Transcription
Introduction toPostabortion Care(PAC)Postabortion Care (PAC) Postabortion care is the management ofa medical emergency It is care for women with complicationsof abortion You are already providing PAC services Our aim is to improve the quality andexpand the services available21
ObjectivesBy the end of this session, we will be ableto: Explain the importance of PAC List the key elements of quality PACservices Defend the rational for this program3Elements of Postabortion CareEmergencyTreatmentFP Counseling& ServicesOtherReproductiveHealth Services42
Importance of PAC Services PAC is a life-saving service Death from abortion complications ispreventable We have the technology to makequality PAC services much moreaccessible Most unwanted pregnancies, andtherefore abortions, are preventable5Importance of PAC Programs Many hospitals manage patients withcomplications of abortions, but . . . Quality, accessible PAC services arecurrently only available in a fewhospitals63
The Scope of the Problem 70 million unwanted pregnancies yearly 40-60 million abortions performed everyyear 20 abortions occur in unsafe conditions 99 % of these occur in developingcountries 25-50 % of them Among Teenagers7The Scope of the Problem (cont.) 600,000 women die annually in the worldfrom pregnancy related causes 70,000 women die annually from abortion 13-50% of MMR is due to complications ofabortion 15-60 % gynaecological beds in hospitalsoccupied by postabortion cases84
The Scope of the Problem (cont.)Plus . . . 15% of all pregnancies result inspontaneous abortions – many clientsseeking PAC services have had amiscarriage9In Zambia 649/100,000 live births (1996 DHS) 1,000-2,000/100,000 reported in somedistricts PAC caseload doubled in 10 years– 16,000 PAC Admissions in UTH, 1993– 16,000 in first half of 2002105
Why is the risk so high in Africa? Emergency services are not accessibleFew paramedical staff are trained in PACPatients arrive in late and in poor conditionServices are not available on an emergency,immediate basis D&C is the primary clinical management– added delays waiting for OT time and staff– added risk of complications Community understanding is poor andcultural barriers are a reality11Postabortion Care: Rationale for UsingManual Vacuum Aspiration (MVA)MVA is the preferred treatment ofincomplete abortion because:– Risk of complications is reduced– Access to services is increased– Cost of postabortion services & consumption/use of resources is reduced– Immediate access to emergency care is muchmore likely126
Comparison of Complication RatesSummary of 13 StudiesComplications(major only)VacuumAsp.(Range %)D&C(Range %)Summary(Rate D&C)Excessiveblood loss0-15.70.5-2810/13 (78%)Pelvic infection0.2-5.40.7-67/9 (78%)Cervical injury0-3.10.3-6.46/7 (86%)Uterineperforation0-0.50-3.310/12 (83%)13Source: Greenslade et al 1993.Average Total Patient Stay forVacuum Aspiration vs. D&CKenya120100Sharp CurettageMVA80Time60(hours)40200Hospital 1Source: Johnson et al 1992.Hospital 2147
Average Patient Stay for VacuumAspiration vs. D&CZambiaAverage hospitalization duration:UTH (full-time MVA service)0.6 daysNdola (sporadic MVA service)1.2 daysLivingstone (no MVA service)3.5 daysMongu (no MVA service)4.4 daysSource: PAC Needs Assessment, 199815Cost of inpatient stay for D&CChipata General HospitalAverage hospitalization duration: 5 daysFood2,500 (breakfast, lunch, dinner)Stationery1,400 (folder, paper)Cleaning mat’s1,500 (detergents)Drugs/Supplies188,500 (gentamycine, pethadine, flagyl,catheter,IV fluids, etc.)Total193,900 ZMK per patientPlus . . . Over utilization of beds, sheets, water, facilities,laundry, staff time, etc.168
Factors Contributing to the Risk ofRepeat Unsafe Abortion Lack of recognition of problem of unsafeabortion and patient FP / RH needs Lack of FP services for some groups ofwomen (e.g., adolescents, single women) Separation of emergency services frompreventive services (FP) Misinformation about which FP methodsare appropriate postabortion17Summary PAC is a life saving service Quality PAC Services require:– Prompt and safe emergency treatment with MVA, for most cases– Positive, non-judgmental staff attitudes– Psychosocial support and counseling– Proper pain management– Preventive services (i.e. family planningcounseling & services)– Linkages to other RH services189
