Transcription
11/6/2013Thursday, November 7, 2013These presenters havenothing to discloseIHI ExpeditionTreating Sepsis in the Emergency Department and BeyondSession 5Andy Odden, MDDiane Jacobsen, MPH, CPHQToday’s Host2Max Cryns, Project Assistant, Institute for HealthcareImprovement (IHI), assists programming activities forhospital settings including Expeditions (2-4 month webbased educational programs), Passport memberships,and mentor hospital relations. He also supports IHI’snetworking and knowledge efforts. Max is currently inthe Co-Operative Education Program at NortheasternUniversity in Boston, MA, where he majors in BusinessAdministration with concentrations in Entrepreneurshipand Marketing. He enjoys professional and collegiatesports, playing basketball, music, the beach, and trivia.1
11/6/2013WebEx Quick Reference3 Welcome to today’s Raise your handsession!Please use chat to “AllParticipants” for questionsFor technology issues only,please chat to “Host”WebEx Technical Support:866-569-3239Dial-in Info: Communicate /Join Teleconference (in Select Chat recipientmenu)Enter TextWhen Chatting 4Please send your message toAll Participants2
11/6/2013Expedition Director5Diane Jacobsen, MPH, CPHQ, Director, Institute forHealthcare Improvement (IHI) is currently directing theCDC/IHI Antibiotic Stewardship Initiative, NSLIJ/IHIReducing Sepsis Mortality Collaborative. Ms Jacobsenserved as IHI content lead and improvement advisor for theCalifornia Healthcare-Associated Infection PreventionInitiative (CHAIPI) and directed Expeditions on AntibioticStewardship, Preventing CA-UTIs, Reducing C. difficileInfections, Sepsis, Stroke Care and Patient Flow. Sheserved as faculty for IHI’s 100,000 Lives and 5 Million LivesCampaign and directed improvement collaboratives onSepsis Mortality, Patient Flow, Surgical Complications,Reducing Hospital Mortality Rates (HSMR) and co-directedIHI's Spread Initiative She is an epidemiologist withexperience in quality improvement, risk management, andinfection control in specialty, academic, and communityhospitals. A graduate of the University of Wisconsin, sheearned her master's degree in Public Health-Epidemiology.from the University of Minnesota.Today’s Agenda6IntroductionsDebrief: Session 4 ActionPeriod AssignmentEarly Recognition andMonitoring of the SepsisPatient on the Inpatient FloorAction Period Assignment3
11/6/2013Expedition Objectives7By the end of the Expedition participants will be ableto:Describe the latest evidence based care for patientswith severe sepsis and septic shockDesign reliable processes to ensure that eachpatient receives all elements of the best possiblecare at each opportunityIdentify key opportunities and test changes onmedical/surgical units to improve early recognition ofsepsis in a care context which has been challengingfor providersSchedule of Calls8Session 1 – Clinical Updates to the Surviving Sepsis Campaign Guidelines: The 3Hour Resuscitation BundleDate: Thursday, September 12, 1:00-2:30 PM ETSession 2 – Key Considerations for Enhancing Reliability with Antibiotic Therapyin the Emergency Department and in Inpatient FloorDate: Thursday, September 26, 1:00-2:00 PM ETSession 3 – Lactate and Blood Culture Collection: Getting to Results Within OneHourDate: Thursday, October 10, 1:00-2:00 PM ETSession 4 – Ensuring Reliable Care from the Patient PerspectiveDate: Thursday, October 24, 1:00-2:00 PM ETSession 5 – Early Recognition and Monitoring of the Sepsis Patient on theInpatient FloorDate: Thursday, November 7, 1:00-2:00 PM ETSession 6 – Considerations and Challenges with Fluid ResuscitationDate: Thursday, November 21, 1:00-2:00 PM ET4
