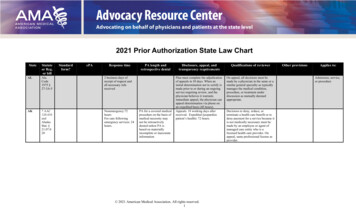
Transcription
2021 Prior Authorization State Law ChartStateALAKStatuteor Reg.or billStandardform?ePAResponse timeAla.Code1975 §27-3A-52 business days ofreceipt of request andall necessary inforeceived7 AAC120.410andAlaskaStat. §21.07.020Nonemergency:72hoursFor care followingemergency services: 24hours.PA length andretrospective denialPA for a covered medicalprocedure on the basis ofmedical necessity maynot be retroactivelydenied unless PA isbased on materiallyincomplete or inaccurateinformationDisclosure, appeal, andtransparency requirementsQualifications of reviewerPlan must complete the adjudicationof appeals in 30 days. When aninitial determination not to certify ismade prior to or during an ongoingservice requiring review, and thephysician believes it warrantsimmediate appeal, the physician canappeal determination via phone onan expedited basis (48 hours).Appeals: 18 working days afterreceived. Expedited (jeopardizepatient’s health): 72 hours.On appeal, all decisions must bemade by a physician in the same or asimilar general specialty as typicallymanages the medical condition,procedure, or treatment underdiscussion as mutually deemedappropriate. 2021 American Medical Association. All rights reserved.1Decisions to deny, reduce, orterminate a health care benefit or todeny payment for a service because itis not medically necessary must bemade by an employee or agent ofmanaged care entity who is alicensed health care provider. Onappeal, same professional license asprovider.Other provisionsApplies to:Admission, service,or procedure
StateARStatuteor Reg.or billAR Code§ 23-991107(2017)Standardform?YesePAResponse timePA length andretrospective denialNonurgent: 2 businessdays of obtaining allnecessary infoUrgent: 1 business dayEmergency: a minimumof 24 hours followingprovision of emergencycare for patient orprovider to notify planof admission orprovision of care(2) If occurs on aholiday or weekend,plan cannot requirenotification until thenext business dayCannot rescind, limit orcondition based onmedical necessity unlessprovider is notified 3business days before thescheduled date.If patient receivesemergency care thatrequires an immediatepost-evaluation or poststabilization service, aplan must make anauthorization within 60minutes of receiving arequest.Disclosure, appeal, andtransparency requirementsPlans must disclose all PArequirements and restrictions,including any written clinicalcriteria, in a publicly accessiblemanner on its website. (Ifproprietary, can be available viasecured link.)Cannot implement new/amendedrequirements before providingwritten 60-day notice.Statistics must be availableregarding prior authorizationapprovals and denials on plan’swebsite in a readily accessibleformat. The statistics mustcategorize approvals and denials byphysician specialty; medication ordiagnostic test or procedure; medicalindication offered as justification forthe prior authorization request; andreason for denial.An adverse determination must bebased on medical necessity orappropriateness of the health careservices and on written clinicalcriteria.Qualifications of reviewerAn adverse PA determination shallbe made by a qualified health careprofessionalOther provisions"Medical necessity"includes "medicalappropriateness","primary coveragecriteria", and any otherterminology used by aplan that refers to a"primary coveragecriteria", and any otherterminology used by aplan that refers to adetermination that isbased in whole/in part onclinical justification for aservice.The determination by aplan of medical necessityof an emergency servicecannot be based onwhether the service wasprovided by an out-ofnetwork provider.If a subscriber's coveredprescription painmedication requires aprior authorization, thenthe prior authorizationshall not be denied if thesubscriber has a terminalillness.A PA decision shallinclude a determinationas to, whether, or not theindividual is covered bya health benefit plan andeligible to receive therequested service. 2021 American Medical Association. All rights reserved.2Applies to:Includes steptherapy
