Transcription
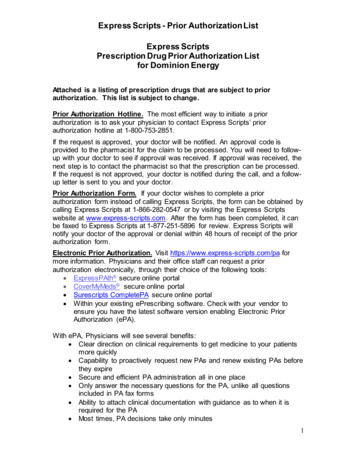
Prior Authorization Requirements forArizona Complete Care MedicaidEffective November 1, 2018General InformationThis list contains prior authorization requirements for UnitedHealthcare Community Plan in Arizona Acute Medicaidparticipating care providers for inpatient and outpatient services. To request prior authorization, please submit yourrequest online, or by phone or fax: Online: Use the Prior Authorization and Notification app on Link. Go to UHCprovider.com and click on the Linkbutton in the top right corner. Then, select the Prior Authorization and Notification app tile on your Link dashboard. Phone: 866-604-3267 Fax: 888-889-1499; fax form is available at UHCprovider.com/AZcommunityplan Prior Authorization andNotification Resources Prior Authorization Paper Fax FormsImportant Information To be eligible for prior authorization, services must be covered benefits as outlined and defined by the ArizonaHealth Care Cost Containment System (AHCCCS). Services provided by non-network health and out-of-state care providers require prior authorization anddocumentation supporting the out-of-network request. Experimental and investigational services are not covered benefits. All rendering providers, facilities and vendors must be actively registered with AHCCCS. Physician Specialty Service delivered inside Multi-Specialy Interdisciplinary Clinics (MSIC) do not requireprior authorization for Special Healthcare Needs (CRS) members. Only one care provider may request services on a prior authorization request form. Only medically necessary, cost effective, and federally- and state-reimbursable services are covered services, asoutlined by AHCCCS.Procedures and ServicesAllergy immunotherapyAdditional InformationFor members younger than age 21:Allergy immunotherapy and allergytesting is covered under Early andPeriodic Screening, Diagnostic andTreatment (EPSDT) when medicallynecessary.For members age 21 and older:Allergy immunotherapy, includingdesensitization treatments administeredby subcutaneous injections (allergyshots), sublingual immunotherapy (SLIT)or another route of administration, is nota covered benefit.Allergy testing, including testing forcommon allergens, is a covered benefitwhen the member has: Sustained an anaphylactic reactionto an unknown allergen Exhibited such a severe allergicreaction where it’s reasonable toassume further exposure to theunknown allergen may result in aCPT is a registered trademark of the American Medical Association.Doc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc. CPT or HCPCS Codes and/orHow to Obtain Prior Authorization
Procedures and ServicesAllergy immunotherapy (cont’d)Bariatric surgeryBehavioral healthAdditional Informationlife-threatening situation. Examplesinclude severe facial swelling,breathing difficulties, epiglottalswelling, extensive urticaria, etc.Prior authorization is required forallergy testing when it meets thecriteria above.Prior authorization required for thecodes listedFor members with serious mentalillness (SMI):Behavioral health services are availablethrough the Regional Behavioral HealthAuthority (RBHA) program at 800-3484058.Bone growth stimulatorElectronic stimulation or ultrasoundto heal fracturesBRCA genetic testingBreast reconstruction (nonmastectomy)Reconstruction of the breast exceptfor after mastectomy CPT or HCPCS Codes and/orHow to Obtain Prior 84743842438484384543860438824388764590The following benefits and/or codes requireprior authorization: Acute inpatient admission Adaptive behavior treatment (ABA) Electroconvulsive therapy Home care training client Psychological testing Out-of-state placement Residential behavioral healthfacility – Level II group home Residential treatment center –Level 1 Transcranial magnetic stimulationPrior authorization required for thecodes listed20975E074920979E0747E0748Prior authorization required for thecodes se direct all lab requests to LabCorpat 800-533-0567 for review andprocessing.Prior authorization required for thecodes 8193801936919396L8600Cancer supportive servicesInjectable colony-stimulating factor drugsPrior authorization required for colonythat require prior authorization:stimulating factor drugs and bonemodifying agent administered in anoutpatient setting for a cancer diagnosisBio similar (Zarxio )Q5101Filgrastim (Neupogen )J1442Pegfilgrastim (Neulasta )J2505Sargramostim (Leukine )J2820Doc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc.
