Transcription
See discussions, stats, and author profiles for this publication at: Missouri Screening, Brief Intervention, Referral and Treatment: An Analysis ofNational Funding Trends for SBI ServicesTechnical Report · March 2014CITATIONSREADS0154 authors, including:Rita E. AdkinsJoseph George GrailerMissouri Institute of Mental HeathWashington University in St. Louis7 PUBLICATIONS 35 CITATIONS4 PUBLICATIONS 1 CITATIONSEE PROFILESome of the authors of this publication are also working on these related projects:OVCR Online Research Compliance Education Survey View projectMissouri Screening, Brief Intervention and Referral to Tx View projectAll content following this page was uploaded by Joseph George Grailer on 23 December 2015.The user has requested enhancement of the downloaded file.SEE PROFILE
MISSOURI SCREENING, BRIEF INTERVENTION, REFERRAL AND TREATMENT:AN ANALYSIS OF NATIONAL FUNDING TRENDS FOR SBI SERVICESPrepared by theMissouri Institute of Mental HealthRita E. Adkins, MPAJoseph G. Grailer, MFAMandy R. Lay, BABarbara E. Keehn, BSN, RNApril, 2013Revised March, 2014
2Missouri Screening, Brief Intervention, Referral and Treatment:An Analysis of National Funding Trends for SBI ServicesHighlights Due to the current fiscal situation, state revenues are down while expenditures have continuedto rise. As a result, states have been charged with finding new ways to contain escalatinghealthcare costs. Since 50% of patients admitted to trauma centers are under the influence ofalcohol or illicit substances and almost a third of all Emergency Department visits in 2009 werealcohol- and/or drug-related, reducing risky use and the resultant personal and societal costsshould be a top priority. There is a growing body of evidence that Screening, Brief Intervention and Referral to Treatment(SBIRT) is effective in reducing drinking and substance use problems. Based on the outcomesfrom Missouri’s SBIRT (MOSBIRT) program, those individuals receiving brief interventions showreductions in risky use, along with improvements in employment, housing, legal involvementand physical and mental health. Numerous studies have indicated that there is a cost savings of from 3.81 to 5.60 for eachdollar invested in screening for risky use. The most promising approach to sustaining SBIRT services in Missouri and its associatedfinancial, personal, and societal benefits is for Mo HealthNet to fund the State Medicaid codesalready on the state’s fee schedule, thereby allowing for reimbursement of SBI services. There are currently 22 states across the nation with Medicaid (H0049 and H0050) and/or CPTcodes (99408 and 99409) open for SBI reimbursement. Missouri has the Medicaid codes on thefee schedule, but does not have a fee assigned for billing. The average rate for screening isabout 25 per unit, with rates of around 40 per unit for the brief intervention. In addition, some states use the Health and Behavior Assessment/Intervention (HBAI) codes of96150-96155 to bill for SBIRT services. There are 29 states using these codes. Based on experience with the Missouri SBIRT project, the potential costs to activate the SBIcodes for MO HealthNet adults over 18 would be negligible, especially in light of the potentialcost savings. Based on the hypothetical scenario presented, activating the codes would account for anadditional 9 million in Medicaid expenditures, an increase of less than 0.11% of total Medicaidexpenditures in 2010. Of this total, Missouri should only be responsible for 35%, or 3.11 million.The potential benefits from this investment could range from 38 to 56 million, or 1,089% to1,600% in medical and societal costs.