StateARCont.Statuteor Reg.or billAZA.R.S.§202803CA28 CCR§1300.67.241Standardform?Utilize andaccept onlythe PA form(Form No.61-211).Acceptthrough anyreasonablemeans- paper,electronic,phone, webportal, oranothermutuallyagreeablemethod.Notices toproviderdelivered inePAResponse timeFor care provided afterinitial screeningexamination andimmediately necessarystabilizing treatment,prior auth is grantedunless denied ordirection of thepatient’s care isinitiated by the planw/in a reasonableperiod of time after theplan receives therequest2 business days forexigent circumstancesand 72 hours urgent ofreceipt of requestPA length andretrospective denialDisclosure, appeal, andtransparency requirementsQualifications of reviewerOther provisionsA provider may submita benefit inquiry to aplan for a service notyet provided todetermine whether theservice meetsmedical necessity andall other requirementsfor payment.Payer cannot request infothat does not apply to themedical condition atissue for the purposes ofdetermining whether toapprove or deny a PArequest.Plan cannot rescind ormodify the authorizationafter the provider rendersthe authorized care ingood faith and pursuantto the authorization.Plan must have written policies andprocedures establishing the processby which the plan prospectively,retrospectively, or concurrentlyreviews and approves, modifies,delays, or denies, based in whole orin part on medical necessity,requests by providers of health careservices for plan enrollees. Thesepolicies and procedures shall ensurethat decisions based on the medicalservices are consistent with criteriaor guidelines that are supported byclinical principles and processes.These policies and procedures, and adescription of the process by whichthe plan reviews and approves,modifies, necessity of proposedhealth care delays, or deniesrequests by providers to, 2021 American Medical Association. All rights reserved.3Plan must employ or designate amedical director who holds anunrestricted license to practicemedicine in this state issued pursuantto Section 2050 of the Business andProfessions Code or pursuant to theOsteopathic Act. The medicaldirector or clinical director shallensure that the process by which theplan reviews and approves, modifies,or denies, based in whole or in parton medical necessity, requests byproviders prior to, retrospectively, orconcurrent with the provision ofhealth care services to enrollees,complies with the requirements ofthis section.Applies to:Emergency caredrugs
StateCACont.COStatuteor Reg.or billStandardform?ePAResponse timesame manneror .S.10-16113YesElectronicallymeans when theprovider submitsrequest througha secure, webbased internetportal. Does notinclude e-mailFor Rx: 2 business days(ePAs); 3 business days– non-urgent (oral, fax,email); 1 business day –urgent (oral, fax, email)For medical services:15 days non-urgent,Urgent 72 hours.For concurrent reviewurgent care requestsinvolving a request bythe patient to extend thecourse of treatmentbeyond the initialperiod of time or thenumber of treatmentsauthorized, if therequest is made at least24 hours prior to theexpiration of theauthorized period oftime or authorizednumber of treatments,the plan shall make adetermination withPA length andretrospective denialDisclosure, appeal, andtransparency requirementsQualifications of reviewernecessity of proposed health caredelays, or denies requests byproviders prior to, retrospectively, orconcurrent with the provision ofhealth care services to enrollees,shall be filed with the director forreview and approval, and shall bedisclosed by the plan to providersand enrollees upon request, and bythe plan to the public upon request.No individual, other than a licensedphysician or a licensed health careprofessional who is competent toevaluate the specific clinical issuesinvolved in the health care servicesrequested by the provider, may deny,or modify requests for authorizationof health care services for an enrolleefor reasons of medical necessity.The decision of the physician orother health care professional shallbe communicated to the provider andthe enrollee pursuant to subdivision(h).Notice of right to appeal must begiven to patient when PA is denied.Must disclose list of drugs thatrequire PA, written clinical criteriaand criteria for reauth of previouslyapproved drug after PA periodexpired.Require evidence-based guidelines.For prospective reviewdetermination, carrier must giveprovider opportunity to request peerto-peer conversation regardingadverse determination by thereviewer making determination.Request may be made orally or inwriting. Peer-to-peer must occurw/in 5 calendar days of receipt ofrequest and be conducted b/wprovider and reviewer who made thedetermination or a clinical peerdesignated by reviewer if reviewercan’t be available w/in 5 calendardays. 2021 American Medical Association. All rights reserved.4Other provisionsApplies to:
StateCOCont.Statuteor Reg.or billStandardform?ePAResponse timePA length andretrospective denialrespect to the requestand notify the patientand provider within 24hours.Disclosure, appeal, andtransparency requirementsFirst level – plan has 30 days.Review must be evaluated by aphysician who consults with anappropriate clinical peer unlessreviewing physician is a clinicalpeer. The physician and clinicalpeer(s) cannot have been involved ininitial determination but person thathas involved w/denial may answerquestions.Reviewer must consider allcomments, documents, records, andother info regarding requestsubmitted w/o regard to whether theinfo was submitted or considered inmaking the initial adversedetermination.CTDEHB 381(2016)Yes, NCDPDstandard for ePA(no standard formedical servicesePA)Drugs: 2 business daysfrom clean PAMedical services notthrough ePA, 8 businessdays; ePA: 5 businessdaysPlan cannot revoke,limit, condition or restricta PA on ground ofmedical necessity afterdate the health careprovider received the PA.A proper notification ofpolicy changes validlydelivered may void a PAif received after PA butbefore delivery of theservice. 2021 American Medical Association. All rights reserved.5Qualifications of reviewerAll written adverse determinationsmust be signed by a licensedphysician familiar with standards ofcare in Colorado. In the case ofwritten denials of requests forcovered benefits for dental care, alicensed dentist familiar withstandards of care in Colorado maysign the written denial.Other provisionsCan prospectivelyrequest peer-to-peerreview.Plan must establish areview process at whichpatient has right toappear in person or byphone at review meetingbefore a health careprofessional(reviewer) or, if offeredby the plan, a reviewpanel of health careprofessionals, selected bythe carrier. The adversedetermination, or w/respect to a voluntarysecond level review of afirst level reviewdecision, the denial mustbe reviewed by a healthcare professional or, ifoffered by the carrier, areview panel of healthcare professionals, whohave appropriateexpertise in relation tothe case presented by thecovered person.Applies to:Drugs/medicalservices
StateDECont.DCFLStatuteor Reg.or billStandardform?ePAResponse timePA length andretrospective denialA PA for a health careservice shall be valid fora period of time that isreasonable andcustomary for thespecific service, but noless than 60 days fromthe date the health careprovider receives the PA,subject to confirmationofcontinued coverage andeligibility and to policychanges validlydelivered.Disclosure, appeal, andtransparency requirements60-day notice of new PArequirements.Must make any current PArequirements readily accessible onwebsite and in written or electronicform upon request. Requirementsmust be described in detail and inclear, easily understandablelanguage.Clinical criteria must be described inlanguage easily understandable by aprovider practicing in the sameclinical area.Plans must report statistics on PAapprovals, denials, and appeals tothe Delaware Health InformationNetwork at least twice annually.Department may also request thisdata at any time.The statistics shall include: (1) Fordenials, aggregated reasons fordenials; (2) For appeals: a.Practitioner specialty; b.Medication, diagnostic test, ordiagnostic procedure; c. Indicationoffered; d. Reason for underlyingdenial; and e. Number of denialsoverturned upon appeal.Ch.2016224(627.42392)and Ch.16 –222A plan thatdoes not useePA must usethe standardPA formapproved bythe FSC 2021 American Medical Association. All rights reserved.6Qualifications of reviewerOther provisionsApplies to:Drugs and medicalservices (not allprovisions apply toboth.)Not Medicaid
StateGAHIStatuteor Reg.or billGACodeAnn.33-64-8Standardform?ePAResponse timePA length andretrospective denialApproval of coveredservice cannot berescinded after theservice is provided,except forfraud/misrep/nonpayment of premium,exhaustion of benefits, ormember not enrolled atthe time service wasprovided.Approval of medicalexception request goodfor one year or end ofcoverage.Other provisionsApplies to:General formused by someinsurers.Title 41,Ch. 39(413930)2 business days aftercomplete membermedical information isprovided to plan, unlessexceptionalcircumstances warrant alonger period.IL215ILCS13472 hours from receipt ofpaper or electronic priorauthorization form mustapprove or deny; 24hours expedited.SB 73(2017)HR1143(2018)Qualifications of reviewerYes, NCPDPstandardIDINDisclosure, appeal, andtransparency requirementsYesNCPDPstandard.Required of planand physicians.Exemptionsunder certaincircumstancesand provider touse standardform(12/31/2019)Urgent – 72 hours fordetermination afterreceiving request.Nonurgent – 7 businessdays for determinationafter request. Ifincomplete request,must respond w/in timeperiod. (For ePAimmediate electronicreceipt required.)After authorization,cannot retroactively denyexcept if false orincorrect info wasprovided or noncoverageon day of service. Cannotdeny claims forunanticipated medicalservice provided duringanother authorizedmedical service basedsolely on lack of priorauth.15 days for appeal decisions.Denials can be appealed andreviewed by external independentreview.Must provide, upon request, precertification and other utilizationreview procedures and requirements.List of prior auth requirements byCPT code on website or portal,including specific information that aprovider must submit for request tobe completed. Plans must discloseany new prior auth requirements 45days before implemented (can beaccomplished by postedconspicuously on plan’s website). 