increase inOASDI Benefits in 1972Individuals Deemed To BeReceiving SSI - Individuals WhoWould be Eligible for SSI/SSP butfor OASDI COLA IncreasesClosed Eligibility Groups - DisabledWidows and Widowers Ineligiblefor SSI due to Increase in OASDIMedicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase 2.2-AMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsA – MandatoryCoverageGroupsB – OptionalGroupsPaper-based State Plan ProvisionMMDLPDF Name(s)MACProRU Name(s)24. Disabled widows, widowers, and unmarried divorcedspouses ineligible for SSI due to early receipt of socialsecurity (1634(d))25. Qualified Medicare beneficiariesNone26. Qualified disabled and working individualsNoneQualified Disabled and WorkingIndividuals27. Specified low-income Medicare beneficiariesNoneSpecified Low Income MedicareBeneficiaries28. Qualifying IndividualsNoneQualifying Individuals1. Individuals who meet the income and resourcerequirements of AFDC/SSI/SSP but do not receive cashassistance (435.210)S51: Eligibility Groups– Options forCoverage: OptionalCoverage of Parentsand Other CaretakerRelativesOptional Coverage of Parents andOther Caretaker RelativesNoneIndividuals Deemed To BeReceiving SSI – Disabled Widowsand WidowersQualified Medicare BeneficiariesIndividuals Eligible for but NotReceiving Cash AssistanceAttachment2.2-AB – OptionalGroups2. Individuals who would be eligible for AFDC/SSI/SSP if notin a medical institution (435.211)NoneIndividuals Eligible for Cash Exceptfor InstitutionalizationAttachment2.2-AB – OptionalGroups3. Individuals who become otherwise ineligible for Medicaidwhile enrolled in an MCO or PCCM (435.212)NoneFuture DevelopmentCrosswalk from Paper-based State Plan to MACPro and MMDL Version 1.08Medicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase Plan/AttachmentAttachment2.2-AMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionB – OptionalGroupsPaper-based State Plan ProvisionMMDLPDF Name(s)MACProRU Name(s)4. Individuals who would be eligible for Medicaid if theywere in a nursing facility or ICF/MR, who but for theprovision of home and community based services under awaiver (435.217) or PACE enrollment would requireinstitutionalizationNone5. Individuals who would be eligible for Medicaid if theywere in a medical institution, who are terminally ill, andwho receive hospice care6. Individuals who would be eligible for AFDC if their workrelated child care costs were paid from earnings (435.220)NoneIndividuals Receiving HospiceN/A – obsoleteN/A – obsoleteS52: Eligibility Groups– Options forCoverage:ReasonableClassification ofIndividuals under Age21S53: Eligibility Groups– Options forCoverage: Childrenwith Non IV-EAdoption AssistanceN/A – obsoleteReasonable Classifications ofIndividuals under Age 21PACE ParticipantsAttachment2.2-AB – OptionalGroupsAttachment2.2-AB – OptionalGroupsAttachment2.2-AB – OptionalGroups7. Individuals who are not described in 1902(a)(1)(A)(i) ofthe Act, who meet the income and resource requirementsof the AFDC state plan, and who are under 21 years of age,or reasonable classifications of such individuals (435.222)Attachment2.2-AB – OptionalGroups8. A child for whom there is in effect a state adoptionassistance agreement (other than under title IV-E of theAct) (1902(a)(10)(A)(ii)(VIII)Attachment2.2-AB – OptionalGroupsAttachment2.2-AB – OptionalGroups9. Individuals who would be eligible for AFDC if coverageunder the state’s AFDC plan were as broad as allowed undertitle IV-A (435.223)10. Individuals who receive only a state supplementaryNonepayment (states using SSI criteria with agreements undersections 1616 and 1634 of the Act) (435.230)Crosswalk from Paper-based State Plan to MACPro and MMDL Version 1.0Individuals Receiving Home andCommunity Based Waiver Servicesunder Institutional Rules9Children with Non-IV-E AdoptionAssistanceN/A – obsoleteOptional State SupplementBeneficiariesMedicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase Plan/AttachmentMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionAttachment2.2-AB – OptionalGroupsAttachment2.2-AB – OptionalGroupsAttachment2.2-AB – OptionalGroupsAttachment2.2-AB – OptionalGroupsPaper-based State Plan Provision11. Individuals who receive a state supplementary payment(section 1902(f) states and SSI criteria