The Situation ofPostabortion Care inZambiaObjectivesBy the end of this session, we will be ableto: Describe the health system and policyenvironment affecting PAC services inZambia Explain the weaknesses in caring forwomen with complications of pregnancyin Zambia2010
Assessment team Dr. Christine Kaseba-Sata, UTHMrs. Dorcas Phiri, General Nursnig CouncilMs. Carol Camlin, POLICY ProjectDr. Harshad Saghvi, JHPIEGOMs. Tamara Smith, JHPIEGODr. Peggy Chibuye, USAID/ZambiaMs. Michelle Folsom, USAID/REDSO/ESA21Background to the Study2211
Postabortion Care Emergency treatment services forcomplications of abortion Postabortion family planning counsellingand services Links between emergency treatmentand other RH services23Legal environment for abortion Zambia’s Termination of Pregnancy Act of1972:– abortion is permitted if continuation of pregnancyinvolves risk to the life, or injury to the physical ormental health of the woman, unborn child or thewoman’s existing children Legal abortion requires:– consent of three physicians, one of whom is aspecialist– performance by a licensed physician Illegal abortion is subject to imprisonment2412
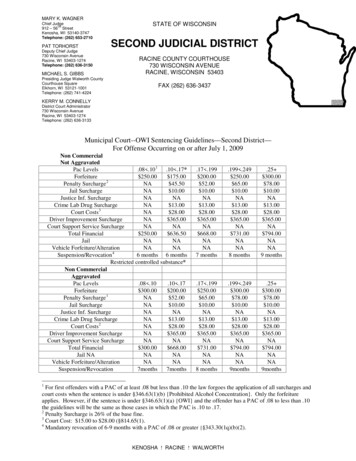
Limited access to legal abortion services Hospitals lack physicians and specialists Health care providers and administratorsoften are opposed to abortion for religiousand personal reasons Many Zambians are misinformed about theAct and its guidelines Self-induced and other illegal abortions areunsafe and frequent25Maternal deaths due to abortion13%197430%199316,000 hospital admissions foremergency cases of illegally inducedabortionsUNICEF, 19942613
Abortion complications Complications result from miscarriage andlegal abortions as well as from illegallyinduced abortions Urban and rural women of all ages seek carefor complications– young, unmarried women make up the highestproportion Emergency services are available only athospitals– demand for services at hospitals is high-42% of all emergency gynaecology admissions atUTH are due to cases of incomplete abortion27Unmet need for family planningMore than one in four married women whowant to space or limit childbearing are notusing family planning2814
Family planning use% of married womenwho use family planning26%Traditional methods15%14%Modern methods9%19921996ZDHS, 199629Women at greatest risk Rural women are 3 times less likely thanurban women to use family planning 91% of married women ages 15-19 are notusing a modern family planning method Adolescents are often excluded fromreproductive health services Limited access to quality family planningservices contributes to high abortion rates3015
Policy Environment for PAC31Health sector reform Decentralisation “Essential Package” of health servicesIssues relevant to strengthening PAC Deployment of health personnel Retraining of medical and paramedicalpersonnel in the “Essential Package”3216
Nurses and Midwives Act of 1997 Guides the education, training, monitoringand scope of work of nurses and midwives Removes legal barriers to their expanded rolein primary health care services and allowsthem to become private, independentpractitioners Allows them to play a greater role in provisionof PAC services33Postabortion Care Services3417
Limited capacity for emergency care Lower-level facilities cannot provideemergency care Delays in emergency PAC:––––staff and supply shortagesscheduling conflicts and pressure from otheremergenciesinsufficient providers skills in emergencytreatmentfacilities are unprepared to deal with acuteemergencies35MVA is not widely used or available Many physicians are unaware of theprocedure, equipment is not widely available,and sharp curettage is most often used Average hospitalization duration:UTH (full-time MVA service)Ndola (sporadic MVA service)Livingstone (no MVA service)Mongu (no MVA service)0.61.23.54.4daysdaysdaysdays3618
Infection prevention procedures vary Most sites visited have difficultyapplying infection prevention principles Decontamination is not always available Hospitals rely on central sterilizationservices which are overworked andinefficient37No links to FP and other RH services In all sites visited, PAC is not providedas a complete package FP counselling, service provision andlinkages to other reproductive healthservices are virtually nonexistent There is little pre-procedure counsellingand no counselling of patient atdischarge3819