2021 American Medical Association. All rights reserved.7As provided in the IL Health CarrierExternal Review ActMedical exceptionprocess includes steptherapy exceptionsprocess – 72 hours for adecision.DrugDrugs
StateIAKSKYStatuteor Reg.or bill191 IAC79KY RevStat §217.211SB 542019Standardform?YesePAResponse timeCommissionercan considerNCPDPstandards.72 hours for urgentclaims; 5 calendar daysfor non-urgent claims;24 hours expeditedIf a request for a PAis incomplete oradditional info isrequired, the plan mayrequest additional infow/in the applicable timeperiods. Once the infois submitted, theapplicable time-periodbegins again.Payer must assign PArequest a uniqueelectronic ID number totrack request.Insurers mustdevelop,coordinate, oradopt a processforelectronicallyrequesting andtransmitting PAfor drugs thatmeets the mostrecent NCPDPSCRIPTstandard for ePAadopted byHHS. Fax,proprietarypayer portals,electronic formsare notelectronictransmission.Urgent: 24 hours aftergetting all necessaryinfo.Nonurgent: 5 days aftergetting all necessaryinfo.Necessary info islimited to the results ofany face-to-face clinicalevaluation; any secondopinion that may berequired; and other infodetermined by thedepartment to benecessary to making autilization reviewdetermination.PA length andretrospective denialDisclosure, appeal, andtransparency requirementsQualifications of reviewerOther provisionsPayers must make the followingavailable/accessible on websites:a. PA requirements and restrictions,including list of drugs that requirePA. b. Clinical criteria that areeasily understandable to health careproviders, including clinical criteriafor reauthorization of a previouslyapproved drug after the PA periodhas expired. c. Standards forsubmitting and considering requests,including evidence-basedguidelines, when possible, formaking PA determinations.PA for a drug for apatient with a conditionthat requires ongoingmedication therapy, andthe provider continues toprescribe the drug, thePA is valid for the lesserof 1 year or the last dayof coverage under theplan year. Changes indoses do not require newPA. This provision doesnot include medicationsfor a non-maintenancecondition; that have atypical treatment period 12 months; where thereis evidence that does notsupport 2-monthapproval; or opioidanalgesics orbenzodiazepines.Insurers must make writtenprocedures for determining whethera requested service, treatment, drug,or device is covered; makingutilization review determinations;and notifying patients and providersof its determinations readilyavailable on website to coveredpersons, authorized persons, andproviders.Insurers must maintain info onpublicly accessible website aboutlist of services/codes for which PAis required including when required(effective dates); date therequirements were listed; and dataPA is removed if appliable. Also,must include services where PA isperformed by contracted entity.(Cannot deny claim if PA not ineffect on data of services on claim) 2021 American Medical Association. All rights reserved.8Applies to:DrugsAny contract entered into on or afterthe effective date of for the provisionof utilization review services, onlylicensed physicians, who are of thesame or similar specialty andsubspecialty, when possible, as theordering provider, can make autilization review decision to deny,reduce, limit, or terminate a benefitor to deny, or reduce payment for aservice because that service is notmedically necessary, experimental,or investigational.Medically necessaryhealth care servicesdefinition: Health careservices that a providerwould render to a patientfor the purpose ofpreventing, diagnosing,or treating an illness,injury, disease, or itssymptoms in a mannerthat is: (a) In accordancew/ generally acceptedstandards of medicalpractice; and (b)Clinically appropriate interms of type, frequency,extent, and duration.Cannot require PA forbirths or inception ofneonatal intensive careservices and notificationcannot be required as acondition of payment.