Procedures and ServicesAdditional InformationCancer supportive services(cont’d) CPT or HCPCS Codes and/orHow to Obtain Prior AuthorizationTbo-filgrastim (Granix )J1447Bone-modifying agent that requires priorauthorization:DenosumabJ0897CardiologyPrior authorization required forparticipating physicians for inpatient,outpatient and office-basedelectrophysiology implants prior toperformancePrior authorization required forparticipating physicians for outpatientand office-based diagnosticcatheterizations, echocardiograms andstress echoes prior to performanceChemotherapyFor prior authorization:please submit requests online by using the PriorAuthorization and Notification app on Link. Go toUHCprovider.com and click on the Link buttonin the top right corner. Then, select the PriorAuthorization and Notification app tile on yourLink dashboard. Or, call 888-397-8129.For prior authorization, please submit requestsonline by using the Prior Authorization andNotification app on Link. Go toUHCprovider.com and click on the Link buttonin the top right corner. Then, select the PriorAuthorization and Notification app tile on yourLink dashboard. Or, call 866-889-8054.For more details and the CPT codes that requireprior authorization, please visitUHCprovider.com/AZcommunityplan PriorAuthorization and Notification Resources Cardiology Prior Authorization and NotificationProgramPrior authorization required for injectable Injectable chemotherapy drugs that requirechemotherapy drugs administered in an prior authorization:outpatient setting including intravenous, Chemotherapy injectable drugs (J9000 intravesical and intrathecal for a cancerJ9999), Leucovorin (J0640), Levoleucovorindiagnosis(J0641) Chemotherapy injectable drugs that have aQ code Chemotherapy injectable drugs that have notyet received an assigned code and will bebilled under a miscellaneous HealthcareCommon Procedure Coding System(HCPCS) codeFor prior authorization:please submit requests online by using the PriorAuthorization and Notification app on Link. Go toUHCprovider.com and click on the Link buttonin the top right corner. Then, select the PriorAuthorization and Notification app tile on yourLink dashboard. Or, call 888-397-8129.Chiropractic careFor members younger than age 21:Prior authorization not requiredFor members age 21 and older:CircumcisionChiropractic care is not a coveredbenefit.Routine circumcision is not a coveredbenefit.Prior authorization required only forcases with documented medicalnecessity.Doc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc.54150541605416154162
Procedures and ServicesCochlear and other auditoryimplantsA medical device within the inner earwith an external portion to helppersons with profound sensorineuraldeafness achieve conversationalspeechAdditional InformationFor members younger than age 21: CPT or HCPCS Codes and/orHow to Obtain Prior c and reconstructiveproceduresCosmetic procedures that change orimprove physical appearance without Services or items furnished solely forsignificantly improving or restoringcosmetic purposes are excluded fromphysiological functionAHCCCS coverage.1196015847Reconstructive procedures that treata medical condition or improve orrestore physiologic functionDental servicesDiabetic suppliesPrior authorization required for thecodes