3I.IntroductionIn 2008, the Missouri Division of Alcohol and Drug Abuse reported that the societal costs forsubstance abuse were estimated to be 7 billion annually, with approximately 10% of Missouricitizens needing treatment. The cost to society was reported to average 17,300 for eachsubstance-addicted individual (Missouri Division of Alcohol and Drug Abuse, 2008). That sameyear, the Substance Abuse and Mental Health Services Administration (SAMHSA) awardedfunding to Missouri to provide expanded capacity to identify individuals with risky substanceuse in medical settings and intervene appropriately through a Screening, Brief Intervention andReferral to Treatment (SBIRT) program. Since that time, MOSBIRT, the Missouri SBIRT program,has been successfully implemented at health care facilities in Springfield, Columbia, and St.Louis. In 2012, MOSBIRT was extended to all of Missouri's Health Care Homes (18 FederallyQualified Health Centers, 6 Hospital Affiliated Clinics and one Independent Rural Health Clinic)with over 60 new locations in all. Early identification of risky behaviors is crucial in improvinghealth outcomes and reducing health care and societal expenditures.There is a growing body of evidence about SBIRT’s effectiveness in reducing drinking andsubstance use problems. Those individuals receiving brief interventions show improvements inemployment, housing, legal, physical and emotional health as well as exhibiting decreases intheir substance use. These improvements in social and health domains are supported by theMOSBIRT outcomes (Adkins & Noel, 2011). However, once the federal funding for the MOSBIRTprogram ends on September 30, 2013, there are concerns for maintaining Screening and BriefIntervention (SBI) practices in Missouri. The most promising approach to sustaining SBIRTservices, as well as the associated financial, personal, and societal benefits, is to fund the StateMedicaid codes that allow for reimbursement of SBI services.II.The Personal and Societal Costs of Substance AbuseExcessive alcohol use has been associated with a number of negative health and societyoutcomes. Drinking too much can lead to individual health issues, including cirrhosis of the liver,obesity, certain types of cancer, high blood pressure, stroke, and type 2 diabetes.Figure 1: Physiological Consequences of Risky DrinkingSource: (Cole, Bogenschutz, & Hungerford, 2011)
4The use of alcohol or illicit drugs can also lower inhibitions, leading to riskier behaviors andpotential harm to the user, including homicide, sexual assault and suicide. Risky behaviors as aresult of substance use are also a major factor affecting the incidence of traumatic injury.Almost 50% of patients admitted to trauma centers are under the influence of alcohol or illicitsubstances (Gentilello, Ebel, Wickizer, Salkever, & Rivara, 2005; Gentilello et at., 1999) whilealmost a third of all Emergency Department visits in 2009 were alcohol- and/or drug-related(National Institute on Drug Abuse, 2011). In addition to healthcare costs associated with illness,hospitalizations, and premature deaths, there are also increased costs due to trauma fromvehicular, sporting and work-related accidents.While substance misuse often results in negative health outcomes and resultant increasedhealthcare costs for the individual, there are also associated negative costs to society. In fact, inits 2011 study, the Office of National Drug Control Policy estimated that the societal cost ofsubstance use was 193 billion (United States Department of Justice, 2011). Substance misusealso negatively impacts individuals, families and communities through decreases in workerproductivity and increases in homelessness. The National Institute on Drug Abuse (2011)estimates that local, state and federal government assumes 45% of the cost of substancemisuse while individuals and their families account for 44% of the costs. SBIRT has been shownto be effective in helping to alleviate these personal and societal costs.III.SBIRT is an Effective SolutionCommunity-based screening for health risk behaviors has been recognized as a cost-effectiveway to improve the quality of healthcare in the United States (Babor et al., 2007). As riskysubstance use may lead to injury or negative health consequences, research and clinicalexperience supports SBIRT as an effective intervention for persons at risk for the developmentof substance-related health and social problems. This fact has led the Centers for Medicare andMedicaid Services (CMS) to conclude that the evidence for screening and behavioral counselingto reduce alcohol misuse is reasonable and necessary for the prevention or early detection ofillness or disability (Centers for Medicare and Medicaid Services, 2011). A number of studieshave demonstrated that the return on investment for SBIRT services range from 3.81 to 5.60for each dollar spent (Fleming et al., 2000; Estee, Wickizer, He, Shah, & Mancuso, 2010;Gentilello et al., 2005; Kraemer, 2007) lead the CMS to cover annual screenings and behavioralcounseling services for those screening positively (Centers for Medicare and Medicaid Services,2011). Furthermore, alcohol SBIRT services generate the fourth greatest return on medicalinvestment according to the National Commission on Prevention Priorities, behind daily aspirinuse, childhood immunizations and smoking cessation programs (Partnership for Prevention,2010). A Robert Wood Johnson publication from July, 2012 reported that providing 90 percentof the U.S. population with three clinical preventive services—tobacco-cessation screening andassistance; discussing daily aspirin use; and alcohol screening with brief counseling—wouldeach generate an estimated net savings of more than 1 billion, per year (based on 2006 data).In addition, these three services each would prevent the loss of more than 100,000 years of lifeper year (Crum, 2012).