StateKYCont.LAMEStatuteor Reg.or R.S.22:1139Chapter273 PLS.P.218L.D.7052019Yes, must s.ePAResponse timeThe insurer's failure tomake a determinationand provide writtennotice w/in the timeframes will be deemedto be a PA for theservices or benefitssubject to the review.Must accept/respond to PArequests throughsecure electronictransmissionusing standardsadopted byNCPDP forelectronicprescribingtransactions fax, proprietarypayer portal, orvia electronicform is notelectronictransmissionPA length andretrospective denialDisclosure, appeal, andtransparency requirementsInsurer (or contacted entity), beavailable to conduct utilizationreview during normal business hoursand extended hours on Monday andFriday through 6:00 p.m., includingfederal holidays.Nonemergency: Lesserof 72 hours or 2business days (notifyprovider and patient).If does not respond w/If additionalinformation needed,lesser of 72 hours or 2business days fromreceiving info. Ifoutside consultationneeded, 72 hours or 2business days fromplan’s initial response. 2021 American Medical Association. All rights reserved.9Qualifications of reviewerOther provisionsUnless otherwisespecified by theprovider's contract, aninsurer cannot deem asincidental or denysupplies that areroutinely used as part ofa procedure when: (a)associated procedure hasbeen preauthorized; or(b) PA for the procedureis not required.Applies to:
StateMDStatuteor Reg.or billMDCodeAnn.19108.2Standardform?ePAOnlineprocess foraccepting PAelectronicallyPlans mustestablish anonline PAsystem for drugs& for steptherapyResponse timeMAMGL C.1760,25YesMust beavailableelectronically2 business days afterreceiving a completedPA request from aproviderMISection500.2212c oftheinsurance codeFor Rx - DOIappoint ists,hospitals,others indevelopingPA standardmethodologyWorkgroup shallconsidernationalstandards forePA developedby NCPDP15 days for nonurgent,72 hours for expeditedto approve, deny orrequest more info. Aftersubmission of info, timerequirements startagain. Prescriber mustsubmit additional infow/in 21 days (5 days forurgent)PA length andretrospective denialDisclosure, appeal, andtransparency requirementsReal time for ePA(pharma) that meetscriteria, and no additionalinfo is needed.1 business day for nonurgent drug;2 business days nonurgent services(electronically)Online access for providers to healthcare services requiring PA and keycriteria for making a determination.Unique electronicidentifier that providercan use to track PA. 2021 American Medical Association. All rights reserved.10Qualifications of reviewerOther provisionsStep-therapy overrideprocessApplies to:PA and Step therapyRx, provider officevisits, imaging/diagnostic testing,lab testing and anyother health careservice
StateMNStatuteor Reg.or billM.S.A.§62M.05;M.S.A.§62M.06M.S.A.§62M.07tSF 32042019Standardform?YesSec. 4. MNStatutes 2018,section62M.04,subdivision 3limitedePAYes, NCPDPstandardmandated forprescribers andplans.(If PA for healthcare service isrequired, mustallow providersto submitrequests bytelephone, fax,or voice mail orthrough anelectronicmechanism 24hours a day,seven days aweek)Response timePA length andretrospective denialDisclosure, appeal, andtransparency requirementsNonurgent: 5 businessdays after all inforeasonably necessary tomake decision isprovided (2022) andmust provide “audittrail” of notification.When patient changesplans, PA must be goodfor 60 days. To obtaincoverage for this 60-dayperiod, provider/patientmust submitdocumentation of theprevious PA to new plan.Upon request, provide the provideror patient w/ criteria used todetermine necessity,appropriateness, and efficacy of theservice and identify the database,professional treatment parameter orother basis for the criteria.Expediteddetermination requiredif provider believeswarranted.Determinationexpeditiously