listedFor members age 21 and older: Prior authorization required forsupplies, equipment maintenanceand repair of component parts Hardware is not a covered benefit. Clinical documentation mustaccompany and establish medicalnecessity for this service request.Prior authorization required for thecodes 5679226792367966679246795067961For prior authorization requirements,please call UnitedHealthcare Dental at855-812-9208.Diabetic supplies are provided by thelocal pharmacy.To locate contracted care providers or vendors,please visitUHCprovider.com/AZcommunityplanPrior authorization for talking Member Information: Current Medical Plans, IDglucometers available through theCards, Provider Directories, Dental & Visionmedical prior authorization processplansDurable medical equipment (DME) To request DME items, please callFor services not covered by PreferredPreferred Homecare at 800-636-2123.Homecare, please review UnitedHealthcareCommunity Plan’s Provider Manual for a list ofPrior authorization required for the contracted vendors related to DME products atcodes listed with a retail purchase or a UHCprovider.com/AZcommunityplancumulative rental cost of more than 500 Member Information: Current Medical Plans, IDCards, Provider Directories, Dental & VisionThese DME items are not covered byplans.Preferred Homecare:E0194E0265E0266E0270 Bone stimulatorsE0300E0445E0457E0460 Diabetic suppliesE0466E0483E0620E0636 Enclosed bedsE0638E0641E0642E0656 Insulin pumps Percussion vestsE0669E0670E0675E0693 Specialty bedsE0694E0700E0710E0745 Wound etics are not DME – see OrthoticsE1006E1007E1008E1009and prosthetics.E1010E1030E1035E1036E1161E1233Doc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc.E1229E1234E1231E1235E1232E1236
Procedures and ServicesAdditional InformationDurable medical equipment(DME) (cont’d)Enteral services/parenteral/oralTo request services and/or supplies,In-home nutritional therapy eitherplease call Preferred Homecare at800-636-2123.enteral or through a gastrostomytube, total parenteral nutrition (TPN),and/or lipids and oral supplements CPT or HCPCS Codes and/orHow to Obtain Prior l documentation and oral supplementCertificate of Medical Necessity as applicablemust accompany and establish medicalnecessity for this service request.For members younger than age 21:For more information, please review theAHCCCS Medical Policy Manual (AMPM)Chapter 400, Section 430, Policy 430-10 atAZAHCCCS.gov Resources GuidesManuals-Policies AHCCCS Medical PolicyManual (AMPM) Chapter 400, Medical Policyfor Maternal and Child Health 430, EPSDTServices 430-10.The Certificate of Medical Necessity forCommercial Oral Nutritional Supplements canbe found at AZAHCCCS.gov Resources Guides-Manuals-Policies AHCCCS MedicalPolicy Manual (AMPM) Chapter 400, MedicalPolicy for Maternal and Child Health 430-2.For members age 21 and older:Please review AMPM Chapter 300, Policy 310GG at AZAHCCCS.gov Resources GuidesManuals-Policies AHCCCS Medical PolicyManual (AMPM) Chapter 300, Medical Policyfor Covered Services 310, Covered Services 310-GG.The Certificate of Medical Necessity forCommercial Oral Nutritional Supplements canbe found at AZAHCCCS.gov Resources Guides-Manuals-Policies AHCCCS MedicalPolicy Manual (AMPM) Chapter 300, MedicalDoc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc.