5IV.What is SBIRT?Many people are unaware that their alcohol and/or other drug use is excessive, but are willingto make behavioral changes once they become aware of the risks to their health. Screening forsubstance use offers a cost-effective way to identify these persons at-risk for substance-relatedproblems.SBIRT is an evidence-based prevention program that systematically screens individuals toidentify, reduce and prevent problematic use of alcohol and drugs (Madras et al., 2009).Typically conducted in medical settings, SBIRT has been shown to be effective in emergencydepartments (Desy & Perhats, 2008), community health centers (Madras et al., 2009) andphysicians’ offices (Fleming et al., 2002), as well as through Employee Assistance Programs(Osilla, Zellmer, Larimer, Neighbors, & Marlatt, 2008; Osilla et al., 2010).Studies have shown that patients who screen positive for unhealthy levels of alcohol and druguse respond more positively to brief interventions than those who drink heavily (Fleming et al.,2002), therefore SBIRT is designed to target those with risky use, focusing on those not yet atthe level of a diagnosable problem. An analysis of over 40 treatment approaches for alcohol usetreatments found that screening and brief intervention was the single most effective treatmentmethod for those not actively seeking treatment (Miller & Wilbourne, 2002). For those withevidence of higher risk levels, there are protocols in place for referral for diagnosis andtreatment.Screening and brief intervention uses a structured set of questions designed to identifyindividuals at risk of substance misuse. Those identified as being at risk engage in a briefdiscussion with a service provider using an evidence-based brief intervention. These briefinterventions (one 5- to 15-minute session or up to six 1-hour sessions, depending on thepatient’s level of risk) are used to increase the patient’s awareness of his/her substance use andits consequences. The provider gives nonjudgmental feedback and suggestions in the form ofuseful information and personal recommendations for change. Using motivational interviewingtechniques, the service provider then attempts to motivate the person to reduce their risky use.ScreeningIncorporated in the normal routine in medical and other communitysettings, screening provides identification of individuals with problemsrelated to alcohol and/or substance use. Those answering positively toprescreen are administered the ASSIST, the full screening instrument.Brief EducationBrief CoachingFollowing a screening result indicatingFollowing a screening result of moderate tomoderate risk, a brief 5-15 minutehigh risk, a brief coaching is provided. Thisintervention is provided, involvingalso involves motivational discussion andmotivational discussion focused onclient empowerment, but is moreraising individuals’ awareness of theircomprehensive. It includes assessment,substance use and its consequences, andeducation, problem solving, copingmotivating them toward behavioralmechanisms & building a supportive socialchange.environment.Source: (Substance Abuse and Mental Health Services Administration, 2008)Referral to TreatmentFollowing a screening result of possibledependence, a referral to treatment isprovided. This is a proactive process thatfacilitates access to care for thoseindividuals requiring more extensivetreatment than SBIRT provides andensures access to appropriate level of carefor all screened.