asmedical conditionrequires, but no laterthan 48 hrs and mustinclude at least onebusiness day after theinitial request. Whenexpedited adversedetermination is made,must also notify thepatient and provider ofright to submitexpedited appeal andthe procedure.May not revoke, limit,condition, or restrict aPA that has beenauthorized unless there isevidence that the PA wasauthorized based onfraud or misinformationor a previously approvedPA conflicts w/ state orfederal law.UR entity must notify in writing thepatient, provider, claimsadministrator of determination onthe appeal w/in 15 days after receiptof the notice of appeal. If the URentity can’t make a determinationw/in 15 days due to circumstancesoutside of its control, may take up to4 additional days. Anymore andmust inform parties of reason.Documentation may include all/partof medical records and writtenstatement from provider. Review ofdocumentation by physician who didnot make adverse determination isrequired.Every April, plans must post: (1) #of PA requests for which anauthorization was issued; (2) # ofPA requests that adversedetermination was issued and sortedby: (i) service; (ii) whetherappealed; and (iii) whether upheld orreversed on appeal; (3) # of PArequests submitted electronically (4)reasons for denials including but notlimited to: (i) patient did not meetPA criteria; (ii) incomplete infosubmitted; (iii) change in treatmentprogram; (iv) patient no longercovered. 2021 American Medical Association. All rights reserved.11Qualifications of reviewerIn cases of appeal to reverse anadverse determination for clinicalreasons, the UR organization mustensure that a physician of URorganization’s choice in the same ora similar specialty as typicallymanages themedical condition, procedure, ortreatment is reasonably available toreview the case.No individual who is performingutilization review may receive anyfinancial incentive based on thenumber of adverse determinationsmade provided that utilization revieworganizations may establishmedically appropriate performancestandards.Other provisionsDefinition of clinicalcriteria: written policies,rules, clinical protocols,medical protocols, or anyother criteria or rationaleused by the UR entity todetermine whether ahealth care service isauthorized.UR org must havewritten standards: (1)written procedures andcriteria used to determinewhether care isappropriate, reasonable,or medically necessary;(2) system for providingprompt notification ofdeterminations andnotifying of appealprocedures; (3)compliance w/ timeframes; (4) writtenprocedures to appealadverse determinations;(5) procedures to ensureconfidentiality of patientspecific information,consistent w/ applicablelaw.Report by 4/1/21 fromcommissioner tolegislature on complianceand additionalinformation from fullyand self-insured plansthat include total PArequest, frequency ofelectronic requests,response times, reasonsfor denial, etc.Applies to:
StateMNCont.Statuteor Reg.or billStandardform?ePAResponse timePA length andretrospective denialDisclosure, appeal, andtransparency requirementsQualifications of reviewerOther provisionsAny medical director whoadministers the utilization reviewprogram or oversees the reviewdecisions shall be a qualified healthcare professional licensed in the stateof Missouri. A licensed clinical peershall evaluate the clinicalappropriateness of adversedeterminations.Payer must review entiremedical record before adenial of emergencycare.Plan must post on its public websitethe PA requirements of org thatperforms UR review for the plan.If, during plan year, coverage termschange or the clinical criteria used toconduct PA change, does not applyuntil the next plan year for patientswho received PA using formercoverage terms or clinical criteria.Does not apply if deemed unsafe, ifindependent source of research/clinical guidelines or evidencedbased standards changes for reasonsrelated to patient harm; or ifreplaced w/ generic rated asequivalent or biologic rates asinterchangeable and 60-day noticegiven.MSMOMSCode201583-9-63Mo stat.376.1350376.1389SB 982(2018)For drugs;cannot exceed2 pagesStandard formmust beavailableelectronically2 business days ofreceiving completedrequest on standardform.2 business days ofobtaining all necessaryinfo. For concurrentreview determinationsw/in 1 working day ofobtaining all necessaryinfo.Electronic notice of new/amendedrequirement must be sent 45 days inadvance to all Minnesota-based, innetwork attending providers who aresubject to the PA requirements.A plan must implement a writtenutilization review program thatdescribes all review activities. Aplan must file an annual report of itsutilization review program activitieswith the director.All review programs must usedocumented clinical review criteriathat are based on sound clinicalevidence. A plan may develop itsown clinical review criteria, orpurchase or license clinical reviewcriteria from qualified vendors. A 2021 American Medical Association. All rights reserved.12Applies to:
StateMOCont.MTStatuteor Reg.or billStandardform?ePATitle 33.Insurance andInsuranceCompanies § 3336-205.NHRSA420-J;7bHB1608(2017)PA length andretrospective denialDisclosure, appeal, andtransparency requirementsQualifications of reviewerOther provisionsApplies gency servicesand stabilizationservices.plan must make available its clinicalreview criteria upon request byregulators.Care for postevaluation/ poststabilization servicesrequired immediatelyafter emergencyservices, plan mustprovide access to anauthorizedrepresentative 24/7 tofacilitate review.NENHResponse timeYesePA w/NCDPDstandardpermitted. Apayer cannot useePA when:pharmacist orprescriber (1)lack broadbandInternet access;(2) has lowpatient volume;(3) has optedout for a certainmedicalcondition or fora patientrequest; (4)lacks a EMR orwhen (5) ePAinterface doesnot provide forAppeals - 1st level: insurer conductstheir own investigation; 2nd level:appeal submitted to an insurerspecific panel for review; 3rd level:insurance director hires appealsreview organization.48 hours for medicallynecessary nonformulary Rx drug. 2021 American Medical Association. All rights reserved.13
StateNHCont.NMStatuteor Reg.or billStandardform?NM Stat§ 59A22-52(2013)Yes (drugsand services)SB 188(2019)ePAthe prepopulation ofprescriber andpatient info; (6)ePA interfacerequires anadditional costto the prescriber.No NCPDPInsurers mustestablishelectronic portalsystem forsecure electronictransmission ofPA requests24/7.Response time7 daysExpedited: 24 hoursReasonable medicalprobability, delay in thetreatment could:(a) seriously jeopardizepatient’slife or overall health;(b) affect patient’sability to regainmaximum function; or(c) subject patient tosevere and intolerablepain.PA length andretrospective denialDisclosure, appeal, andtransparency requirementsQualifications of reviewerOther provisionsBy each Sept. each year the office ofinsurance must provide report to thegovernor and the legislature toinclude, at a minimum:(1) PA datafor each insurer individually andcollectively; (2) the number andnature of complaints against insurersfor failure to follow the Act; and (3)actions taken by the office,including imposition of fines,against insurers to enforcecompliance.Auto-adjud
(ePAs); 3 business days - non-urgent (oral, fax, email); 1 business day - urgent (oral, fax, email) For medical services: 15 days non-urgent, Urgent 72 hours . For concurrent review urgent care requests involving a request by the patient to extend the course of treatment beyond the initial period of time or the number of treatments