Procedures and ServicesEnteral services/parenteral/oral(cont’d)Experimental and investigationalEye care/optometryAdditional InformationPrior authorization required for allservices considered experimental and/orinvestigational CPT or HCPCS Codes and/orHow to Obtain Prior AuthorizationPolicy for Covered Services Chapter 300 Overview Attachment 226186866180For more information, please refer to95978A4638A9274E1831AMPM Chapter 300, Section 320, Policy320-B at AZAHCCCS.gov Resources Guides-Manuals-Policies AHCCCSMedical Policy Manual (AMPM) Chapter 300, Medical Policy for CoveredServices 320, Services With SpecialCircumstances 320-B.Benefits provided for membersFor member eye care services, please callyounger than age 21:Nationwide Vision at 800-481-2779. One routine eye exam every 12months Regular single vision bifocal ortrifocal polycarbonate lenses Frame for up to 79.99 retail price One replacement pair of glasses iflost, stolen or damaged Members may pay the difference fora more expensive pair of glasses,but must sign a waiver provided byNationwide Vision.For members age 21 and older:Prior authorization required whenmedically necessary to diagnose or treatdiseases and conditions of the eyeFemoracetabular impingementsyndrome (FAI)Functional endoscopic sinussurgery (FESS)Prior authorization required for thecodes listedPrior authorization required for thecodes listedGenetic testingPrior authorization required for allservices not covered by LabCorpTo determine prior authorizationrequirements, please call LabCorp at800-788-9743.Hearing servicesFor members younger than age 21:Hearing evaluations and hearing aidsPrior authorization not requiredFor members age 21 and older:Prior authorization requiredHome health care servicesDoc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc.Prior authorization required for thecodes 9G03003125531267
Procedures and ServicesIncontinence suppliesInfusion in-home servicesInjectable medicationsfor in-home usageInjectable medicationsAdditional InformationIncontinence supplies are a benefit onlywhen provided through PreferredHomecare.Prior authorization required for allservices not covered by PreferredHomecarePrior authorization required for allmedications not covered by PreferredHomecarePrior authorization required for thecodes listed CPT or HCPCS Codes and/orHow to Obtain Prior AuthorizationTo request incontinence supplies, please callPreferred Homecare at 800-636-2123.To request services and/or supplies, please callPreferred Homecare at 800-636-2123.To request medications, please call PreferredHomecare at 800-636-2123.Actemra ****J3262 ActharJ0800Botulinum toxinsJ0585J0586J0587J0588Brineura C9014Cerezyme **J1786 CinqairJ2786Elelyso **J3060 ****EntyvioJ3380Exondys 51 **J1428Fasenra C9466Ilaris J0638 57J1559J1561J1566J1568J1569J1572J1575J1599 LemtradaJ0202Luxturna C9032MakenaJ1726Nucala * J2182Ocrevus J2350Doc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc.J1729J2675
Procedures and ServicesInjectable medications (cont’d)Additional Information CPT or HCPCS Codes and/orHow to Obtain Prior AuthorizationOrencia ****J0129Parsabiv J0606Probuphine J0570Radicava C9493 ****RemicadeJ1745Renflexis ****Q5104Simponi Aria ****J1602Soliris **J1300Spinraza **J2326Sublocade Q9991Q9992Synagis **90378Unclassified codes***C9399J3490J3590 VPRIVJ3385 **XolairJ2357Please check our Review at Launch for New toMarket Medications policy for the most up-todate information on drugs newly approved by theFood & Drug Administration (FDA) and includedon our Review at Launch Medication List. Predetermination is highly recommended for thedrugs on the list. The Review at Launch for Newto Market Medications policy is available atUHCprovider.com Menu Policies andProtocols Community Plan Policies Medical& Drug Policies and Coverage DeterminationGuidelines for Community Plan.* For Makena prior authorization, please fax888-899-1499. Fax forms are available atUHCprovider.com/AZcommunityplan PriorAuthorization and Notification Resources PriorAuthorization Paper Fax Forms** For Cerezyme, Elelyso, Exondys 51, Soliris,Spinraza, Synagis and Xolair prior authorization,please call the Pharmacy Prior AuthorizationService at 800-310-6826.Doc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc.