states withoutagreements under section 1616 or 1634 of the Act)12. Individuals who are in institutions for at least 30consecutive days and who are eligible under a specialincome level (435.231)13. Certain disabled children age 18 who are living at home,who would be eligible for Medicaid under the plan if theywere in a medical institution (1902(e)(3))14. Pregnant women and/or infants who are not mandatorycategorically needy whose income does not exceed anincome level established by the state (1902(a)(10)(A)(ii)(IX)and 1902(l))Attachment2.2-AB – OptionalGroups15. Children who are not mandatory categorically needywhose income does not exceed an income level establishedby the state (1902(a)(10)(A)(ii)(IX) and 1902(l)(1)(D))Attachment2.2-AB – OptionalGroupsAttachment2.2-AB – OptionalGroups16. Individuals who are age 65 or older or are disabled,whose income does not exceed 100% FPL(1902(a)(10)(A)(ii)(X), 1902(m)(1) and (3))17. Presumptive eligibility for pregnant women (1902(a)(47)and 1920)Attachment2.2-AB – OptionalGroups18. Individuals required to enroll in cost-effective employerbased group health plans remain eligible for a minimumenrollment period (1906)Crosswalk from Paper-based State Plan to MACPro and MMDL Version 1.0MMDLPDF Name(s)MACProRU Name(s)NoneOptional State SupplementBeneficiariesNoneIndividuals in Institutions Eligibleunder a Special Income LevelNoneChildren under Age 19 with aDisabilityS28: Eligibility Groups– MandatoryCoverage: PregnantWomenPregnant WomenS30: Eligibility Groups– MandatoryCoverage: Infants andChildren under Age19S30: Eligibility Groups– MandatoryCoverage: Infants andChildren under Age19NoneS28: Eligibility Groups– MandatoryCoverage: PregnantWomenNone10Infants and Children under Age 19Infants and Children under Age 19Age and Disability-Related PovertyLevelPresumptive Eligibility forPregnant WomenFuture DevelopmentMedicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase Plan/AttachmentMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionPaper-based State Plan ProvisionMMDLPDF Name(s)MACProRU Name(s)Attachment2.2-AB – OptionalGroups19. Individuals entitled to COBRA continuation coverage(1902(a)(10)(F) and 1902(u)(1))NoneIndividuals Electing COBRAContinuation CoverageAttachment2.2-AB – OptionalGroups20. Optional targeted low income children(1902(a)(10)(A)(ii)(XIV))Optional Targeted Low IncomeChildrenAttachment2.2-AB – OptionalGroupsS54: Eligibility Groups– Options forCoverage: OptionalTargeted Low IncomeChildrenNoneAttachment2.2-AB – OptionalGroupsAttachment2.2-AB – OptionalGroupsAttachment2.2-AB – OptionalGroups21. Children under a specified age who have beendetermined eligible and are deemed to be eligible for a totalof 12 months regardless of changes in circumstances(1902(e)(12))22. Presumptive eligibility for children under age 19 (1920)S30: Eligibility Groups– MandatoryCoverage: Infants andChildren under Age1923. Women who have been screened for breast or cervicalNonecancer under the CDC’s Breast and Cervical Cancer EarlyDetection Program (1902(a)(10)(A)(ii)(XVIII))24. Presumptive eligibility for the breast and cervical cancer Noneearly detection program eligibility group (1920B)Attachment2.2-AB – OptionalGroups25. Individuals infected with tuberculosis(1902(a)(10)(A)(ii)(XII) and 1902(z))Attachment2.2-AB – OptionalGroups26. Family Opportunity Act (1902(a)(10)(A)(ii)(XIX))Crosswalk from Paper-based State Plan to MACPro and MMDL Version 1.0S55: Eligibility Groups– Options forCoverage: Individualswith TuberculosisNone11Future DevelopmentPresumptive Eligibility for ChildrenUnder Age 19Individuals Needing Treatment forBreast or Cervical CancerIndividuals Needing Treatment forBreast or Cervical Cancer –Presumptive EligibilityIndividuals with TuberculosisFamily Opportunity Act Childrenwith a DisabilityMedicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase Plan/AttachmentMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionPaper-based State Plan ProvisionMMDLPDF Name(s)MACProRU Name(s)S57: Eligibility Groups– Options forCoverage:Independent FosterCare AdolescentsNoneIndependent Foster CareAdolescents29. TWWIIA Basic Coverage Group (1902(a)(10)(A)(ii)(XV))NoneTicket to Work BasicB – OptionalGroups30. TWWIIA Medical Improvement Group(1902(a)(10)(A)(ii)(XVI))NoneTicket to Work MedicalImprovementsB – OptionalGroups31. Individuals who are eligible for home and communitybased services under the needs based criteria establishedunder section 1915(i)(1)(A) and have income that does notexceed 150% of the FPL, or who are eligible for home andcommunity-based services under a waiver approved for theState under section 1915(c), (d) or (e) or section 1115 andwhose income does not exceed 300% of the supplementalsecurity income benefit rate32. Family planning – individuals who are not pregnant andwhose income does not exceed the state establishedincome standard (1902(a)(10)(A)(ii)(XXI))NoneIndividuals Receiving State PlanHome and Community-BasedServicesAttachment2.2-AB – OptionalGroups27. Independent foster care -AB – OptionalGroups28. BBA Work Incentives Eligibility Group(1902(a)(10)(A)(ii)(XIII))Attachment2.2-AB – ment2.2-AB – OptionalGroupsAttachment2.2-AB – OptionalGroups33. Presumptive eligibility for family planningCrosswalk from Paper-based State Plan to MACPro and MMDL Version 1.0S59: Eligibility Groups– Options forCoverage: IndividualsEligible for FamilyPlanning ServicesS59: Eligibility Groups– Options forCoverage: IndividualsEligible for FamilyPlanning Services12Work IncentivesIndividuals Receiving State PlanHome and Community-BasedServices who are OtherwiseEligible for HCBS WaiversIndividuals Eligible for FamilyPlanning ServicesIndividuals Eligible for FamilyPlanning Services – PresumptiveEligibilityMedicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase Plan/AttachmentMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionAttachment2.2-AC – MedicallyNeedyAttachment2.2-AC – MedicallyNeedyAttachment2.2-AAttachment2.2-AC – MedicallyNeedyC – MedicallyNeedyAttachment2.2-AC – MedicallyNeedyAttachment2.2-AAttachment2.2-AC – MedicallyNeedyC – MedicallyNeedyAttachment2.2-APaper-based State Plan ProvisionMMDLPDF Name(s)MACProRU Name(s)1. Pregnant women who, except for income and/orresources, would be eligible as categorically needy undertitle XIX of the Act2. Women who, while pregnant, were eligible as medicallyneedy, continue to be eligible for 60 days postpartum(1902(e))3. Individuals under age 18 who, but for income would beeligible under section 1902(a)(10)(A)(i) (1902(a)(10)(C)(ii)(I))4. Newborn children born on or after October 1, 1984 to awoman who is eligible as medically needy and is receivingMedicaid on the date of the birth (1902(e)(4))5. Financially eligible individuals who are not described inC.3. who are under the age of 21, or reasonableclassifications of individuals under 21 (435.308)6. Caretaker relatives (435.310)NoneMedically Needy Pregnant WomenNoneMedically Needy Pregnant WomenNoneMedically Needy Children underAge 18Deemed Newborns7. Aged individuals (435.320 and 435.330)NoneC – MedicallyNeedy8. Blind individuals (435.322 and 435.330)NoneAttachment2.2-AC – MedicallyNeedy9. Disabled individuals (435.324 and 435.330)NoneAttachment2.2-AAttachment2.2-AC – MedicallyNeedyC – MedicallyNeedy10. Individuals who would be ineligible if they were notNoneenrolled in an HMO (435.326)11. Blind and disabled individuals who meet all currentNonerequirements for Medicaid eligibility except the blindness ordisability criteria, were eligible as medically needy inDecember 1973 and have continued to meet those criteriaevery month since thenCrosswalk from Paper-based State Plan to MACPro and MMDL Version 1.0NoneNoneNone13Medically Needy ReasonableClassifications of Individuals underAge 21Medically Needy Parents andOther Caretaker RelativesMedically Needy PopulationsBased on Age, Blindness orDisabilityMedically Needy PopulationsBased on Age, Blindness orDisabilityMedically Needy PopulationsBased on Age, Blindness orDisabilityFuture DevelopmentProtected Medically NeedyIndividuals Who Were Eligible in1973Medicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase Plan/AttachmentMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionAttachment2.2-AC – on CSupplement lement 2Attachment2.6-AA – Eachindividualcovered underthe plan:A – Eachindividualcovered underthe plan:Attachment2.6-AAttachment2.6-ASupplement 3N/APaper-based State Plan Provision12. Individuals required to enroll in cost effective employerbased group health plans remain eligible for a minimumperiodThe