6V.SBIRT in MissouriMOSBIRT, Missouri's SBIRT project, emphasizes prevention, early detection, and earlyintervention of substance use, and builds upon the work of previous grantees by incorporatingthe evidence-based practices into a tablet computer. Using this system (MOSBox), the healthcoaches at the original MOSBIRT medical sites conduct face-to-face screenings of all individualsentering the medical facilities for signs of the misuse of prescription and illicit drugs, alcohol,and tobacco. All individuals are initially screened for risky behaviors with one to four questions.A web-based system, eSBIRT, has also recently been developed, and is used by the BehavioralHealth Consultants with Health Home patients at the Federally Qualified Health Centers. AllHealth Home patients are screened annually.MOSBIRT Screening(N 80,887) Thru 12/31/2012Low RiskModerate Risk(N 4,355, 5.4%)Moderate/HighRisk (N 1,013, 1.2%)No FurtherInterventionBrief EducationBrief Coaching(N 74,162, 91.7%)Severe Risk(N 1,357, 1.7%)Referred toTreatmentThose who score positively from the prescreen questions (generally less than 30%) areadministered an additional screening, the World Health Organization’s Alcohol, Smoking andSubstance Involvement Screening Test (ASSIST). Individuals who are identified as being at-risk(8-9%) in the second-level screen are provided a personalized feedback report describing theirindividual risks, comparing their substance use with peers, and providing specific behavioralchange recommendations based on their readiness to change (see appendix 1 for an exampleof the personalized feedback report generated by MOSBox and eSBIRT electronic systemsdesigned to aid in the SBI process). This report is used by MOSBIRT’s trained staff to guideservice delivery.Most of the at-risk individuals will exhibit moderate risk scores and are offered a 5-15 minuteintervention using Motivational Interviewing (Carroll et al., 2006; Vasilaki, Hosier, & Cox, 2006).Those with higher levels of risk can get up to six sessions of behavioral coaching, or for thosewho already show symptoms of abuse or dependence, the staff will employ an evidence-basedwarm hand-off approach. This method links patients with potential substance abuse problemswith specialists, using face-to-face or phone transfer to get them into a specialized substanceabuse treatment program. As of December, 2012, over 80,000 patients have been screenedacross the state of Missouri, with nearly 7,000 individuals receiving interventional services.A detailed description of the MOSBIRT process can be found in Appendix II.
7VI.MOSBIRT OutcomesMOSBIRT is designed as a universal screening process, meaning that all patients over 18 arescreened, provided their health is not compromised to the point of unfeasibility. A detaileddescription of the MOSBIRT process can be found in Appendix II.National Outcome Measures (NOMS): Intake and 6-Month Follow-Up of ThoseScreening PositiveTo measure the effectiveness of the MOSBIRT project, a random sample of patients receiving anintervention is administered a 6-month follow-up interview. The outcomes chart the progressof patients for whom both intake and 6-month follow-up data were available. As of December31, 2012, the follow-up rate for 6-month patients was 75.3%. The progress on the NOMs for thepatients receiving follow-up interviews (N 176) follows. Please note that the number ofpatients by NOM varies, as those receiving Brief Education are only asked the substance usequestions.Abstinence — The percentage of patients who reported that they did NOT use increased511.1% from intake to 6 month follow-up (N 176). Number of days of substance use in thepast 30 days at intake and 6-month follow-up show declines as follows:Crime and Criminal Justice —The percentage of patients whoreported NO arrests within the past30 days increased by 11.3% fromintake to 6-month follow-up (N 61).Employment/Education — Thepercentage of patients reportingthey were currently employed orattending school increased by 33.3%from intake to 6-month follow-up(N 43).Health/Behavioral/Social Consequences — The percentage of patients reporting noalcohol or illegal drug related health, behavioral or social consequences increased by 53.1%from intake to follow-up (N 65).Stability in Housing — The percentage of patients reporting that they had a permanentplace to live in the community did not change from intake to follow-up (N 64)The successes demonstrated to date with MOSBIRT services would further reduce societal costsby proactively addressing risky behaviors before they become full blown addictions. Earlydetection of risk behaviors that negatively impact health is not only important for the quality oflife issues of Missouri’s citizens, it is also an important component in controlling for bothpersonal and societal health care costs.