Procedures and ServicesAdditional InformationInjectable medications (cont’d)Inpatient admission*** For Unclassified codes C9399, J3490 andJ3590, prior authorization is only required forBrineura, Crysvita , *Fasenra, Luxturna ,Radicava and Trogarzo **** Prior authorization is required for dates ofservice 10/15/18 and afterNotification required for admissionsJoint replacementPrior authorization required for theJoint, total hip and knee replacement codes listedproceduresLaboratory servicesPrior authorization requiredNon-emergent air ambulancetransportOrthognatic surgeryTreatment of maxillofacial/jawfunctional impairmentPrior authorization required for thecodes listedPrior authorization required for thecodes listedOrthotics and prostheticsPrior authorization required for thecodes listed with a retail purchase or acumulative rental cost of more than 500For members younger than age 21with orthotic limitation: Reasonable repairs or adjustmentsof purchased orthotics are coveredfor all members to make the orthoticserviceable and/or when the repaircost is less than purchasing anotherunit. The component will be replaced if, atthe time authorization is requested,documentation is provided toestablish that the component is notoperating effectively.For members age 21 and older:AHCCCS orthotics coverage applies if: The use of the orthotic is medicallynecessary as the preferred treatmentoption consistent with Medicareguidelines. The orthotic is less expensive thanall other treatment options or surgicalprocedures to treat the samediagnosed condition.Doc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc. CPT or HCPCS Codes and/orHow to Obtain Prior 4472713827486274122748727446298662986729868Please call LabCorp at 905L3976L3961L3977L3971L3999L3975L4000
Procedures and ServicesOrthotics and prosthetics (cont’d)Doc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc.Additional Information The orthotic is ordered by aphysician or primary care provider. CPT or HCPCS Codes and/orHow to Obtain Prior 040L7190L8042L7191L8043L8044L8045L8046L8047
Procedures and Services Additional InformationCPT or HCPCS Codes and/orHow to Obtain Prior AuthorizationOrthotics and prosthetics (cont’d)Out-of-network servicesOut-of-state servicesOutpatient therapyPrior authorization required for all out-ofnetwork servicesBenefit only approved when service isemergent or unavailable in the state ofArizonaFor members younger than age 21:Prior authorization required after the 12visitthOccupational, physical and speechtherapy is covered in an inpatient oroutpatient setting. No benefit limitsapply.For members age 21 and 9Prior authorization not requiredOutpatient speech therapy is not acovered benefit.Occupational and physical therapy arecovered in an inpatient or outpatientsetting. Outpatient occupational andphysical therapy are: Limited to 15 occupational andphysical therapy visits per benefityear, Oct. 1 - Sept. 30, to help anindividual restore a skill or level offunction, and maintain it. Limited to 15 occupational andphysical therapy visits per benefityear, Oct. 1 - Sept. 30, to help anindividual acquire a new skill or levelof function, and then maintain it.For QMB members:Pharmacy drugsCovered for unlimited visits whenmedically necessaryA list of medications requiring priorauthorization is available atUHCprovider.com/AZcommunityplan Pharmacy Resources and PhysicianAdministered DrugsService requests must include “J”Codes and NDC Codes for themedication requested.The following hemophilia factor/biotechdrugs are included on the priorauthorization list: Acthar gel Aldurazyme Ceprotin Cerezyme Cinryze Elaprase Elelyso Fabrazyme Doc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc.For pharmacy prior authorization, please contactUnitedHealthcare Pharmacy Prior AuthorizationService by:Phone: 800-310-6826Fax: 866-940-7328For specialty pharmacy prior authorization,please fax 866-940-7328.Fax forms are available atUHCprovider.com/AZcommunityplan Pharmacy Resources and PhysicianAdministered Drugs Pharmacy PriorAuthoriazation Pharmacy Prior AuthorizationForms . For specific medications listed in thissection, click on the medication and use theattached service request form specific to thatdrug.
Procedures and ServicesPharmacy drugs (cont’d)Pregnancy terminationAdditional Information Juxtapid Kalydeco Kuvan Kynamro Lumizyme Myozyme Orfadin VPRIV Prior authorization required for thecodes listed CPT or HCPCS Codes and/orHow to Obtain Prior 522598505985659851598577752377525Prior authorization includes Mifepristone, Mifeprex or RU-486Clinical documentation and theCertificate of Medical Necessity forpregnancy termination mustaccompany the prior authorizationrequest form.For more information, please reviewAMPM Chapter 400, Section 410,Section E Pregnancy Termination atAZAHCCCS.gov Resources Guides-Manuals-Policies AHCCCSMedical Policy Manual (AMPM) Chapter 400, Medical Policy for Maternaland Child Health 410, Maternity CareServices Section E PregnancyTermination.Private duty nursingProton beam therapyFocused radiation therapy usingbeams of protons, which are tinyparticles with a positive chargeRadiologyThe Certificate of Medical Necessity ForPregnancy Termination can be found atAZAHCCCS.gov Resources Guides-Manuals-Policies AHCCCSMedical Policy Manual (AMPM) Chapter 400, Medical Policy for Maternaland Child Health Attachment C.Prior authorization required for thecodes listedPrior authorization required for thecodes listedPrior authorization required forparticipating physicians who requestthese advanced outpatient imagingprocedures: Certain CT, MRI, MRA and PETscans Nuclear medicine and nuclearcardiology proceduresCare providers ordering an advanced outpatientimaging procedure are responsible for providingnotification prior to scheduling the procedure.For prior authorization, please submit requestsonline by using the Prior Authorization andNotification app on Link. Go toUHCprovider.com and click on the Link buttonin the top right corner. Then, select the PriorAuthorization and Notification app tile on yourLink dashboard. Or, call 866-889-8054.For more details and the CPT codes that requireprior authorization, please visitUHCprovider.com/AZcommunityplan PriorAuthorization and Notification Resources Radiology Prior Authorization and NotificationProgramDoc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc.