Standards of care are not in place Specific service delivery standards andguidelines have not been incorporated intoCBOH technical guidelines There are no written standards and protocolsguiding the care of PAC patients Hospitalization is prolonged due to lack ofprotocols for seeing clients as soon as theyare admitted39Support systems & supervision are weak Service delivery infrastructure Logistics and distribution of supplies andcommodities IEC materials and strategies Information systems for monitoring & evaluation DHMTs supervise only health centres andoutposts Central/referral hospitals have no mechanism tosupervise district hospitals4020
Training in Postabortion Care41Overview Training in PAC to date has focused ondoctors’ use of MVA No linkage between emergencytreatment for abortion complicationswith the provision of FP or other RHservices No links between training andsupervision4221
Medical training Interns taught MVA at UTH; no FPcounselling or links to other servicesincluded When interns are deployed outside ofUTH, they learn D&C as no MVA kits areavailable43Nurse training PAC not incorporated into preservicenursing education No formal training currently conductedin PAC counselling, FP service or links toother RH service UTH conducts unstructured on-the-jobtraining for nurses working in acutegynae ward4422
Training recommendations Strengthen training programmes fordoctors and clinical officers Develop UTH as a nationaldemonstration site Develop innovative approaches toinstitutionalise PAC training45Conclusions4623
Positive beginnings were not sustained Although all interns are trained in MVA,services still are not available outsideLusaka Focus is still on emergency care, notabortion prevention47Weak healthcare system Inadequate staff, supplies andequipment for expansion of PACactivities Lack of training in IP, FP andemergency care Weak supervision of clinical care areas Inadequate referral system4824
Fragmented approach to expansion Existing services aimed at emergencycare only Little effort made to prevent futureabortions through IEC or advocacy No systems (in training, supplies andcommodities procurement, supervisionand service delivery) to ensuresustainable services49Discriminatory attitudes and behaviors Abortion cases are often ill-treated aspatients Many providers feel that abortion ismorally wrong and withhold quality care5025
Lack of public awareness Patients often unaware of symptoms ofabortion complications, therefore theyseek care late Late care means increased risk ofserious complications or death51Limited roles of nurses and midwives Lack adequate knowledge and training inPAC and FP counselling Inadequate numbers of nursing staff meansnurses don’t have enough time to offeradditional attention to PAC clients Since nurses are not yet authorised toperform MVA, emergency PAC services arerestricted to facilities with doctors5226
National PAC TaskforceAction Plan–––––––––Clinical Training Network &Expansion of PAC ServicesObjectivesBy the end of this session, we will be ableto: Discuss the national action plan forexpanding PAC services Explain how this activity, and our owninstitutions, fit into this overall program5427
Three Phase ExpansionI.Establish quality clinical training sitesat 3 referral hospitalsII. Establish quality clinical training sitesat 9 Provincial HospitalsIII. Establish quality PAC services atdistrict hospitals55I. Establish quality clinical trainingsites at 3 referral hospitals Advocate and develop support at national level(completed) Identify national training sites (completed) Orient hospital management and staff (completed) Prepare hospital (PAC organization within the facility,supply of necessary drugs, supplies, equipment, etc.)(completed) Strengthen underlying skills and services (infectionprevention, FP counseling & method provision, etc.)(completed)5628
I. (continued) Provide follow-up Support (completed) PAC Standardization (completed) Provide follow-up support to help establishmodel PAC services (completed) Train trainers in Clinical Training Skills(completed) Co-teach first PAC courses (See Below –training of provincial hospital teams)57II. Establish quality clinical trainingsites at 9 Provincial Hospitals Orient and secure support of PMO andDHMT Orient hospital management and staffand identify key staff Prepare hospital (PAC organizationwithin the facility, supply of necessarydrugs, supplies, equipment, etc.)5829
II. (continued) Strengthen underlying skills andservices (infection prevention, FPcounseling & method provision, etc.) Train PAC teams at one of the threeestablished training sites Follow-up support to help establishmodel PAC services Train PAC teams in clinical training skillsCo-teach first PAC courses (See Below –training of district hospital teams)59III. Establish quality PAC services atdistrict hospitals Orient and secure support of DHMT andhospital management teams Identify appropriate and interested hospitalsOrient hospital management and staff andidentify key staff Prepare hospital (PAC organization within thefacility, supply of necessary drugs, supplies,equipment, etc.)6030
III. (continued) Strengthen underlying skills andservices (infection prevention, FPcounseling & method provision, etc.) Train PAC teams at one of the 12established training sites Follow-up support to help establishquality PAC services61II. Establish quality clinical trainingsites at 9 Provincial Hospitals6231
Activity 2.01 Orient and secure support of PMO,DHMT, hospital management Conduct a one-week orientation andskills building workshops for PMO,DHMT and hospital management teammembers632.01 Outputs: 9 PMOs, DHMTs, and hospitalmanagement teams oriented to PAC Strengthened capacity developed tosupport the PAC expansion Support and coordination mechanismsestablished6432
Activity 2.02 Visit provincial hospitals to orient themanagement and staff Outputs:– 9 Provincial Hospitals supportive ofproviding quality PAC services– Plans developed for preliminarystrengthening prior to PAC training– Hospital staff to implement PAC servicesand training identified65Activity 2.03 Ensure that the necessary steps aretaken to prepare the hospital Outputs:– 9 Provincial Hospitals with adequateequipment, commitment to providenecessary medicines and supplies, andorganized to provide quality PAC services6633
Activity 2.04 Strengthen underlying skills andservices at the selected hospitals Outputs:– 9 Provincial Hospitals prepared to initiatequality PAC services, using quality infectionprevention practices, able to provide PAC,FP counseling and services, and integratedRH counseling with linkages to other RHservices on the ward as part of PAC serviceprovision67Activity 2.05 Train PAC teams in PAC services at oneof the three established training sites Outputs:– PAC teams from 9 provincial hospitalstrained in PAC services6834
Activity 2.06 Provide follow-up support to helpestablish model PAC services Outputs:– 9 provincial hospitals providing quality PACservices69Activity 2.07 Train PAC teams in clinical training skills Outputs:– Training teams from 9 sites prepared tooffer quality clinical training– 27 candidate PAC clinical trainers7035
Activity 2.08 Co-teach first PAC courses at ProvincialHospitals Outputs:– Training teams from 9 provincial hospitalscompetent in PAC clinical training– 27 qualified PAC clinical trainers71III. Establish quality PAC services atdistrict hospitals7236
Summary Expansion to the provincial level:– Establish quality PAC services– Develop training capacity Thorough preparation, orientation, andcollaboration with local management isa significant investment of the program73Roles and Responsibilitiesat National, Provincial, &District Levels in PACExpansion37
ObjectivesBy the end of this session, we will be ableto: Describe the role of National, Provincialand District level partners and theirinteraction List the key responsibilities for each ofour own institutions75National Level Guidelines and protocols for PAC Development of training system (materials,training sites, trainers) Coordinate expansion programs Advocate among stakeholders at the Nationallevel for funding and support Support Provincial and District level Overall monitoring / supervision / evaluation Feedback7638
Provincial Level Prepare expansion plans on Provincial level(coordinating among Districts) Ensure logistics – equipment & supplies (ensuredistricts are planning & budgeting appropriately) Collaborate with stakeholders for funds andlogistic support at the Provincial level Ensure Quality of Care – incorporate PAC intoquality assessment visits to all districts Monitoring, supervision & evaluation at theProvincial level (coordinating among districts)77District Level Plan for introduction of PAC within theDistrict Site assessment and preparation Support for site strengthening Ensure appropriate, adequate manpower Provision of quality, emergency PACservices on demand Outreach and linkages throughout thedistrict to improve access and referrals7839
District Level (cont.) Assure preventive services (immediateFP counseling and services on-site) Integration of other RH services withPAC (HIV/AIDS, STI, cervical cancerscreening, infertility, etc.) Ensure sustainability: budget forequipment and supplies, manpower Monitoring, supervision & evaluationwithin the District Reporting to the Provincial level and theNational Task Force79Conclusion National, Provincial & District levelseach have responsibilities These areas overlap, so there is needfor coordination and communication Through teamwork we can develop andsustain good quality PAC services8040
PAC Training & Supervision–––––––––Orientation to theIndividualized TrainingApproach and MaterialsObjectivesBy the end of this session, we will be ableto: Explain the training & supervisionapproach Describe the training and supervisionmaterials Discuss the realities from the field8241
Individualized Training On-The-Job-Training (OJT) Training small groups Competency-based & Performanceoriented83Why an Individualized Approach? Case load constraints Flexible, efficient, effective Practical8442
Learning Package Development Initiated in Nairobi in November 1999 Regional– Zambia, Kenya, South Africa, and Uganda Representative Cooperating Partners– JHPIEGO, INTRAH, IPAS, AVSC,REDSO/ESA, and USAID/Kenya85Learning Package Materials PAC Supervisor’s GuidePAC Trainer’s GuidePAC Trainee’s GuidePAC Reference ManualVideosAnatomical models8643
Key Players TraineesTrainersSupervisorsCentral level (PAC Task Force)Training site managementPAC service site management87Approach to Expansion Decentralize– Establish provincial training sites andcapacity Emphasize quality of care– IP, Counselling, Prompt & ComprehensiveCare Progressive Expansion Teamwork8844
Supervisor’s Role Establish, support & monitor trainingsites Identify potential PAC service sites– Orient administration and staff– Ensure basic quality services– Organize / coordinate training89Supervisor’s Role(cont.) Facilitate and Supervise Training– Supervise training & ensure competency Provide supportive supervision– To establish PAC Services– Continual support and monitoring of quality9045
Summary The decentralized, individualized approachdepends on:– Teamwork– Individual commitment to quality Supplies & equipment Manpower: skilled, consistent Basics: IP, interpersonal communication, etc. Comprehensive services: emergency care,counselling, FP, linkages to other RH91Integrating Family Planning& Reproductive HealthServices into PAC46
What is integration?Integration is the provision of two ormore types of services, which werepreviously provided separately, as asingle, coordinated and combined service93ObjectivesBy the end of this session, we will be ableto: Justify the need for providing FPservices on the ward Explain the value of integrating andlinking other RH services to PACservices9447
Why integrate? Ability to prevent future healthproblems (e.g., FP for PAC patients) Improvement of quality of service More efficient and cost-effective service No missed opportunity to meet clients’RH needs Convenient for the client Components of RH are interrelated95Importance of Starting PostabortionFP ImmediatelyFP is a preventive service for PAC clientsIncreased risk of repeat pregnancy:– Ovulation may occur by day 11 postabortion– 75% of women will have ovulated within 6weeks postabortionSource: L#hteenm#ki 1993; L#hteenm#ki et al 1980.9648