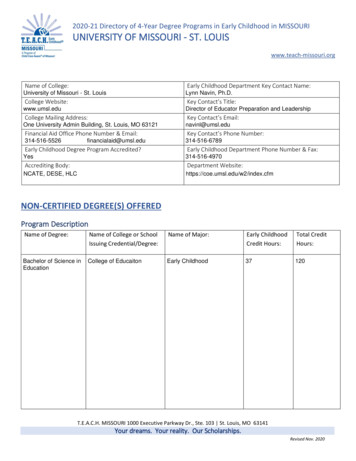
8VII. Study of Codes Nationwidea)BackgroundMedical procedures are billed using codes, either through the Healthcare Common ProcedureCoding System (HCPCS) or the Common Procedure and Terminology (CPT) code sets. The HCPCScodes consist of Level 1 (CPT codes) and Level II (State codes). The American MedicalAssociation (AMA) maintains the CPT coding system, while the Centers for Medicare andMedicaid Services (CMS) maintains the Level II State codes. These Level II codes are nationallystandardized and are 5-digit, beginning with a letter followed by 4 digits. As of January, 2007,CMS designated HCPCS codes H0049 for substance use screening and H0050 for Briefinterventions. The following year, the AMA approved several billing codes, including 99408 for15 minutes of SBI and 99409 for 30 minutes of SBI Substance Abuse and Mental Health ServicesAdministration, 2012). While a billing amount is suggested by the CMS, states have the abilityto determine its own billing amounts. Though Missouri currently has the Medicaid codes on thefee schedule, a dollar amount allowing providers to bill for SBI services has not been assigned tothe codes. Without these billing amounts, practitioners do not have the ability to getreimbursed for SBI services. Without reimbursement, there is no incentive to conduct theseservices, despite the known personal and societal benefits to doing so.b)PurposeIn an effort to present MO HealthNet with a rationale for supporting SBIRT services, the authorsexamined the states that have funded the billing codes in an attempt to determine the fiscaland societal costs and benefits encountered.c)MethodsA review of the literature revealed that while a number of states (including Missouri) have theSBIRT codes on its Medicaid fee schedule, they do not have a billing amount assigned to thecodes (open for reimbursement) (Fussell, Rieckmann, & Quick, 2011; Anderson & Bhang, 2009).We contacted other states that had received SAMHSA funding for SBIRT services to gain abetter understanding for how to approach getting the SBI and HBAI codes funded, and, basedon their experience, we elected to employ qualitative methods. With input from Dr. Joe Parks,Director of the Missouri Institute of Mental Health, we developed a questionnaire designed togather information from the states of their current status of the SBI and HBAI codes on theirMedicaid fee schedules (see Appendix III).In August, 2012, the Director of State Medicaid for Missouri, Dr. Ian McCaslin, sent a request tothe National Association of Medicaid Directors to complete this questionnaire. We receivedinformation from 6 states and DC, indicating that 5 states had the codes listed on their stateMedicaid fee schedule, with 1 state (CO) and DC reporting the SBI codes with a billing amountassigned, and 2 states (CA and OK) and DC having a billing amount assigned to their HBAI codeslisted on their Medicaid fee schedule.