Procedures and ServicesAdditional InformationRhinoplasty and septoplastyTreatment of nasal functionalimpairment and septal deviationPrior authorization required for thecodes listedSinuplastyPrior authorization required for thecodes listedPrior authorization only required whenrequesting service in an outpatienthospital settingSite of service (SOS) – outpatienthospitalPrior authorization not required ifperformed at a participating AmbulatorySurgery Center (ASC) CPT or HCPCS Codes and/orHow to Obtain Prior 4623046531295312963129731298Carpal tunnel surgery64721Cataract 385Cosmetic and ar, nose and throat (ENT) procedures2132069631301403052069436Gynecologic procedures5752258353585585856358565Hernia 5Liver nsillectomy and adenectomy4282042821428254283042826Upper and lower gastrointestinal endoscopy432354323943249Urologic proceduresDoc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, 23325226052351523525570052353572885235655040
Procedures and ServicesSkilled nursing facility servicesAdditional InformationPrior authorization requiredSleep apnea procedures andPrior authorization required for thesurgeriescodes listedMaxillomandibular advancement andoral-pharyngeal tissue reduction fortreating obstructive sleep apneaSpecialty/enclosed bedsPrior authorization required for thecodes listedSpinal stimulator for painmanagementSpinal surgerySterilizationPrior authorization required for thecodes listedPrior authorization required for thecodes listedPrior authorization required for thecodes listedFor all members younger than age 21:Prior authorization requiredAny member requesting sterilizationmust sign an appropriate Consent forSterilization form.For more information, please reviewDoc#: PCA-4-010492-04202018 06062018 2018 United HealthCare Services, Inc. CPT or HCPCS Codes and/orHow to Obtain Prior 5525854458553
Procedures and ServicesSterilization (cont’d)Additional InformationAMPM Chapter 400, Section 420,Section E Sterilization atAZAHCCCS.gov Resources Guides-Manuals-Policies AHCCCSMedical Policy Manual (AMPM) Chapter 400, Medical Policy for Maternaland Child Health 420, Family Planning Section E Sterilization. CPT or HCPCS Codes and/orHow to Obtain Prior 525The Consent to Sterilization form can befound at AZAHCCCS.gov Resources Guides-Manuals-Policies AHCCCSMedical Policy Manual (AMPM) Chapter 400, Medical Policy for Maternaland Child Health 420, Family Planning Attachment A.Transplant servicesPrior authorization required for thecodes listedFor transplant and CAR T-cell therapy servicesincluding Kymriah (tisagenlecleucel) andYescarta (axicabtagene ciloleucel), please callClinical documentation to support the the UnitedHealthcare Community and Stateneed for transplants must accompany Transplant Case Management Team at 800and establish medical necessity for418-4994 or the notification number on the backservice request.of the member’s health plan ID 471474714448
prior authorization for Special Healthcare Needs (CRS) members. Only one care provider may request services on a prior authorization request form. Only medically necessary, cost effective, and federally- and state-reimbursable services are covered services, as outlined by AHCCCS.