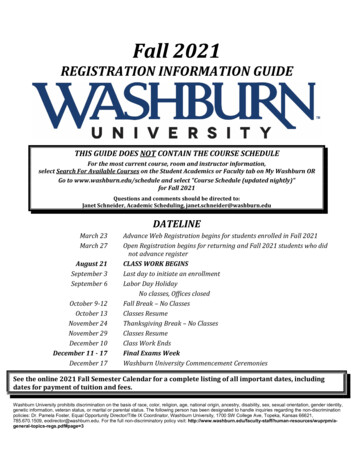
Transcription
SPRING 2021ACQAADVISOR2Clinical Corner3Back Pain4Preoperative Testing5PharmacyBenefit CheckACQA Advisor is a quarterlynewsletter dedicated to sharingnews, updates and best practiceswith our ACQA partnersA nonprofit independent licensee of the Blue Cross Blue Shield Association
Clinical CornerNow that I have had the chance to really start working with ourvalue-based teams, it is wonderful to get to know you and tobe a part of some truly collaborative relationships. But, as theCOVID-19 pandemic has continued to put stress on all in thehealth-care system and create challenges for so many, I havehad to stop at times and wonder – how important are thesevalue-based relationships and programs right now?The more I began to think about it, the more I realized that whatwe are doing is perhaps even more important and timely thanwe previously thought. What we have witnessed with thepandemic has exposed the vulnerability and unsustainabilityof the traditional fee-for-service model, and the advantages ofvalue-based model concepts.A colleague leading a very large health system once said,“We are in two basic businesses in health care – the businessof keeping people well, and the business of taking care of themwhen they get sick.” Health care providers can intervene at bothpoints, and at any point in between. Sometimes it is the inbetween points that can have the greatest impact. What we areoften trying to do together in our ACQA relationships is to identifyinnovative ways to intervene at earlier stages – or even beforesomeone becomes sick – to improve quality of care, improveoutcomes, and reduce cost.In the past few years, Medicare has been moving toward valuebased care, “bending the cost curve,” and rewarding “qualityover quantity.” The hope is that, by 2025, nearly all Medicarereimbursement will be tied to value-based arrangements. Thepandemic is likely to accelerate this timeline. What we do togetherfor our communities will help better position each of you to beready to expand these initiatives to the entire patient populationyou serve.Nicholas Massa, M.D.Interim Vice President, Medical Affairs“We are intwo basicbusinesses inhealth care –the business ofkeeping peoplewell, and thebusiness oftaking care ofthem whenthey get sick.”COVID-19 has created challenges we couldn’t have imagined,impacting health care on so many levels. Our work in theACQA arena is more important than ever. Let us not forgetthat this collaboration is truly valuable for what we are tryingto accomplish together and will help us prepare for thecoming landscape.2
Primary Care Decisionsfor Acute Low Back PainMay Trigger Chronic PainLow back pain (LBP) is the leading cause of disabilityand leading cost to society1, 2. It typically is also thebiggest health care expense of local employer groups.Primary care is widely seen as the key to efficientand effective health care in general3, but has provento be problematic when it comes to LBP. This hasbeen highlighted in two prestigious journal articlespublished in the last few months.Kamper et al4, in a systematic review published in thejournal Pain, found that only approximately 20% ofprimary care practitioners follow the recommendedapproaches of evidence-based LBP guidelines.That means four out of five patients are not gettingevidence-based direction early in their care journey.There is significant opportunity in spinal care toimprove outcomes and prevent harm just by adoptingevidence-based care.and depression) for transitioning from acute LBP tochronic LBP. In fact, unnecessary imaging, prescribingof opioids and early specialty referrals were themost powerful predictors of who would become achronic back pain sufferer. The health care system isinadvertently triggering the development of chronicback pain!The data shows that only a small number ofpractitioners follow evidence-based guidelineswhen dealing with back pain patients. And, if thepractitioner’s treatment approach runs contrary torecommended guidelines, not only is the patientunlikely to be helped, there is an increase in thelikelihood that he/she will become a chronicLBP sufferer.The clinician’s early care decisions can actually triggerthe evolution of chronic pain. In a groundbreakingJournal of the American Medical Association articlepublished