9To supplement the minimal responses received, we surveyed state Medicaid agencies bytelephone and email, with little success. Fussell, Riechmann, and Quick (2011) found that websearches corroborated information reported by phone interviews, validating the Medicaid feeschedules posted on the web. We therefore opted to conduct web searches for all stateMedicaid fee schedules. These web investigations were conducted from September, 2012 toDecember, 2012, with all states having the public information posted on their websites.d)Results of Code AnalysisScreening, Brief Intervention (SBI) Codes:Currently, reimbursement for SBIRT screening is not provided consistently. There areopportunities for expanding SBI as the Affordable Care Act (ACA) will require that all employerand Medicare plans cover prevention services that the US Prevention Services Task Force(USPSTF) has concluded are effective (Brolin et al., 2012). Alcohol screening and briefintervention are on the list of effective clinical prevention treatments.The AMA and CMS guideline for healthcare providers who conduct Screening and BriefIntervention follows, with billing codes that can be used to ensure that SBI services arereimbursed odeDescriptionCPT99408Alcohol and/or substance abuse structured screening and brief interventionservices; 15 to 30 minutes 33.41CPT99409Alcohol and/or substance abuse structured screening and brief interventionservices; greater than 30 minutes 65.51H0049Alcohol and/or drug screening 24.00H0050Alcohol and/or drug service, brief intervention, per 15 minutes 48.00G0396Alcohol and/or substance abuse structured screening and brief interventionservices; 15 to 30 minutes 29.42G0397Alcohol and/or substance abuse structured screening and brief interventionservices; greater than 30 minutes 57.69Source: (Substance Abuse and Mental Health Administration, 2012)An analysis of the states that have the SBI codes on the Medicaid fee schedule (H0049 andH0050) and the commercial CPT codes (99408 and 99409) indicate a range of fees allocated tothe SBI codes, as follows:
10Survey of Medicaid Reimbursement Rates for SBI (n 51, All states and DC)SBI CodeH0049 (Screening)H0050 (Brief Intervention)# of States w/Code on Fee Schedules# of States w/Code# of States w/Code FundedBut Not FundedNot on Fee Schedule7 (Range 14.49- 30.24, Avg 23.30)13318 (Range 19.50- 64.26, Avg 35.42)123199408 (15 min SBI)17 (Range 14.07- 54.25, Avg 27.85)142099409 (30 Min SBI)17 (Range 27.60- 105.90, Avg 55.10)1420Missouri has all SBI codes on the Medicaid fee schedule, but does not have a fee assigned to allow for billing of services.Some State Medicaid Agencies (SMAs) bundle all services into one rate, a prospective paymentsystem (PPS). One state (DE) listed minimal rates of less than 2, so were excluded from theaverage rate list for the 99408 and 99409 codes. The state of Tennessee contracts with outsideproviders that maintain their own fee schedule, so they were counted as having the codesfunded, but the prices were not included in the averages. In some states, there are differentrates based on facility/non-facility charges, with minimal differences of 30-60 cents betweenthe 2 charges. In these cases, an average of the 2 charges was used in the calculations of themean charges.Billing for SBIRTThere are also state differences in the level of provider that is eligible to bill for SBI. However,only a few states actually list the provider able to bill for the SBI codes on its Medicaid feeschedule. For instance, in North Carolina the billing rates for the SBI code of 99408 is listed as 30.73 for a non-facility Nurse Midwife and 29.46 for a Facility Physician, Physician Assistant,& Nurse Practitioner, while New Jersey lists a rate of 15.21 for a “specialist” and 12.93 for a“non-specialist”. Alaska stipulates a 58.65 for a physician and 49.85 for a nurse practitioner.While there is no provider stipulated for the remainder of the states with a billing amountlisted, The American College of Surgeons Committee on Trauma (COT) states that“Brief intervention does not have to be administered by a state-certifiedsubstance abuse counselor or by other clinicians with advanced training insubstance abuse treatment. After relatively little training, brief intervention canbe performed by anyone capable of showing respect and concern for injuredpatients. In addition to mental health or substance abuse counselors, the COTbelieves that there are multiple people in each trauma center who can meetthese criteria, including surgeons and other MDs, psychologists, physicianassistants, nurses, social workers and spiritual care workers.” (Substance Abuseand Mental Health Services Administration, 2007)Babor, et al. (2006) found that using paraprofessional staff to deliver brief interventions hasbeen shown to be as effective as those delivered by licensed practitioners. The averageincremental costs of the intervention in their study was 4.16 per patient using licensedpractitioners compared to 2.82 using mid-level specialists.
