Transcription
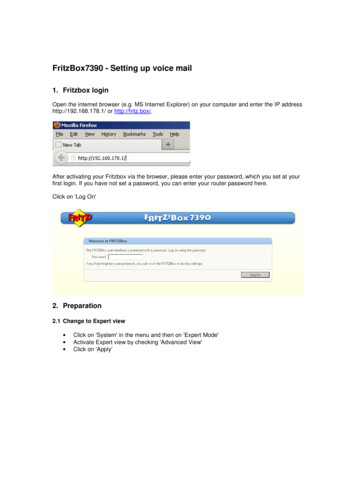
Evaluation of Voice and Voice Disorders Across Practice SettingsJulie Barkmeier-Kraemer, PhD, CCC-SLP, ASHAFEvaluation of Voice and VoiceDisorders Across PracticeSettings, Part 1Speaker Disclosure Financial:– Professor, University of Utah– Speaker Honorarium from ArSHA Nonfinancial:Julie Barkmeier‐Kraemer, PhD, CCC‐SLP,ASHAFUniversity of UtahJulieB.Kraemer@hsc.utah.edu– ASHA member– Member of ASHA’s SIG3: Voiceand Upper Airway Disorders– ASHA working group member forCAPE‐V and Instrumental VoiceAssessment ProtocolsJulie Barkmeier‐Kraemer, PhD, CCC‐SLPUniversity of UtahUpon completion of this course,participants will be able to:1. Identify key components of a voice assessment thatidentify the presence or absence, nature, and severityof a voice disorder2. Identify basic equipment necessary for a voiceassessment in a variety of settings3. Describe appropriate measures of voice used to testhypotheses about and track voice change over time aswell as those related to treatmentOnline Resource Online ASHA Voice Portal as a great resourceto members:– Topics/Voice‐Disorders/ArSHA 20211
What is a voice disorder?The purpose of a voice assessment Two perspectives needed to identify the presence ofa voice disorder:1. An individual (or caregiver) expresses concernthat their (child’s) voice does not meet dailyfunction needs (American Speech‐Language‐Hearing Association [ASHA], 1993;Colton & Casper, 1996; Stemple, Glaze, & Klaben, 2010; Verdolini & Ramig, 2001)2. A voice clinician describes aberrant voicequality, pitch, and/or loudness with regard to the person’s age, gender,cultural background, or geographic location(Aronson & Bless, 2009; Boone, McFarlane, Von Berg, & Zraik, 2010; Lee, Stemple, Glaze, &Kelchner, 2004)The purpose of a voice assessment Assessment outcomes should offerinsights regarding:Case IntakePatient Self‐ReportArSHA bility– Educate/counsel the patient abouthis/her voice problem– Define treatment goals andmethods– Determine treatment outcomesClinical Decisions During Assessment to DriveTreatment Pitch, Loudness, Quality As progress, may expandupon particular parameterswhen evidence points to avoice problem that is:– Neurological– Functional– OrganicSLP Voice Assessment ComponentsCranialNerve Exam(AKA oralperipheralexam) Also can be used to:– Evaluate parameters of voice ASHA practice patterns for SLPsrecommend otolaryngology assessmentpre‐treatmentand resonance (non‐instrumental)– Presence/absence of a voicedisorder– Severity of a voice disorder– Nature of a voice disorder Use a Standard Protocol– Voice function strengths andweaknesses– Impact of the voice problem on dailyliving activities– Prognosis for change– Appropriate intervention and support– Appropriate referral(s)CPT 92524 Behavioral and qualitative analysis of voice LaryngealImagingThe Case Intake A thorough case history isimportant to:– Develop hypothesesregarding the voice problem– Inform appropriateevaluation methods– Determine factors that mayinfluence recommendations2
The Case IntakeThe Case Intake Health and Medical History:–––––SurgeriesChronic llowing problemsFor children: Characterize onset andconsistency of the voiceproblem– Pattern of onset– Duration– Consistency– Associated symptoms andsensations Developmental history Impact on learning/participation Patient description of their voice problem Patient report of previous voice treatment Daily habits/vocal hygieneSLP Voice Assessment ComponentsCPT 92524 Behavioral and qualitative analysis of voiceand resonance (non‐instrumental)Case IntakePatient Self‐ReportCranialNerve