in February, Stevans et al 5 sought toidentify the key factors that contribute to a patient’sacute LBP becoming chronic. An assessment of morethan 5,000 acute LBP primary care patients identifiedseveral factors, including smoking, obesity anddepression, to be associated with transition to chronicLBP. This verified previous studies.Primary care has been provided with several highquality LBP guidelines, but evidence is clear that thisis not enough to bring about improvement. What isneeded is an expanded support system framed in acare pathway that includes easily applied tools andactive collaboration, as is offered by the ExcellusBlueCross BlueShield Spine Health Program. Oursimple 2-hour evidence-based, on-line spine pathwayworkshop has shown to decrease inappropriateimaging, opioid use and specialist referrals whileachieving high provider satisfaction scoresfrom attendees.However, it was also found PCP care not supportedby evidence-based guidelines to be an independentrisk factor (i.e., controlling for smoking, obesityTo register for the pathway training, which provides 2free CMEs, go to: -registration/For further information, please contact brian.justice@excellus.comHoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study.Annals of the rheumatic diseases. 2014 Jun;73(6):968-74.² Dieleman JL, Cao J, Chapin A, Chen C, Li Z, Liu A, et al. US Health Care Spending by Payer and Health Condition, 1996-2016. Jama. 2020 Mar 3;323(9):863-84.³ Phillips RL, Jr., Bazemore AW. Primary care and why it matters for U.S. health system reform. Health affairs. 2010 May;29(5):806-10. PubMed PMID:20439865. eng.⁴ Kamper SJ, Logan G, Copsey B, Thompson J, Machado GC, Abdel-Shaheed C, et al. What is usual care for low back pain? A systematic review ofhealth care provided to patients with low back pain in family practice and emergency departments. Pain. 2020 Apr;161(4):694-702.⁵ Stevans JM, Delitto A, Khoja SS, Patterson CG, Smith CN, Schneider MJ, et al. Risk Factors Associated With Transition From Acute to Chronic LowBack Pain in US Patients Seeking Primary Care. JAMA Netw Open. 2021 Feb 1;4(2):e2037371.13
Consider Needfor PreoperativeTestingin Low-Risk ProceduresAlthough we are all still dealing with the COVID-19pandemic, we continue to examine ways to addressvariations in care. Our research has identified variationin preoperative testing for low risk procedures.Given this fact, we want to provide the followinginformation as food for thought prior to orderingpreoperative testing.Society of General Internal Medicine: “Don’tperform routine pre-operative testing beforelow-risk surgical procedures.”American College of Surgeons: “Avoidadmission or preoperative chest X-rays forambulatory patients with unremarkable historyand physical exam.”American Academy of Family Physicians:“Don’t order annual electrocardiograms orother cardiac screening for low-risk patientswithout symptoms.”Excellus BlueCross BlueShield’s research revealedthat preoperative laboratory studies, pulmonaryfunction tests, X-rays, electrocardiograms and othercardiac studies have been performed on patients priorto low-risk procedures. Follow-up research uncoveredthe following guidelines issued by various specialtysocieties and reported by Choosing Wisely . Thesestatements are intended to spark conversationsbetween physicians and patients to ensure thatthe right care is delivered at the right time for theright reason.Our claims data uncovered testing for low-riskprocedures without a clear clinical indication andthere was variation amongst our regional facilities.We believe that the following factors could be theprobable causes of variation: Routine preoperative testing protocols/facility protocols Preoperative standing orders versus preoperativepatient-centered assessments HabitAmerican Society of Anesthesiologists: “Don’tobtain baseline laboratory studies in patientswithout significant system disease (ASAI or II),complete profiles for low-risk surgery.”As we all work together to reduce the burden on ourpatients and to keep health care affordable, I ask youto consider the following questions before orderingpreoperative testing:American Academy of Ophthalmology: “Don’tperform preoperative medical tests for eyesurgery unless there are specific medicalindications.” Is this recommended evidence-based care?American College of Cardiology: “Avoidperforming stress cardiac imaging oradvanced non-invasive imaging as apreoperative assessment in patients scheduledto undergo low-risk non cardiac surgery.”It was also recommended that routineelectrocardiography (ECG) screening as partof preoperative or preprocedural evaluationsfor asymptomatic patients undergoing low-risksurgical procedures be avoided. Is there a clinical rationale for testing? Will the test have value in the patient outcome?Our hope is to ensure that preoperative testing isguided by the patient’s medical history, physical examfindings and assessment of potential risk rather thanroutine protocol.On behalf of our members, we thank you for yourconsideration. Please stay safe and a million thanksfor everything you are doing for our members and ourcommunity during these challenging times.Richard Vienne, DOSenior Medical Director, WNYand Employer Group Support4
Real Time Benefit Check Improves Patient,Provider SatisfactionNew medications are coming tomarket faster than ever and pricesare continuously fluctuating. It isbecoming increasingly complexand time consuming for providersto choose the most appropriatemedication for their patients at thelowest cost.Leveraging the technology of apharmacy Real Time Benefit Check(RTBC) tool that is integratedinto an electronic medical record(EMR) workflow can assist withmany prescription challenges. Thegoal of RTBC is to provide clarityon medication costs, facilitatethe prescribing process, improvehealth care outcomes, and,ultimately, increase both providerand patient satisfaction.Price TransparencyWithin a RTBCtool, providerscan see real-timedrug pricing.Out-of-pocketmedication costsare available forthe prescribed drug as well as fortherapeutic alternatives. Providerscan also see if there is a differencein medication cost depending onwhether the prescription is filledat a retail or mail order pharmacy.This is especially helpful if patientsare also interested in obtaininga larger quantity of medicationthrough mail order (i.e., 90-day vs.30-day supply) but are unsure ifthey can afford the larger up-frontcost. These price transparencycapabilities allow the mostcost-effective medication to beprescribed for patients.5IncreasedAdherenceElectronic PriorAuthorization (ePA)Within a RTBC tool, providerscan see formulary coverageand any other requirements forthe medication, such as a priorauthorization (PA) or a specialtypharmacy restriction. The tool canhelp guide the provider to choosea formulary covered medicationover a non-formulary alternative.If the provider wishes to continuewith prescribing the medicationrequiring a PA, his/her EMRsystem may allow for seamlesssubmission of an electronic PArequest. The fewer exchangesnecessary between the provider,insurer and pharmacy throughoutthe prescribing process, the earlierthe patient can start treatment.Having ePA available withinan EMR facilitates the patientreceiving the most appropriatemedication as quickly as possible.RTBC:There are variousreasons patientsdo not adhere tomedications, whichcan increase overallhealth care costs drastically.Patients and prescribers oftendo not know the price or benefitcoverage of the prescribedmedication until the patient goesto the pharmacy. If a prescriptionis too costly, the patient may notpick it up at the pharmacy or maynot take as prescribed. Also, ifa patient learns the prescriptionis not covered by insurance orrequires a prior authorization,the patient may become frustratedand forgo treatment. A RTBCwith both price transparencyand ePA can help avoid thesesituations and improvemedication adherence.This tool may be available foryour EMR. Please reach out toyour ACQA team for additionalinformation.Fast FactsProviders who report using ePA instead of fax and/or phone spend2.5 hours less per weekan average ofon priorauthorization for their patients. -2018.pdf71%of providers who were considered experienced users reportedtheir patients received faster care after implementation of ePA. /
Excellus BlueCross BlueShield's research revealed that preoperative laboratory studies, pulmonary function tests, X-rays, electrocardiograms and other cardiac studies have been performed on patients prior to low-risk procedures. Follow-up research uncovered the following guidelines issued by various specialty