11While the New York State Department of Health reimburses for SBIRT services provided byphysicians, nurse practitioners, nurse midwives and psychologists with 4 hours of training inSBIRT skills, paraprofessionals with minimum hours of SBIRT training can also bill under theprovider number of a licensed provider, such as a hospital or clinic. The following table lists theprovider types eligible to perform SBIRT and bill under a licensed provider/facility:Provider TypePhysician AssistantsRegistered NursesLicensed Practical NursesLicensed Master Social Worker (LMSW) or Licensed Clinical Social Worker (LCSW)Licensed Mental Health CounselorsLicensed Marriage and Family TherapistCertified School CounselorCertified Rehabilitation CounselorOASAS-credentialed professionals including Credentialed Alcoholism and SubstanceAbuse Counselors (CASACs), Credentialed Prevention Professionals (CPPs) andCredentialed Problem Gambling CounselorsHealth Educators and unlicensed individuals (may only provide SBIRT services underthe supervision of a licensed health care professional, following consistent protocols)RequiredTraining/Certification4 hours4 hours, unless qualifiedas a CARN4 hours4 hours4 hours4 hours4 hours4 hours4 hours12 hoursSource: (New York State Department of Health, 2011)The MOSBIRT project has produced a document that details the training requirements for eachstep of the SBIRT process. Training for a licensed or unlicensed staff to administer the prescreenrequires 2 hours of training, 6 hours of training for full screening and other assessments, and 10hours to screen and provide a brief intervention. The document detailing the Clinical Definitionsof MOSBIRT services can be found in Appendix IV.Health and Behavior Assessment/Intervention (HBAI) Codes:Some states use Health and Behavior Assessment/Interventions codes to identify psychologicaland behavioral factors important to the prevention, treatment and management of physicalhealth problems. These codes are used for services performed by nonphysician health careprofessionals to assess a patient’s behavior and emotional state that are important to thetreatment and management of physical health problems. There are five reimbursement codesfor health and behavior assessment and intervention that are sometimes used for SBI services.The health and behavior assessment and intervention codes follow (American MedicalAssociation, 2006):96151 – An assessment of the patient to evaluate the patient’s condition and determine theneed for further treatment. A re-assessment may be performed by a clinician other than theone who conducted the patient’s initial assessment.96152 – The intervention service provided to an individual to modify the psychological,behavioral, cognitive, and social factors affecting the patient’s physical health and wellbeing. Examples include increasing the patient’s awareness about his or her disease and
12using cognitive and behavioral approaches to initiate physician prescribed diet and exerciseregimens.96153 – The intervention service provided to a group. An example is a smoking cessationprogram that includes educational information, cognitive-behavioral treatment and socialsupport. Group sessions typically last for 90 minutes and involve 8 to 10 patients.96154 – The intervention service provided to a family with the patient present. Forexample, a psychologist could use relaxation techniques with both a diabetic child and hisor her parents to reduce the child’s fear of receiving injections and the parents’ tensionwhen administering the injections.96155 – The intervention service provided to a family without the patient present. Anexample would be working with parents and siblings to shape the diabetic child’s behavior,such as praising successful diabetes management behaviors and ignoring disruptive tactics.An analysis of the states that have the HBAI codes on the Medicaid fee schedule (96151-96155)indicate that states have activated these codes more often than the SBI codes. The range offees allocat
Barbara E. Keehn, BSN, RN . April, 2013 . Revised March, 2014 MISSOURI SCREENING, BRIEF INTERVENTION, REFERRAL AND TREATME NT: AN ANALYSIS OF NATIONAL FUNDING TRENDS FOR S BI SERVICES . 2 Missouri Screening, Brief Intervention, Referral and Treatment: