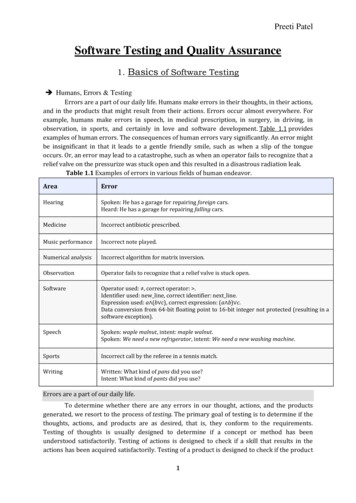
Transcription
3M Quality Measures:3M Potentially Preventable EventsSeptember 26, 2018
Overview Introduction Provide Overview of 3M History with Florida and Florida Health Finder Potentially Preventable Events- the Big Picture Premise Costs Savings Populations Risk adjustment Overview Potentially Preventable Readmissions (PPR) Overview Potentially Preventable Admissions (PPA) Overview Potentially Preventable ER Visits (PPV) Adding Value through Additional Data Quality Performance – Providers Perspective24 September 3M 2018. All Rights Reserved. 3M Confidential.2
3M Health Information Systems:Deep Experience in Payment and Measurement InnovationU.S. Adoption of 3M Patient Classification Systems 35 years in health information and paymentsystems Industry leader for methodologies,classification, payment systems and coding,used by CMS, MedPAC, 38 states, 200 payers,& 80% of U.S. hospitals 3M has combined with the computing power,search capabilities and prioritizationalgorithms of Verily (formerly Google LifeSciences), forming a unique partnership thatprovides both payers and providers withknowledge from a single source of truth24 September 3M 2018. All Rights Reserved. 3M Confidential.22 states (27 grouper adoptions) through 1983-200611 additional states (37 grouper adoptions) 2007 – 20106 additional states (33 grouper adoptions) 2011 – Q3 2012More Than 5,000 U.S. Hospitals Trust 3M HIS3
Broad based experience1 billion claims per month54 million covered lives5,000 U.S. hospitals200 private insurers38 state agencies, CMS, and MedPAC97% customer retention24 September 3M 2018. All Rights Reserved. 3M Confidential.4
3M Methodology Use by the State of Florida The 2012 Florida Legislature mandated Agency for Health Care Administration (AHCA)implement inpatient payments utilizing 3MTM All Patient Refined Diagnostic Related Groups(APR DRGs) beginning in July 2013. The 2016 Florida Legislature mandated AHCA implement a new outpatient paymentmethod utilizing 3MTM Enhanced Ambulatory Patient Groups (EAPGs) for Florida Medicaidon July 1, 2017. 3M Clinical Risk Groups (CRGs) are used by AHCA, Business Intelligence Unit , MedicaidData Analytics to analyze the disease burden of Florida Medicaid enrollees.24 September 3M 2018. All Rights Reserved. 3M Confidential.5
3M Methodology Use by the State of Florida Potentially Preventable Events – Beginning in 2019, new managed care contracts mustdemonstrate how a Plan will reduce potentially preventable hospital admissions,readmissions, emergency department use, and use of unnecessary ancillary services FloridaHealthFinder.gov In June 2008, FloridaHealthFinder.gov was updated to include 3MTM PotentiallyPreventable Readmission Rates (replacing general readmission rates), based on APRDRGs 3M also processes data to calculate additional measures including length of stay,provide data on specific conditions using EAPGs and APR-DRGs, and calculate variousAHRQ measures24 September 3M 2018. All Rights Reserved. 3M Confidential.6
Potentially Preventable EventsPotentially PreventableReadmissions (PPR)Result of poorcontinuity/transitions of careOvertreatmentPotentially PreventableComplications (PPC)Reflect processesof careComplicationsPotentially PreventableEmergency Room Visits (PPV)Result of inadequateaccess to careNever eventsPotentially PreventableAdmissions (PPA)Result of inadequatecoordination of careUnnecessary servicesPotentially PreventableAmbulatory Services (PPS)24 September 3M 2018. All Rights Reserved. 3M Confidential.Avoidable services outsideinpatient settingInappropriate care7
Typical Distribution of Potentially Preventable OpportunityAchieving value comes withincreasing difficulty.Facility/Primary Care24 September 3M 2018. All Rights Reserved. 3M Confidential.Facility/Primary Care Primary CarePrimary Care/Specialty Care/Facility8
Real resultsBetter results.Fewer readmissions.20% reduction in readmissions—or 8,800healthy nights at home—leading to 70 millionin savings*Sustainable cost savings.With better quality. 35 million in avoided costs with betterprimary care, reduced ER visits andreadmissions, and higher continuity of care* 35 millionIn waste avoided20%Readmissionreduction* MinnesotaMedicaid and DOHusing 3M PPRs24 September 3M 2018. All Rights Reserved. 3M Confidential.* WellmarkCommercial ACOsin Iowa9
Potentially Preventable Events: costs by segment3M Clinical Risk Groups categorize persons by their overall illness burden, regardless of specific disease status, as the foundation for populationhealth management.Targets forfocused caremanagementPopulation health segments are groupings of 3MTM Clinical Risk Groups.24 September 3M 2018. All Rights Reserved. 3M Confidential.10
Over-utilization and 3M Potentially Preventable Events3M Potentially Preventable Admissions (PPAs), Readmissions (PPRs), and ED Visits (PPVs) provide a set ofclinically-based tools that can, when evaluated on a risk-adjusted basis, identify health services that might havebeen avoided through effective care coordination. PPA (red bars) rates are displayed in units of per thousand persons per year (PKPY). Expected values (black lines) are risk-adjusted network means.24 September 3M 2018. All Rights Reserved. 3M Confidential.11
Types of Potentially Preventable EventsPotentially Preventable Readmissions (PPR)Potentially Preventable Initial Admissions (PPA)Potentially Preventable ED Visits (PPV)Potentially Preventable Complications (PPC)Potentially Preventable Services (PPS)24 September 3M 2018. All Rights Reserved. 3M Confidential.12
Potentially Preventable ReadmissionsPotentially Preventable Readmissions tendto be the failure of appropriatecoordination at the point of dischargeeither for post discharge services and careor as a result of a discharge that occursprematurely. These reasons suggest thatresults are as much a facility attribute asthey are shortcoming in primary carecoordination and follow-up.24 September 3M 2018. All Rights Reserved. 3M Confidential.Best PracticePresent as a‘rate’ andidentify outliersin performanceIncentives forimprovementyear/yearProvideactionableinsight forimprovement13
Identification of patients with 3M PPRsPHASE 1PHASE 2Identify ExcludedAdmissions and NonEventsDetermine PreliminaryClassification ofRemaining AdmissionRemove admissionswhere preventability isdifficult to determine: Excluded admissionsNon-events24 September 3M 2018. All Rights Reserved. 3M Confidential.Compare withReadmission Time intervalDetermine if admissioncan be a ReadmissionPHASE 3Identify PPRs andDetermine FinalClassification ofAdmissionsLook across admissions:Determine ClinicalRelevanceIdentify theReadmission Chains14
3M Potentially PreventableAdmissions (PPAs)Potentially Preventable Admissions areambulatory sensitive conditions that mayhave resulted from lack of adequate access tocare. The occurrence of high rates of PPAsrepresents failure of ambulatory careprovided. Since the majority of PPAs areadmitted through the emergency department,it is best practice to measure concurrentlywithPotentially Preventable Visits (PPVs)Assumptions: Not all ambulatorysensitive admissions arepreventable PPAs may result when: Nursing facility care issub-standard Poor medicationmanagement Poorly managed chronicconditions Poor ED management Poorly aligned facilitypayment Use APR DRG foundation24 September 3M 2018. All Rights Reserved. 3M Confidential.15
3M Potentially Preventable Visits(PPVs)Potentially Preventable Emergency Room Visits(PPVs) are emergency room visits that may resultfrom a lack of adequate access to care orambulatory care coordination. In general, theoccurrence of high rates of PPVs represents afailure of the ambulatory care provided to thepatient, or the result of actions taken or omittedduring the hospital stay, such as incompletetreatment or poor care of the underlying problemand/or poor coordination with the primary care orspecialist physician.24 September 3M 2018. All Rights Reserved. 3M Confidential.Assumptions: Not all emergencydepartment visits arepreventable PPVs may result when: Poor access to primarycare Poor relationship withprimary care Poor medicationmanagement Poorly managed chronicconditions Use Enhanced AmbulatoryPayment Groups (EAPGs)as foundation16
Data Sources – Adding Value to AnalyticsFloridaHealthFinder.gov: Currently utilizes discharge data.Quarterly Statewide Medicaid Managed Care Report: Utilizes eligibility, encounter, and claims data Florida MedicaidManaged Information System (FLMMIS)Claims Data can Provide: More Complete Longitudinal View of Patient Additional Value to CRG by adding Professional Services,Behavioral Health, and Pharmacy Provides more actionable data through more holistic view of apatient/member’s services24 September 3M 2018. All Rights Reserved. 3M Confidential.17
Managing Quality Performance – Providers Perspective24 September 3M 2018. All Rights Reserved. 3M Confidential.18
Managing Quality Performance – Providers Perspective24 September 3M 2018. All Rights Reserved. 3M Confidential.19
Questions?Mike McCarthymcmccarthy@mmm.com
More Than 5,000 U.S. Hospitals Trust 3M HIS 22 states (27 grouper adoptions) through 1983-2006 11 additional states (37 grouper adoptions) 2007 -2010 6 additional states (33 grouper adoptions) 2011 -Q3 2012 U.S. Adoption of 3M Patient Classification Systems 3M Health Information Systems: Deep Experience in Payment and Measurement Innovation