11/6/20139FacultyAndy Odden, MD, is a hospitalist at the University ofMichigan and the Ann Arbor VA. His research focuseson the management and outcomes of severe sepsis onthe general inpatient ward. He is the founder andDirector of the Hospitalist Program at the Ann Arbor VA,where he serves as Chief of the Hospital MedicineSection and Director of the Inpatient Care CoordinatorProgram at that institution. He is a faculty mentor for theMichigan Transitions of Care Collaborative and an activemember of the Society of Hospital Medicine. As amember of the IHI faculty, he is working with the NorthShore‒Long Island Jewish Health System to reduceinpatient sepsis mortality.Debrief: Session 4 Action PeriodAssignment10Ensuring Reliable Care From the Patient PerspectiveIdentify one (or more) elements of the 3 hour bundle with anopportunity to improve reliability:– Lactate collection– Blood cultures prior to antibiotics– Antibiotics– FluidsDesign a PDSA within the process of care to improve thetimeliness of one (or more) of the 3 hour bundle elements5
11/6/2013Intermountain Experience: Impact ofIncreased Reliability on MortalitySession 5 Action Period Assignment1112Design a PDSA to enhance early recognition of sepsison the inpatient floor, considering:– MEWS (modified early warning system)– Rapid Response Team/System– Situational awareness6
11/6/201313Early Recognitionand Monitoring of theSepsis Patient on theInpatient FloorRoadmap14Why do we care about early recognition on the floor?What is the scope of sepsis on the inpatient floors?What are the unique barriers to identifying sepsis on theinpatient floors?How can sepsis recognition be improved?7
11/6/2013Four Main Types of Patients15Admitted with a diagnosis of sepsis from the EDProgression of sepsis/severe sepsis/infection from theED“De novo” floor sepsisTransfer from the ICU after stabilizationFailure to Recognize16Partial or substandard care to individual patientsIncomplete view of process improvement initiatives8
11/6/2013Surviving Sepsis Floor Sepsis Initiative17National collaborative announced October 2013Recognizes the importance and unique challenges ofnon-ICU sepsisAim: Increase early recognition and treatment of patientswith sepsis outside of the ICUPoll Question18Does your hospital have a quality improvement effortspecifically focused on improving floor (non-ED, nonICU) sepsis?– Yes– No– Unknown9
11/6/2013Sepsis on the Inpatient Floor19Much progress in the care of the sepsis syndromeRecognition, treatment, and improvement efforts:Focused on ED and ICU populationsEnormous potential to save and improve livesBut is it a problem on the floor The “Septic” Patient2010
11/6/2013Is Sepsis a Problem on the Floor?21Where is sepsis diagnosed?ED and ICU?Where are these patientscared for?The floor: “Diet Sepsis”?How well is it recognized?The few that “slip through thecracks”Poll Question22What percentage of patients with severe sepsis or septicshock outside the ICU do you think are recognized assuch at the time of treatment?– 80%– 60-80%– 40-60%– 20-40%– 20%11
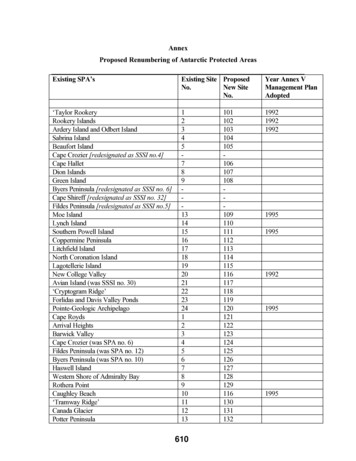
11/6/2013Where Do Sepsis Patients Receive Care?23Angus (CCM 2001;29(7):1304-1310)– 48.9% of severe sepsis patients do not receive ICU care– Academic: 48.2%– Non-academic: 49.2%– 32% receive all care on the inpatient ward (CCU, chronic ventexcluded)Sundarajaran (CCM 2005;33(1):71-80)– 50% of severe sepsis patients do not receive ICU careWhere Do Sepsis Patients Receive Care?Phase of SepsisICU AdmissionRateSepsis12%Severe Sepsis32%Septic Shock75% Prospective cohort Rigorous definition forsepsis 3 Spanish hospitals 702 patients followed untilhospital dischargeEsteban CCM 2007;35:1284-1289.2412
11/6/2013Inpatient Sepsis: A Problem25Most conservative estimates: 32%-50% of severe sepsisdo not receive ICU careAre the numbers inflated by the inherent flaws ofepidemiologic studies? Do these data apply to theinpatient floor?Do these Data Apply?26Concern regarding applicability of Angus implementationusing ICD-9 codes to non-ICU patients– Selection bias, patient differencesPatient-level validation for non-ICU severe sepsispatients (Iwashyna et al. Med Care 2012)– PPV 71%– NPV 92%13
11/6/201327Are the Patients Different?32%-50% of severe sepsis patient never receive ICUcareAre there systematic differences between ICU and nonICU patients?Are floor sepsis patients just “less sick”?Inpatient Sepsis: MortalityPhase of SepsisSepsisNon-ICU Mortality Location ofTreatment8%Severe SepsisMortalitySevere Sepsis26%ICU32%Septic Shock53%Non-ICU29%Sundarajaran (CCM 2005;33(1):71-80Esteban CCM 2007;35:1284-12892814