Exam(AKA tionStudiesLaryngealImagingSelf‐Report Voice Instruments Several instruments are available for use(nonexhaustive list):– ADULTS Voice Handicap Index (VHI) Voice Handicap Index‐10 (VHI‐10) Singing Voice Handicap Index (sVHI) Voice‐Related Quality of Life (V‐RQOL) Voice Symptom Scale (VoiSS)– PEDIATRICS Pediatric Voice Handicap Index (pVHI) Pediatric Voice‐Related Quality of Life (pV‐RQOL) Pediatric Voice Symptom Questionnaire (PVSQ) Pediatric Quality of Life (peds QL) (Ages 8‐12 years)– http://www.pedsql.org/ArSHA 2021Self‐Report Voice Instruments Caregiver or self‐report tools toassess the impact of the voicedisorder on:– Function– Quality of life– Pre‐/Post‐treatment changesVoice Handicap Index (VHI) Developed using psychometric methodology(Jacobson et al, 1997) Strong validity and reliability for– Presence/absence– Severity of a voice problem Translated and psychometrically tested inmore than 30 different languages3
VHI: 30 items, 3 SubscalesTest‐Retest ReliabilityHow Much Change Matters?1. Functional: Impact of a person’s voice disorder on dailyactivities “My voice problem causes me to miss work.” The maximum total score is 120 A change in VHI score is considered to besignificant change IF:2. Emotional: Patient’s emotional response to his/her voicedisorder “I feel annoyed when people ask me to repeat.”3. Physical: Self‐perceptions of laryngeal discomfort and voicecharacteristics “I feel as though I have to strain to produce voice.”– Subset shift of 8 points or more, or– Self‐ratings from “never” (0) to “always” (4) on a 5‐pointequal‐appearing interval scale– Total score shift of 18 points or more(Jacobson et al.,1997)Pediatric VHI (pVHI)SLP Voice Assessment Components Modified VHI to reflect caregiverviewpointCPT 92524 Behavioral and qualitative analysis of voice– 23 items across the 3 subscales(functional, physical, emotional)and resonance (non‐instrumental)– Psychometric testing on a smallcohort (Zur et al, 2007)Case Intake Distinguishes between childrenwith and without a voice disorderPatient Self‐ReportCranialNerve Exam(AKA tionStudiesLaryngealImaging(Lu et al, 2018)– 418 parents of children aged 2‐14years of age (Mandarin language)StructurePeripheral Oral ExamTHREE COMPONENTSJawFace/Lips1. OBSERVE STRUCTURES AT“REST” POSTURE Integrity Tone & SymmetryTongue2. MOTOR ASSESSMENT Strength Range of Motion Coordination for speech and non‐speech tasks3. SENSORY ASSESSMENT General sensation Taste HearingVVVBig smileKissBlow through pursed lipsVIIVIIVIIReport sensation to light touch ofcotton swab at L/R forehead,cheek bone, mandible (eyesclosed)ProtrudeLick lipsSide‐to‐sideTongue tip upwardTongue tip downwardProtrude against resistancePush against inside L/R cheekagainst resistanceApply sugar/salt solution toanterior protruded tongue withcotton swabObserve soft palate symmetry andPalate/Larynx elevation during sustainedphonation of /a/CN SensoryVXIIXIIXIIXIIXIIXIIXIIVIITest ability to feel cotton swab onL/R tongue dorsum (eyes closed)VXAlternating Non‐Speech MovementsBite‐BlowSmile‐KissKiss‐Tongue OutBite‐Mouth OpenV, VIIVII, VIIVII, XIIV, VVVVVDiadochokinetic Rates & IntegrityRepeat "uh‐uh " 20xRepeat /p / 20xRepeat /t / 20xRepeat /k / 20xRepeat /p t k / 10xXVII, V, XXII, VXII, VV, VII, XIIVVVVHearingArSHA 2021SENSORIMOTOR ASSESSMENTTaskCN MotorOpen Mouth wideBite and hold against resistanceRepeatedly bite and click teethWhisper a number in each earand ask them to repeat itVIII4
SLP Voice Assessment ComponentsCPT 92524 Behavioral and qualitative analysis of voiceand resonance (non‐instrumental)Case IntakeParameters of VoicePatient Self‐ReportCranialNerve Exam(AKA tionStudiesLaryngealImagingAuditory‐Perceptual Testing Most common methodused by voice clinicians STANDARD PROTOCOLNEEDED:Auditory‐Perceptual Pitch Loudness QualityAcoustic/AerodynamicPhysiological Fundamentalfrequency (Fo) Intensity (dB SPL) Spectral components(CPP) Vocal fold (VF) vibrationrate Subglottal pressure, VFclosure degree/duration VF configuration,symmetry resonance– Standard speech stimuli– Consistent rating scalefor judging voice quality– Standard set of stimuli totrain clinicians to use theinstrument– Standard anchor stimuliCompleted Using InstrumentationConsensus Auditory‐Perceptual Evaluation of Voice(CAPE‐V)1. Sustained vowels, /a/ and /i/, for 3‐5 seconds duration each2. Sentence reading:a) The blue spot is on the key again. (English vowels)b) How hard did he hit him? (Easy voice onset)c) We were away a year ago. (All‐voiced phonemes)d) We eat eggs every Easter. (Glottal stops)e) My mama makes lemon muffins. (Nasal phonemes)f) Peter will keep at the peak. (Voiceless‐Loaded phonemes)3. Spontaneous speech in response to: “Tell me about yourvoice problem,” or “Tell me how your voice is functioning.”Kempster G, Gerratt B, Verdolini K, Barkmeier‐Kraemer J, Hillman R. Consensus Auditory‐Perceptual Evaluation of Voice: Development of aStandardized Clinical Protocol Am. J of Speech‐Lang. Path. 2009; 18(2): 124‐132.ArSHA 2021Kempster et al. 20095
Overall Resonance Perceptual judgment ngealAlveolarBuccal Fogging mirror test (visualevidence) (Chow et al., 2015)– Sustained vowel (/i/)– Single words (e.g., “pea”“tea” “see” “puppy”)– Sentences (e.g., “Sissy sawSally race.”)GRBAS Developed by Hirano (1981) to evaluate pre‐and post‐thyroplasty for vocal fold paralysis Most widely used rating scale until recently forvoice quality The CAPE‐V expanded upon this scale (Kempsteret al., 2009; Zraick et al., 2011)– Structured speech tasks– Visual‐analog scale instead of ordinal ratingsVoice Quality Overall SeverityJudgments – GuidelinesTaken from Hirano (1981), Clinical Examination of the VoiceMildAdditional tasks Maximum Voice Parameters during sustainedphonation– Maximum pitch range Highest pitch Lowest pitch– Maximum loudness range Softest phonation using comfortable pitch Loudest phonation using comfortable pitchArSHA 2021 Trained listener would consider the voice abnormal; untrained listenerwould consider it unusual but normal. The characteristic is notdistracting, and the ability to effectively communicate is not impaired.Moderate Both trained and untrained listeners would consider the voice abnormal.The characteristic is distracting at times, and the ability to effectivelycommunicate is noticeably impaired under certain circumstances.Severe Both trained and untrained listeners would consider the voice extremelyabnormal. The characteristic is highly distracting all the time, and theability to effectively communicate is consistently affected.Case Example 1: AdultCase Intake/VHI 31‐year‐old female with sudden change in voicesubsequent to a radical neck dissection 10months prior to the appointment, due torecurrence of carcinoma Prior medical history of papillary thyroidcarcinoma 4 years prior to most recent surgery,without complications or change of voice Complained of an excessively soft voice anddifficulty projecting her voice and being heardover background noise Frequent vocal fatigue with voice change andonset of aphonia at the end of the day VHI Total Score 114/120 Current Voice Function rated as 10% NormalAuditory‐Perceptual Sustained Phonation Connected Speech6
Case Example 2: PediatricCase Intake/VHIAuditory‐Perceptual 9‐year‐old female with a longstanding history of araspy voice quality, currently in musical theater andstrains during singing. Prior medical history of central apnea with PICUhospitalization and intubation for 1 day of a week longstay, aspiration of a carrot (2 yrs), and tonsillectomy &adenoidectomy (4 yrs). Normal gestation and twin birth (twin has no voiceproblems). Receives twice weekly (20 min) SLP schoolspeech services /r/, "sh, ch, j" during the past year. Reports vocal fatigue with prolonged voicing, frequentthroat clearing, MPT of 6 s, nasal rustle andhypernasality. pVHI Total Score 28/120 Current Voice Function rated as 30‐40% Normal SustainedPhonation ConnectedSpeechSLP Voice Assessment ComponentsCPT 92524 Behavioral and qualitative analysis of voiceand resonance (non‐instrumental)Case IntakeFacilitative Voicing Techniques Used to explore whattherapy methodsimprove voicing Indicates whetherpatient is a candidate forvoice treatment Gives direction to besttreatment methods forfirst session(Yiu et al, 2012; Boone et al., 2014; Gillespie& Gartner‐Schmidt, 2016; Smith & Titze,2017)ArSHA 2021 Examples of my favorites– Semi‐Occluded Vocal TractTechniques Lip/Tongue raspberry Phonation into a straw Kazoo or “Lip Buzz” during“ooh”– Resonance Adjustments Forward voice resonanceTongue protrusionChantingOpen‐mouthHead positioning (also for vocalfold paralysis/paresis)– Yawn‐sign (stretch and relax)– Vegetative voicing (e.g. throatclear, laughter)– Respiratory training– Laryngeal ManipulationPatient Self‐ReportCranialNerve Exam(AKA tionStudiesLaryngealImagingPhysical Exam andVoicing Facilitation Laryngeal palpation andmanipulation can beinformative– Palpable tension– Tenderness or pain– Voicing changes withmanipulation Facilitative voicingmethods can informabout effective therapymethods7
Voice Stimulability & LaryngealManipulation Case Example Consistent voice quality:––––StrainedBreathyReduced loudnessNot phoneme specific Normal vegetative voicing Stimulable for improvedvoiceAdult Case ExampleFacilitative Voicing Laryngeal Manipulation Semi‐occluded vocal tracttechniques– High/Low pitch– Loud phonation Resonant voiceOutcomes Voice quality improved during:– high pitch– Resonant/forward focused voicing– Thyroid cartilage adduction Increased breathy‐rough voicequality:– Lower pitches– At end of utterances Aperiodicity inconsistent withfunctional voice problemDO NOT AUDIO‐, VIDEO‐RECORD, OR PHOTOGRAPHBehavioral Voice AssessmentDiscussionEvaluation of Voice and VoiceDisorders Across PracticeSettings, Part 2Julie Barkmeier‐Kraemer, PhD, CCC‐SLP,ASHAFUniversity of UtahJulieB.Kraemer@hsc.utah.eduVoice Assessment ToolsSLP Voice Assessment ComponentsCPT 92524 Behavioral and qualitative analysis of voiceand resonance (non‐instrumental)Case IntakeArSHA 2021Patient Self‐ReportCranialNerve Exam(AKA tionStudiesLaryngealImaging8
Voice Assessment ParametersAuditory‐Perceptual Pitch Loudness QualityAcoustic/AerodynamicPhysiological Fundamentalfrequency (Fo) Intensity (dB SPL) Spectral components(CPP) Vocal fold (VF) vibrationrate Subglottal pressure, VFclosure degree/duration VF configuration,symmetry resonanceCompleted Using InstrumentationRecommended Acoustic Tasks andMeasures (Patel et al, 2018)MINIMUM RECOMMENDEDRECORDING TASKS Sustained Phonation Tasks [Repeateach task 3 times]MEASURES Sustained phonation of /a/– Average f0– Average SPL– Cepstral Peak Prominence (CPP)from at least 1 second of middlesustained portion of each of 3trials– Sustain /a/ for 3‐5 seconds atcomfortable pitch and loudness on 1breath– Loudness Range Sustain /ɑ/ as softly as possible forat least 2 seconds withoutwhispering Sustain /ɑ/ as loudly as possible forat least 2 seconds – Lowest SPL value sustained for atleast 1 second– Highest SPL value sustained for atleast 1 second– Pitch Range Sustain /a/ at the highest note thatcan be sustained for 2 seconds Sustain /a/ at the lowest note thatdoes not include glottal fry/pulseregister possible for 2 seconds May use a glide to achieve thehighest and lowest notesRecommended Acoustic Tasks andMeasures (Patel et al, 2018)MINIMUM RECOMMENDEDRECORDING TASKS Connected Speech Tasks– Read a paragraph usingcomfortable pitch andloudness Adults: The RainbowPassage Children: The Trip to the Zoo Pitch Range– Minimum vocal f0 sustained for atleast 1 second– Maximum vocal f0 sustained for atleast 1 second– Determine f0 rangeCan I do instrumental assessment?MEASURES Measures are either obtainedfrom the entire passage orminimum of 5 secondsduration of the passage1.2.3.4.ArSHA 2021Loudness RangeHabitual vocal SPLMean/modal vocal f0Vocal f0 Standard Deviation(SD)Cepstral Peak Prominence(CPP)9
Laryngeal Function Studies:Acoustic MeasuresLow Budget Acoustic Equipment Quantify the auditory‐perceptual parameters ofpitch, loudness, andquality Enable pre‐ and post‐treatment comparisonKeyboard ( 20–X)Pitch Pipe ( 9– 20)Stopwatch ( 2–X)Recording Device(smartphone, cassetterecorder) Elucidate thepathophysiology of vocalfold vibration on voiceproduction(Barsties & De Bodt, 2015; Awan et al., 2016)Affordable Acoustic EquipmentTwo keys to the audio recording Need a High Quality Microphone– Frequency Response:Computer with an audio cardMicrophoneSound Level MeterAudio Interface (mic pre‐ampand A/D converter) Acoustic recording/measurement software Flat (i.e., variation of 2 dB) across the frequency range between the lowest expectedf0 of voice and the highest spectral component of interest (approximately 50–8,000Hz)– Type: Condenser microphone – head mounted Dynamic microphone – tripod or stand– Placement: 4‐5 cm from mouth to microphone Condenser mic should be 45 degrees off‐axis Dynamic mic needs to be directly in front of mouth Environment– Quiet room Ideal if ambient noise is 20 dB SPL lower than recorded voice– Acoustic treatment or considerations (e.g., carpet, sound panels)Examples of two types of micsConnecting your mic to the ‐audio‐interface/Condenser MicrophoneDynamic Microphone 99 220‐ 500You will need: 1501. High quality mic2. Preamp amplifies the mic signalAudiointerface provides3.theAnalog‐to‐digitalpre‐amp, A/D converterAKGC420Frequency ResponseShure SM58Frequency Response transforms audio signal into digitalconverter,and digitalsignal for computerinterface(examples4. Digital interface (e.g. USB,pictured)Firewire, Thuderbolt) 180‐330 communicates with computer5. Computer with sound cardZoom H6 Handy RecorderTASCAM DR‐40X Handheld RecorderArSHA 202110
Sound Level Meter (SLM)Acoustic Analysis Software Type 1 SLM:– Precision grade (most accurate)FREE SOFTWARE Type 2 SLM: Praat (www.praat.org) rfer/)– General grade (less accurate) Use C‐weighting to calibratemeasures of intensity Recommended Reference:– Švec & Granqvist (2018) Tutorial and Guidelines onmeasurement of sound pressure level in voice andspeech, JSLHR, 61: 441‐461.Type 1Type 2Fundamental Frequency (fo) andSound Pressure Level (SPL) Support perceptual correlates– Pitch Fundamental Frequency (fo)– Loudness Sound Pressure Level (SPL)– Quality Cepstral Peak Prominence (CPP) Characterize typical vocal usage duringconversation Characterize maximum performance rangesAmplitude SPLAcoustic Measures Should fo cycles per second 9 cycles/.05s 180 Hertz (Hz)SPL Sound pressure level or acoustic pressure level is alogarithmic measure of sound pressure relative to a reference value– amplitude dimension of the acoustic signal above measured as 62dBMeasures of Voice Quality (Patel et al, 2018) Signal to noise ratiomeasures reflectedlevels of periodic andaperiodic energy in thevoiceWhat is a cepstrum?The Cepstrum The Cepstrum a Fourier transform of the power spectrum of thevoice signal Graphic display of the degree to which the dominant rahmonic canbe identified from the background noise level Crazy terms: spectrum – cepstrum frequency – quefrency filter – lifter Jitter and ShimmerRequire periodicity harmonic – rahmonic Can be obtained from: Sustained vowels Connected speechArSHA 202111
Compare these two CepstraCepstral Peak Prominence (CPP) CPP (circled): Difference inamplitude between the dominantrahmonic (i.e., cepstral peak) andthe cepstrum background (i.e.linear regression line (black)(Hillenbrand et al., 1994, 1996)Typical Voice QualityAberrant Voice Quality13 dB6 dB The CPP measure indicates thedegree of periodic signal in a voice The unit of measure is dB The greater the CPP value, thestronger the periodic signal of thevoice.Recommended measure of voice quality:Cepstral Peak Prominence (CPP) (Patel et al, 2018)CPPs measure: Praat (praat.org) Shown to be a strongpredictor of voicequality (Maryn et al., 2009)– for both vowels andspeech (r .81‐.96)(Awan et al., 2010; Sauder et al,2017) Can be used as atreatment outcomemeasure (Awan & Roy, 2006;Step 1: Load fileStep 2: Analyze Periodicity – to PowerCepstrogramStep 3: Query – Get CPPs2009; Peterson et al., 2013;Ongkasuwan et al, 2019)Maryn & Weenink, 2015; Sauder et al, 2017Case Example 1 – AcousticCPPs measure: Praat (praat.org)Step 2: Analyze Periodicity – toPowerCepstrogram ACOUSTICMEASURESMean/modal F0 (Hz)60‐Hz pitch floor2‐ms time step5 kHz max. frequencyPre‐emphasis from 50 Hz/a/ Avg/i/ Avg292276RainbowPassage314F0 SD (Hz)Mean/modal SPL747621168CPPS in dB15156.5LowestHighestRange641788161217434 (21 ST)Step 3: Query – Get CPPs Subtract tilt before smoothing noTime averaging window .01sQuefrency averaging window .001sPeak search pitch range 60‐330 HzTolerance .05Interpolation “Parabolic”Tilt line quefrency range .001‐0 s (noupper bound)Line type StraightFit method RobustWatts et al, 2017; Brockmann‐Bauser et al,2019; Murton et al, 2020ArSHA 2021SPL RangeF0 Range (Hz) NORMS forFEMALES155-334 Hz ( 25% abovelowest note in the VRP) 32.6 Hz70-80 dB SPL for connectedspeech 14.5 dB for sustainedvowels and 9.3 dB forRainbow Passage 30 dB SPL Range 24 semitonesf0 was at the higher normal rangef0 SD was excessive associated with her noisy voice qualityMean SPL was normal, but SPL range was significantly reducedLow CPP values indicated increased noise in the voiceReduced f0 range and a significantly reduced loudness range (SPL range)12
Laryngeal Function Studies:Aerodynamic AssessmentCase Example 2 – AcousticACOUSTICMEASURES/a/ Avg /i/ AvgAll- VoicelessCAPE-VZoovoiced l fo (Hz)264261210266225251268fo SD (Hz)Mean/modal SPL807773615465776055658NACPPS in dB15169.112.57.99.9NAfo Range (Hz)SPL RangeLowest Highest Range8482001048(29 ST)589537 Efficiency of airstreamconversion into voiceproduction Vocal fold functionduring phonation Respiratory integrity forphonation This child has a normal average and range of fo and SPL range CPPs are not known for children, but had values similar to normal adult valuesAerodynamic Measures at Minimum Average Glottal Air Flow Rate (L/s):– Estimated from the mid‐portion of vowel production Average Subglottal Air Pressure (cmH2O or kPa):– Estimated from interpolated intraoral pressuresduring stop consonant production Mean Vocal SPL and f0:– Aids in the interpretation of air flow and air pressuremeasurementsAffordable Clinical AerodynamicMeasuresAffordable Clinical AerodynamicMeasures Estimate of laryngeal efficiency– S/Z ratio (Eckel & Boone, 1981, Gelfer &Pazera, 2006; Van de Meer et al, 2010; Joshi,2019)– Maximum Phonation Time(MPT)AdultsMalesFemales(Hirano, Koike, & Von Leden, 1968; Bless, 1971;Johnson & Goldfine, 2016)Normal MaxPhonation Durations25‐35 s15‐25 sAffordable Clinical AerodynamicMeasures Vital Capacity Estimate of respiratory drivingpressure for speech– Affordable Spirometer 120.00– Around the house “device” (Hixon etal., 1982)http://www.contecmed.com/index.php?page shop.product details&flypage flypage.tpl&product id 108&category id 21&option com virtuemart&Itemid 604– Ability to sustain 5 cm H2O for 5secondsPhoto taken lArSHA 202113
Affordable Clinical AerodynamicMeasures Average airflow volume calculation– Maximum Phonation Time (MPT)– Vital Capacity (mL)– Phonation Quotient (PQ) Vital Capacity (mL) / MPT (s) Estimated MPT calculation:– MPT(s) VC (mL)/Avg airflow (mL)PhonationQuotientVital CapacityMPTMales4.185 ( .875)31.6 ( 7.94)135 ( 19.3)Females3.019 ( .319)24.6 ( 5.45)125.8 ( 16.4)Additional Respiratory Assessment Observations– Quiet breathing (quiet breathingis 15‐20 breaths per minute)– Respiration‐phonatorycoordination during Sustained phonation Reading task Conversation(Rau & Beckett, 1984; Joshi et al, 2020)Problematic Breathing Patterns Exhaling before speakingShallow inhalationsAudible inhalationsSpeaking too long on one breathPoor phrasingRespiratory effortTension in neck, shoulders, chest, jaw, tongue,lips, etc.SLP Voice Assessment ComponentsAerodynamic MeasuresAdult Case Elevated average airflowvalues– .3‐.4 LPS during sustainedvowels and syllable repetition– .13 ‐ .19 LPS across sustainedvoicing and syllable repetition Elevated intraoral pressures Elevated intraoral pressures– 25 cmH2O (norm is 7‐10cmH2O)– 20 cmH2O (norm is 7‐10cmH2O) MPT 6 seconds s/z ratio 3 MPT 15 seconds s/z ratio 1.7Zraick et al, 2013Weinrich et al, 2013Affordable Laryngeal ImagingSpeech PathologistCPT 92524 Behavioral and qualitative analysis of voiceand resonance (non‐instrumental)Case IntakePatient Self‐ReportCranialNerve Exam(AKA oralperipheralexam)ArSHA ngealImagingPediatric Case Normal average airflowvaluesLaryngologist Determine the presence/ EITHER PARTNER WITH ORabsence of disease/pathologyREFER TO A LARYNGOLOGISTIF YOU DO NOT HAVE Medical diagnosisIMAGING EQUIPMENT Monitor and assess treatmentoutcomes14
Laryngeal ImagingLaryngeal Imaging Contribution Videoendoscopy– Evaluation of gross laryngealand pharyngeal motion andstructure (halogen light) Videostroboscopy– Evaluation of vocal foldvibratory characteristics andstructure (xenon or LEDlight)Overall view of laryngeal structureVocal fold structure and symmetryGlottic configuration during vocal fold closureVocal fold vibratory patternsSupraglottal activityLow‐Tech Viewing of the LarynxIndirect Using iPhoneVideo created from https://www.youtube.com/watch?v 5 RbH3uK640 andhttps://www.youtube.com/watch?v 5g6ew1EhOgYAdvanced Technological LaryngealImagingFlexible ScopeArSHA 2021Scope PlacementLaryngeal Imaging: MethodsRigid Scope15
Rigid Scope Placement90oLaryngeal Imaging: Methods Light Source Differences70o– Videoendoscopy Constant halogen light source– Videostroboscopy Xenon or LED strobe light sourceLaryngeal Imaging: High‐TechEquipmentLaryngeal Imaging: METHODS Scopes attach to a lightsource and camera Camera sends images tothe monitor Images are also recorded(digitized) and saved Audio input (mic) Playback speakersLaryngeal Imaging: Methods Consider clinical tasks– Flexible scope vs. rigid scope Observation Sustained phonation Connected speech– Light source– Patient signs and symptomsLIGHT SOURCE DIFFERENCESVideoendoscopy VideostroboscopyRecommended Laryngeal ImagingProtocolSustained phonation––––Comfortable pitchHigh/low pitchesComfortable loudnessLoud/soft phonation Produce /i–i–i–i/ without breaths inbetween using rapid production ofglottal stops Rest breathing (using rigid or flexibleendoscope) Vegetative tasks and panting Inhalation or “sniff” gesture to test thePCA muscle “/i/–sniff . . . . /i/–sniff” (or inhalation)– Maximum range of motion of vocalfoldsArSHA 202116
Laryngeal Imaging: Stroboscopy Measures of vocal fold vibration require at least 3consecutive videostroboscopic glottal cyclesClosed PhaseOpening PhaseClosing Phase12Laryngeal Imaging: InterpretationEvaluation of gross laryngeal & pharyngeal structure & motion Vocal Fold Edges: Appearance of vocal fold marginsduring abduction Vocal Fold Mobility: Movement of vocal folds towardand away from midline Supraglottic Activity: Degree of compression of thesupraglottic structures during sustained phonation3Slide adapted with permission from Rita Patel; taken from Awan et al. (2015)Laryngeal Imaging: InterpretationEvaluation of Gross Laryngeal and PharyngealMotion and Structure: Vocal Fold Edges:– Smooth & straight, bowed, irregular, or rough– Reported for left and right vocal fold separately Vocal Fold Mobility:– Normal, reduced, or absent– Reported for left and right vocal fold separately Supraglottic Activity:– Predominantly lateral compression,anteroposterior compression, or sphinctericcompression and degree (mild, moderate,severe)Slide adapted with permission from Rita Patel; taken from Awan et al. (2015)Laryngeal Imaging: StroboscopyEvaluation of vocal fold vibratory characteristics duringphonationFigure adapted fromPoburka et al. (2015)1.Regularity: Degree of consistency of one videostroboscopic glottal cyclewith successive cycles2.Amplitude: Extent of lateral movement of vocal fold edges3.Left/Right Phase Symmetry: Degree to which the vocal fold are mirrorimages in the timing of opening, closing, and maximum lateral‐medialexcursion4.Vertical Level: Level difference in vertical plane between the vocal foldduring maximum closed phase of the glottal cycle5.Glottal Closure Pattern: Glottal configuration during maximum closure6.Glottal Closure Duration: Relative portion of each glottal cycle that theglottis is closedSlide adapted with permission from Rita Patel; taken from Awan et al. (2015)Laryngeal Imaging: InterpretationLaryngeal Imaging: Interpretation Regularity:– Regular strobe tracking, intermittent strobetracking, irregular strobe tracking– If the strobe tracking is intermittent or irregular,further estimates/ratings are not valid– Amplitude: 0% to 100% in 25%increments Reported for left and rightvocal fold separatelyFigure adapted from Poburka et al. (2015)RegularIrregularFigure adapted from Poburka et al. (2015)Slide adapted with permission from Rita Patel; taken from Awan et al. (2015)ArSHA 2021Slide adapted with permission from Rita Patel; taken from Awan et al. (2015)17
La
- ASHA member - Member of ASHA's SIG3: Voice and Upper Airway Disorders - ASHA working group member for CAPE‐V and Instrumental Voice Assessment Protocols Speaker Disclosure Julie Barkmeier‐ Kraemer, PhD, CCC‐SLP University of Utah Upon completion of this course, participants will be able to: 1.