Which FP Methods to Use PostabortionAll modern methods are acceptable if:– Thorough counseling is given to ensurevoluntary acceptance and choice– Clients are screened for precautions97FP Methods for PAC Oral Contraceptive PillsInjectablesCondomsIntrauterine DevicesImplantsFemale Sterilization / VasectomyPeriodic Abstinence( )( )( )( )( )( )(– –) can be provided immediately at any PAC service site can be provided immediately, but require trained staff appropriate only if the woman / couple is sure of their choice, but may not be available immediately– – not appropriate until menstrual cycle regularizes9849
Integration of FP with PAC – what doesit take? Training ward staff in FP counselling andmethod provision Ensuring that FP counselling and methodsare always available, in the emergencycare setting (i.e., on the ward) Establishing clear protocols for FP followup after initial supply (e.g., an effectivereferral system to a FP clinic)99To ensure correct and continueduse:Systematic follow-up and information,education and communication arenecessary whenever a family planningmethod is supplied.10050
Examples of Other Linked RH Services HIV counseling, referral for VCT Treatment of sexually transmitted diseases(STDs) Cervical cancer screening for women over age30B35 Infertility services Pre-pregnancy advice (e.g., nutrition,immunization, management of existingmedical conditions)101Summary Quality services are comprehensive FP is a preventive service for many PACclients to prevent repeat abortions Some PAC clients want to get pregnant,and have suffered a miscarriage and mayneed help or guidance Some patients may only come in contactwith the health care system during anemergency, so it is a rare opportunity forthem and the health provider10251
Infection Prevention (IP)ObjectivesBy the end of this session, we will be ableto: Explain proper IP practices andprocedures Justify and support the need to improveIP practices to protect staff and clients10452
Objectives of Infection Prevention: To prevent major postoperativeinfections when providing surgicalcontraceptive methods To minimize the risk of transmittingserious infections (e.g., HBV, HCV,HIV/AIDS) from or to:– clients– service providers– other staff, including cleaning andhousekeeping personnel105IP PrinciplesStandard Precautions: Consider every person (client or staff) infectious Wash hands C the most practical procedure forpreventing person to person transmission Wear gloves before touching anything wet C brokenskin, mucous membranes, blood, body fluids,secretions or excretions C or soiled instruments andother items Use other physical barriers including personalprotective equipment (PPE) – such as protectivegoggles, face masks and aprons – if splashes andspills of blood, body fluids, secretions or excretionsare anticipated10653
IP Principles(cont.) Use safe work practices:– Not recapping or bending needles– Safely passing sharp instruments– Properly disposing of medical waste Process instruments and other items(decontaminate, clean, high-leveldisinfect or sterilize) using recommendedinfection prevention (IP) practices107IP Principles(cont.) In addition to the standard precautions,use transmission based precautions onlyfor patients known or suspected to beinfected with highly transmissible diseasespread by:– Airborne transmission (e.g., tuberculosis,measles, varicella)– Droplet transmission (e.g., influenza,mumps, rubella)– Contact transmission (e.g., hepatitis A,Staphylococal furunculosis, herpes simplex)10854
Risk of Disease TransmissionSource ofexposureSkin puncture(broken skin)MucocutaneousHBV(%)27S37HIV(%)0.3S0.4S 0.1As little as 10-8 ml (.00000001 ml) of HBVinfected blood can transmit HBV to asusceptible hostSource: Gerberding 1995; Seelf 1978; Bond et al 1982.109Reducing the Risks of DiseaseTransmissionBetween clients and staff:– Hand hygiene– Personal Protective Equipment (PPE) suchas gloves and clothing (worn by serviceproviders and cleaning staff)– Proper handling and disposal of sharps11055
Reducing Risks(cont.)From contaminated objects:– Processing instruments and other items Decontamination (staff) Cleaning (clients and staff) Sterilization (clients and staff) High-level disinfection (clients and staff)– Proper waste disposal (staff and community)– Encouraging appropriate IP practices in thecommunity (not reusing cutting implements orneedles, properly disposing of wastes, etc.)111Hand Hygiene Techniques Handwashing Hand antisepsis Waterless handrub Surgical scrub11256