11/6/2013Rivers Study: Baseline VariablesPhysiologic VariableTreatment armControl armTemperature35.9 ⁰C ( /- 3.2)36.6 ⁰C ( /- 2.3)Heart Rate117 ( /-31)114 ( /- 27)Systolic Blood Pressure106 ( /-36)109 ( /-34)Respiratory Rate32 ( /- 11)30 ( /- 11)WBC13,600 ( /- 8,300)14,200 ( /- 9,600)Lactate7.7 ( /- 4.7)6.9 ( /- 4.5)29Other characteristics:Diagnosis: Pneumonia (39%), UTI (26%)Age: 66Co-morbidities: Diabetes (31%), renal failure (21%), COPD (16%)Blood cultures negative in 65%All cultures negative in 24%Rivers NEJM 2001;345(19):1368-1377.Differences Between ICU and Non-ICU30The Michigan Non-ICU Sepsis Group (Rohde JHM 2013)– Site of infection– Organ dysfunction– Documentation of sepsisRetrospective cohort– Detailed hospitalist review: Site of infection, organ dysfunction– 64 patients included in the final cohort: Limitation15
11/6/2013Site of Infection: ICU and non-ICU31Angus CCM 2001;29(7):1304-1310Rohde JHM 2013;8(5):243-247Organ Dysfunction: ICU and non-ICU32Angus CCM 2001;29(7):1304-1310Rohde JHM 2013;8(5):243-24716
11/6/201333Documentation Gap Recognition Gap?Rohde JHM 2013;8(5):243-247How Well is it Recognized?3450% of non-ICU severe sepsis patients did not have“sepsis” of any degree documented by the treatingclinicianThe clinician’s view: infection and a new organdysfunction, not severe sepsisRohde JHM 2013;8(5):243-247.17
11/6/2013Barriers to Recognition: Patient-Level35Identifying the patient who clearly has sepsis– Less of a diagnostic challenge– Typically: septic shock, systemic hypoperfusionAmbiguity: Infection plus SIRS plus new organdysfunction– Under-recognized– Anchoring bias36Barriers to Recognition: SystemsAsynchronous information– Labs, vital signs, assessmentsHandoffs– Shift, transfer– MD, RN, NP, PACommunication within/between disciplines– MA, RN, physician, mid-level18
11/6/2013Barriers to Recognition: Providers37No single pattern to recognizeAnchoring heuristic– Pneumonia renal failure severe sepsis?Multiplicities– Physicians– Nurses– Pharmacists– Wards/unitsPoll Question38What is your hospital’s biggest barrier to timely diagnosisof sepsis on the inpatient floors?– Timing of vital signs– Timing of labs– Physician acceptance of non-ICU sepsis– Delay of physician assessment– Handoffs between providers– Other19
11/6/2013Time Zero: A Word39Improvement strategies require an agreed-upon timezero from which process measures can be assessedED: Triage time serves as a convenient time zeroOn the inpatient floor, defining time zero is challengingStrategies for Sepsis Recognition40MEWS-based sepsis screeningProvider educationSituational Awareness“Code sepsis”RRT20
11/6/2013MEWS41Modified Early Warning SystemDetect subtle changes in patient status before majorproblems developParameters: HR, BP, pulse, temp, urine output, LOCDevelop a clear action plan based on MEWS results– When to involve physician, RRT, intensivist, etc.– Not a substitute for clinical judgmentProvider Education42Multiple aspects: Diagnostic criteria, importance, impactPhysicians, nursing, medical assistants, laboratoryHelp people to see how their work has an impact onpatient care– Data and anecdotes– Tie to daily work flow21
11/6/2013Questions?43Raise your handUse the ChatAction Period Assignment44Design a PDSA to enhance early recognition of sepsison the inpatient floor, considering:– MEWS (modified early warning system)– Rapid Response Team/System*– Situational awareness*i.e. – incorporating sepsis screen22
11/6/2013Expedition Communications45Listserv for session communications:TreatingSepsis@ls.ihi.orgTo add colleagues, email us at info@ihi.orgPose questions, share resources, discuss barriers orsuccessesNext (Final) Session46Thursday, November 21st, 1:00-2:00 PM ETSession 6 - Considerations and Challenges with FluidResuscitation23
Angus (CCM 2001;29(7):1304-1310) - 48.9% of severe sepsis patients do not receive ICU care - Academic: 48.2% - Non-academic: 49.2% - 32% receive all care on the inpatient ward (CCU, chronic vent excluded) Sundarajaran (CCM 2005;33(1):71-80) - 50% of severe sepsis patients do not receive ICU care 23 Where Do Sepsis Patients Receive Care?