Transcription
2664 3369 27GFR–MDRD (mL/mim)65 2160 3658 27Systolic blood pressure (mm Hg)128 14128 19128 15Heart rate (beats/min)76 1382 1681 12Ejection fraction (%)44 1342 1445 10Preexisting condition(s)MedicationClinical and laboratory evaluation(s)Values are presented as n (%) or mean standard deviationACE angiotensin converting enzyme, ARB angiotensin receptor blockers, BUN blood urea nitrogen, GFR glomerularfiltration rate, HFpEF heart failure with preserved ejection fraction, MDRD modification of diet in renal disease, NYHANew York Heart Association
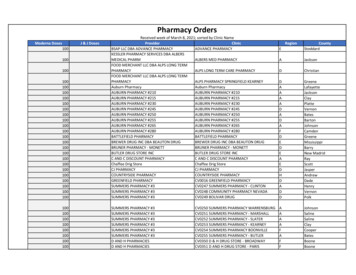
Adv Ther (2015) 32:971–982977Table 2 Clinical parameters and renal metrics at different furosemide dosages in the study populationsParametersSBP (mm Hg)HR (beats/min)Serum sodium(mEq/L)Group 1 (125 mg) (N 5 14)Group 2 (250 mg) (N 5 13)Group 3 (500 mg) (N 5 13)NormalsalineHypertonicsalinePNormalsaline128 14117 140.04 128 1976 1372 90.3140 30.4141 382 16138 3HypertonicsalinePNormalsalineHypertonicsalineP119 160.2128 15118 100.0573 130.181 1268 70.003141 20.32140 20.05 140 3BUN (mg/dL)64 2660 230.664 3279 290.269 3587 330.19Creatinine(mg/dL)1.1 0.41.0 0.40.51.2 0.51.2 0.311.2 0.41.4 0.40.21Values are presented as mean standard deviation. Normal saline (0.9%) and hypertonic Saline (1.4%). BUN blood ureanitrogen, HR heart rate SBP systolic blood pressurewere in New York Heart Association (NYHA)class IV; the mean age of patients in group 2of furosemide of between 27% and 36% and inthe total sodium excretion of between 16% and(250 mg) was 80 8.1 years, 15% were male, 5(38%) had HFpEF, and 84% were in NYHA class29% when HSS was added. An increase in 24-hurine output of between 14% and 18%IV; the mean age of patients in group 3compared to baseline was also observed.(500 mg) was 73 12 years, 54% were male, 6(46%) had HFpEF, and 69% were in NYHA classSimilar behavior was observed for total urinaryosmolality (Table 3). The link betweenIV. There were no substantial differencesbetween the groups, neither in CHF etiologyfurosemide release and natriuretic response isshown in Fig. 3. Each point represents thenor in the different types of medical therapy. Allmedian of one urine collection period and thepatients were receiving treatment withfurosemide orally, overall 45% had severecurve encompassed the time course of the entirestudy (24 h). In approximately 85% of curves,lower limb edema, and 43% had a reducedLVEF. No significant differences in serumthe software assigned a good P value (P[0.05)indicating the quality of the curve. In allsodium,nitrogengroups, the median of furosemide plus HSS(BUN), systolic blood pressure (BP), and heartrate (HR) were found between the groupsshows a dose–response curve up and to the leftwhile the median dose response curve obtained(Table 2). Total furosemide excretion, urinaryosmolarity, urinary sodium, and 24-h diuresis inwith furosemide plus normal saline is down andon the right.creatinine,bloodureathe study population after furosemide plus HSSadministration in comparison with furosemideplus normal saline baseline are presented inDISCUSSIONFig. 2. The addition of HSS to furosemide doseimproved total diuresis, urine osmolarity,The amount of drug reaching the renal tubule isallthe most important determinant of theresponse to a diuretic [26]. The drug can begroups. There was an increase in the excretionquantified by the ratio of sodium excretionfurosemide,andsodiumexcretionin
Adv Ther (2015) 32:971–982978(A)(C)(B)(D)Fig. 2 Changes in a furosemide excretion, b 24-h diuresis, c urinary sodium, and d urinary osmolality in all patients treatedat different furosemide dosages (mean SD). FUR furosemide, HSS hypertonic saline solutionrelative to urinary diuretic concentration [27].Glomerular filtration rates are relatively normalThe relationship between excretion of sodiumand urine furosemide delivery was representedin most patients with CHF but their renal bloodas a curve encompassing the time course of theflow is reduced [28]. Since furosemide gainsaccess to its intraluminal site of action by activeentire study, fitted as a sigmoid function. Toexplain these data, we assumed that the effect ofsecretion at the proximal tubule, a decreasedblood flow could limit delivery to the secretorythe infusion of HSS has realized a dual actionthat would justify the observed variation of thesite. Consequently, patients with CHF may notexcretion pattern of sodium and furosemide,respond because of reduced delivery of diureticto the site of action. The present study suggestsand, therefore, the shift of the dose–responsecurve at the top and to the left, with athat furosemide tubular delivery increases overtime in all groups but a higher furosemidecloser-to-physiology pattern. The shift at thetop of the curve intuitively reflects the increasedconcentration is observed when HSS is added.urinary sodium observed in the whole study
103.8 (20)753.94650.13171.4 (34)678.98507.59236.8 (45)observation that urinary osmolarity, urinarysodium, and 24-h diuresis were higher at alldosages of diuretic administration when HSSwas added is the consequence of majorfurosemide and sodium excretion. Suchconsequenceswereprobablyduetothefavorable diuretic effects of HSS that modifiedpharmacokinetics and pharmacodynamics offurosemide. In fact, due to its osmotic effect,HSS causes a fast and instantaneousmobilization of fluids from the third space tothe vascular compartment, without a significantsimultaneous rising of serum sodium. HSSexerts its positive effects in the kidney actingas a sort of ‘‘bait’’ for the action of the diureticby facilitating its action with a twofold effect[29, 30]. Intuitively, these results are reliablewith an increase in effective kidney bloodvolume that leads to an explanation for thequantitative and qualitative variations of urine.Another explanation may consist in thefunctional attitude of the kidney that changesin response to a load of sodium and water. Deepnephrons, due to their well-developed loops ofHenle, are more efficient in the reabsorption of757.8water and sodium (salt-saving nephrons) whilesuperficial nephrons due to their shortdeveloped loops of Henle are more efficient in521.053.933.450.36 (14)2.562.532.980.45 (18)2.92386.11334.22258.90255.48329.7674.3 (29)320.3361.4 (24)77,957.788509.6 (36) 59,092.07and sodium occurring after administration ofHSS, there is a change in the auto regulation ofthe excretion of water and sodium (salt-losingnephrons) [31]. During increased loads of waterTotal urinary osmolality(mOsm/kg)Total diuresis (L)renal plasma flow, more marked in the cortexTotal Na? excretion (mEq)31,949.113101 (27) 23,439.5614,725.0811,623.60Total furosemide ineHypertonicSalineD (%)NormalsalineHypertonicsalineD (%)Group 3 (500 mg)Group 2 (250 mg)Group 1 (125 mg)ParametersTable 3 Delta modification of total furosemide excretion, total sodium excretion, total diuresis and total urine osmolality in the study population0.48 (14)18,865 (32)population after HSS infusion. Moreover, the51.9 (16)979D (%)Adv Ther (2015) 32:971–982rather than in the renal medulla, and, as aconsequence, blood flow is increased and thefiltration rate in the superficial nephrons(salt-losing nephrons) is also increased [31].The present investigation shows that thebeneficial effects of HSS evidenced in previousstudies [8–12, 15, 16] are supported by the fact thatHSS administered in conjunction with furosemide
Adv Ther (2015) 32:971–982980(A)3 Relationship between the delivery of furosemideand natriuretic response in patients treated withfurosemide and furosemide plus HSS. Curves show thebehavior of each patient in response to the two treatments.a Median of 14 patients treated with 125 mg furosemide(whole line) and 125 mg furosemide plus HSS (dashedline). b Median of 13 patients treated with 250 mgfurosemide (whole line) and 250 mg plus HSS (dashedline). c Median of 13 patients treated with 500 mgfurosemide (whole line) and 500 mg furosemide plus HSS(dashed line). Fu furosemide, HSS hypertonic salinesolutionb Fig.pathophysiological basis for the management of(B)decompensated refractory CHF. Moreover, thesedata, if confirmed, add new insights inunderstandingmechanismsofdiureticadministration in patients with CHF.ACKNOWLEDGMENTSNo funding was received for this study. Thearticle processing charges and the open accessfee were funded by the authors. All namedauthors meet the International Committee ofMedical Journal Editors (ICMJE) criteria ty for the integrity of the work as awhole, and have given final approval for theversion to be published.Disclosures. Salvatore Paterna, Francesca DiGaudio, Vincenzo La Rocca, Fabio Balistreri,Massimiliano Greco, Daniele Torres, UmbertoLupo, Giuseppina Rizzo, Pietro di Pasquale,Sergio Indelicato, Francesco Cuttitta, JavedButler, and Gaspare Parrinello have no conflictof interest to declare and no relationship withindustry.improves diuretic and sodium excretion rate, andsubsequently shifts the furosemide dose–responsecurves up and to the left. These data suggest thatthis approach is effective, and may be adopted intoroutine care and should serve as a newCompliance with ethics guidelines. Protocolwas carried out following the principles of theHelsinki Declaration of 1964, and subsequentrevisions, and in accordance with national
Adv Ther (2015) 32:971–982981legislations. The hospital’s Internal ReviewBoard and its Ethics Committee approved theprotocol and all patients signed a writteninformed consent.Open Access. This article is distributedunder the terms of the Creative CommonsAttribution-NonCommercial 4.0 InternationalLicense (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercialuse, distribution, and reproduction in anymedium, provided you give appropriate creditto the original author(s) and the source, providea link to the Creative Commons license, andindicate if changes were made.REFERENCES1.2.3.Gheorghiade M, Filippatos G, De Luca L, Burnett J.Congestion in acute heart failure syndromes: anessential target of evaluation and treatment. Am JMed. 2006;119(12 suppl 1):S3–10.Felker GM, Mentz RJ. Diuretics and ultrafiltration inacute decompensated heart failure. J Am CollCardiol. 2012;59:2145–53.Valente MAE, Voors AA, Damman K, et al. Diureticresponse in acute heart failure: clinicalcharacteristics and prognostic significance. EurHeart J. 2014;35(19):1284–93.4.Kramer BK, Schweda F, Riegger GA. Diuretictreatment and diuretic resistance in heart failure.Am J Med. 1999;106:90–6.5.Brater DC. Pharmacokinetics of loop diuretics 40–3.6.Dormans T, Gerlag P, Russel F, et al. Combinationdiuretic therapy in severe congestive heart failure.Drugs. 1998;55:165–72.7.Brater DC, Chennasasin P, Seiwell R. Furosemide inpatients with heart failure. Shift of the doseresponse relationship. Clin Pharmacol Ther.1980;28:182–6.8.Paterna S, Parrinello G, Amato P, et al. Tolerabilityand efficacy of high-dose furosemide and small 17volume hypertonic saline solution in refractorycongestive heart failure. Adv Ther. 1999;16:219–28.9.Paterna S, Parrinello G, Amato P, et al. Smallvolumehypertonicsalinesolutionandhigh-dosage furosemide in the treatment ofrefractory congestive heart failure. A pilot study.Clin Drug Invest. 2000;19:9–13.10. Paterna S, Di Pasquale P, Parrinello G, et al. Effectsof high-dose furosemide and small volumehypertonic saline solution infusion in comparisonwith a high dose of furosemide as a bolus, inrefractory congestive heart failure. Eur J Heart Fail.2000;2:305–13.11. Licata G, Di Pasquale P, Parrinello G, et al. Effects ofhigh-dose furosemide and small-volume hypertonicsaline solution in comparison with a high dose offurosemide as bolus in refractory congestive heartfailure: long term effects. Am Heart J.2003;145:459–66.12. Paterna S, Di Pasquale P, Parrinello G, et al.Changes in brain natriuretic peptide levels andbioelectrical impedance measurements aftertreatment with high-dose furosemide andhypertonic saline solution versus high-dosefurosemide alone in refractory congestive heartfailure. J Am Coll Cardiol. 2005;45:1997–2003.13. Gandhi S, Mosleh W, Myers RB. Hypertonic salinewith furosemide for the treatment of acutecongestive heart failure: a systematic review andmeta-analysis. Int J Cardiol. 2014;173(2):139–45.14. Ventrella F, Cappello S, Minafra G, et al. Hypertonicsaline solution and high-dose furosemide infusionin cardiorenal syndrome: our experience. Ital J Med.2012;6:91–8.15. Tuttolomondo A, Pinto A, Parrinello G, Licata G.Intravenous high-dose furosemide and hypertonicsaline solutions for refractory heart failure andascites. Semin Nephrol. 2011;31(6):513–22.16. Tuttolomondo A, Pinto A, Di Raimondo D, et al.Changes in natriuretic peptide and cytokine plasmalevels in patients with heart failure, after treatmentwith high dose of furosemide plus hypertonic salinesolution (HSS) and after a saline loading. NutrMetab Cardiovasc Dis. 2011;21(5):372–9.17. Miller WL, Borgeson DD, Grantham JA, Luchner A,Redfield MM, Burnett JC Jr. Dietary sodiummodulation of aldosterone activation and renalfunction during the progression of experimentalheart failure. Eur J Heart Fail. 2015;17(2):144–50.18. De Vecchis R, Ciccarelli A, Ariano C, et al.Renoprotective effect of small volumes ofhypertonic saline solution in chronic heart failure
Adv Ther (2015) 32:971–982982patients with marked fluid retention: results of acase-control study. Herz.
patients with chronic heart failure (CHF) is better assessed by urine production per unit diuretic dose than by the absolute urine output or diuretic dose. Diuretic resistance arises over time when the plateau rate of sodium and water excretion is reached prior to optimal fluid elimination and may be overcome when