agency provides for making Medicare prescription drugLow Income Subsidy determinations under Section 1935(a)of the Social Security Act.Reasonable Classifications of Individuals Under the Age of21, 20, 19, or 18A. Definition of Blindness in Terms of OpthalmicMeasurementMethod for Determining Cost Effectiveness of Caring forCertain Disabled Children at HomeMMDLPDF Name(s)MACProRU Name(s)NoneFuture DevelopmentNoneFuture DevelopmentS52: Eligibility Groups– Options forCoverage:ReasonableClassification ofIndividuals under Age21NoneReasonable Classifications ofIndividuals under Age 21NoneChildren under Age 19 with aDisabilityFuture DevelopmentN/AN/A1. Is financially eligible (using the methods and standardsdescribed in Parts B and C of this attachment) to receiveservices. (Part 435 Subpart G)NoneSee relevant eligibility group RUs2.a. Meets the applicable non-financial eligibilityrequirements (Part 435 Subpart F) for the categoricallyneedy:(i) Except as specified under items A.2.a.(ii) and (iii) below,for AFDC-related individuals, meets the non-financialeligibility conditions of the AFDC program.(ii) For SSI-related individuals, meets the non-financialrequirements of the SSI program or the more restrictive SSIrelated categorically needy criteria.NoneSee relevant eligibility group RUsCrosswalk from Paper-based State Plan to MACPro and MMDL Version 1.014N/AMedicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase 2.6-AMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLSectionA – Eachindividualcovered underthe plan:Paper-based State Plan Provision2.a.(iii) For financially eligible pregnant women, infants orchildren, meets the non-financial criteria of section 1902(l)of the Act.A – Eachindividualcovered underthe plan:A – Eachindividualcovered underthe plan:2.a.(iv) For financially eligible aged and disabled individualscovered under section 1092(a)(10)(A)(ii)(X) of the Act,meets the non-financial criteria described in section1902(m) of the Act.2.a.(v) For children receiving State adoption assistance whoare financially eligible under section 1902(a)(10)(A)(ii)(VIII)of the Act, meets the non-financial eligibility criteria of thatsection.A – Eachindividualcovered underthe plan:A – Eachindividualcovered underthe plan:2.a.(vi) For tuberculosis-infected individuals financiallyeligible under section 1902(a)(10)(A)(ii)(XII) of the Act,meets the non-financial eligibility criteria of section 1902(z).A – Eachindividualcovered underthe plan:2.a.(viii) For independent foster care adolescents financiallyeligible under 1902(a)(10)(A)(ii)(XVII) of the Act, meets thenon-financial eligibility criteria of section 1905(w).2.a.(vii) For optional targeted low-income childrenfinancially eligible under section 1902(a)(10)(A)(ii)(XIV) ofthe Act, meets the non-financial eligibility criteria of section1905(u)(2)(B).Crosswalk from Paper-based State Plan to MACPro and MMDL Version 1.0MMDLPDF Name(s)S28: Eligibility Groups– MandatoryCoverage: PregnantWomenS30: Eligibility Groups– MandatoryCoverage: Infants andChildren under Age19NoneS53: Eligibility Groups– Options forCoverage: Childrenwith Non IV-EAdoption AssistanceS55: Eligibility Groups– Options forCoverage: Individualswith TuberculosisS54: Eligibility Groups– Options forCoverage: OptionalTargeted Low IncomeChildrenS57: Eligibility Groups– Options forCoverage:Independent FosterCare Adolescents15MACProRU Name(s)Pregnant WomenInfants and Children under Age 19Age and Disability-Related PovertyLevelChildren with Non-IV-E AdoptionAssistanceIndividuals with TuberculosisOptional Targeted Low IncomeChildrenIndependent Foster CareAdolescentsMedicaid & CHIP Business Information Solutions (MACBIS)
CMS XLCBase 2.6-AAttachment2.6-AAttachment2.6-AMedicaid Eligibility SPAs – Crosswalk from Paper-based State Plan to MACPro and MMDLMMDLPDF Name(s)MACProRU Name(s)SectionPaper-based State Plan ProvisionA – Eachindividualcovered underthe plan:A – Eachindividualcovered underthe plan:A – Eachindividualcovered under
CMS XLC Medicaid Eligibility SPAs - Crosswalk from Paper-based State Plan to MACPro and MMDL . Base Plan/ Attachment Section Paper-based State Plan Provision MMDL PDF Name(s) MACPro RU Name(s) Attachment 2.2-A A - Mandatory Coverage Groups 15. Except in states that apply more restrictive eligibility