HandwashingPurpose: Mechanically remove soil anddebris from the skin and reduce number oftransient microorganismsHandwashing may be the single mostimportant procedure in preventinginfection113HandwashingSteps:– Thoroughly wet hands– Apply a handwashing agent– Vigorously rub all areas of hands and fingers for10B15 seconds, paying close attention to fingernailsand between fingers– Rinse hands thoroughly with clean running waterfrom a tap or bucket– Dry hands with a dry clean towel or air dry them– Use a paper towel when turning off water if there isno foot control or automatic shut offSource: Larson 1999.11457
HandwashingWhen:– Before and after examining any client (directcontact)– After removing gloves, because gloves mayhave holes in them– After exposure to blood, body fluids,secretions and excretions – even if gloveswere worn115Hand AntisepsisPurpose: Remove soil and debris and reduceboth transient and resident flora on the handsSteps:– Similar to plain handwashing except that it involvesuse of an antimicrobial agent instead of plain soap ordetergentWhen:– Before performance of invasive procedures (e.g.,placement of an intravascular catheter)Source: Larson 1999.11658
Waterless HandrubPurpose: Inhibit or kill transient & resident floraIf hands are not visibly dirty, use an alcohol-basedwaterless preparationSteps:– Apply enough alcohol-based rinse or foam to coverthe entire surface of hands and fingers– Rub the preparation vigorously into hands until dry(approximately 30 seconds)When:– Same as handwashing– Following surgical scrub117Surgical HandscrubPurpose: Mechanically remove soil, debris, & transientorganisms & to reduce resident flora during surgical procedureSteps:– Remove rings, watches and bracelets– Thoroughly cleanse hands and forearms to the elbows– Clean nails with a nail cleaner– Rinse thoroughly– Apply 3 to 5 ml of antimicrobial agent– Vigorously scrub all surfaces of hands, fingers & forearms for at least2 minutes– If a sponge or a soft brush is used it should be discarded after useor processed before reuse– Rinse hands and arms thoroughly, holding hands higher than theelbows– Keep hands up and away from the body, do not touch anycontaminated surface or article, and dry with a sterile towel11859
Surgical Handscrub with WaterlessAlcohol-Based PreparationSteps:– Wash hands and arms with soap/detergentand water– Clean fingernails thoroughly– Dry hands thoroughly– Follow manufacturers’ instructions regardingapplication of alcohol preparation– Use enough alcohol for fingers, hands, andforearms, and rub for at least 20 seconds119Alcohol-Based Waterless Preparationfor Handrub and Surgical Handscrub Add 2 ml glycerine to 100 ml 60-90% alcoholsolution Apply 3 to 5 ml and continue rubbing thesolution over the hands, covering all surfaces,until dry Repeat the application a second time12060
Skin Preparation Prior to SurgicalProceduresPurpose – To minimize the number ofmicroorganisms on the skin or mucousmembranes by:– Washing with soap and water– Applying an antiseptic121Skin and Mucous MembranePreparation Do not shave hair at the operative site (ifnecessary, trim hair close to skin surfaceimmediately before surgery) Ask the client about allergic reactions beforeselecting an antiseptic solution Wash first with soap and water if visiblysoiled Apply antiseptic starting from the operativesite and working outward in a circular motionfor several inches12261
Cervical and Vaginal Preparations Apply antiseptic solution liberally to thecervix (2 or 3 times) and then to vagina– It is not necessary to prep the externalgenital area if it appears clean.– If heavily soiled, it is better to have theclient wash her genital area thoroughlywith soap and water before starting theprocedure123Personal Protective Equipment
Legal environment for abortion Zambia's Termination of Pregnancy Act of 1972: - abortion is permitted if continuation of pregnancy involves risk to the life, or injury to the physical or mental health of the woman, unborn child or the woman's existing children Legal abortion requires: - consent of three physicians, one of whom is a