Transcription
USER MANUAL FOR SPIROMETRY TESTINGSlow and Forced SpirometryMaximum voluntary ventilation - Minute tidal ventilationS1-ENVersion 2.114/05/2019
Content1Foreword . 52General information . 632.1Description of test and application range . 62.2Indications . 62.3Contraindications. 7Preparation of the testing . 93.1Preparing the equipment . 93.2Preparing the patient. 103.3Encoding the patient in the database . 113.3.1If the patient already exists in the database . 113.3.2If the patient does not exist yet in the database . 123.44567Initializing the spirometry testing mode . 13Slow spirometry testing . 164.1Performing the test . 164.2Quality control . 184.3Reviewing the test . 194.4Editing the test. 20Forced spirometry testing . 215.1Performing the test . 215.2Quality control . 245.3Reviewing the test . 255.4Editing the test. 265.4.1Curves edition . 265.4.2Toolbox . 27Maximum voluntary ventilation testing . 286.1Performing the test . 286.2Quality control . 296.3Reviewing the test . 30Minute tidal ventilation testing . 317.1Performing the test . 317.2Quality control . 327.3Reviewing the test . 33S1-ENSpirometryPAGE 2/39
8Studied parameters . 348.1Slow spirometry . 348.1.1Measured parameters . 348.1.2Calculated parameters . 348.2Forced spirometry . 358.2.1Measured parameters . 358.2.2Calculated parameters . 368.3Maximum voluntary ventilation . 378.4Minute tidal ventilation . 378.4.1Measured parameters . 378.4.2Calculated parameters . 38S1-ENSpirometryPAGE 3/39
sion1.02.02.1ModificationsCreationNew designModification of the CE markingSpirometryPAGE 4/39
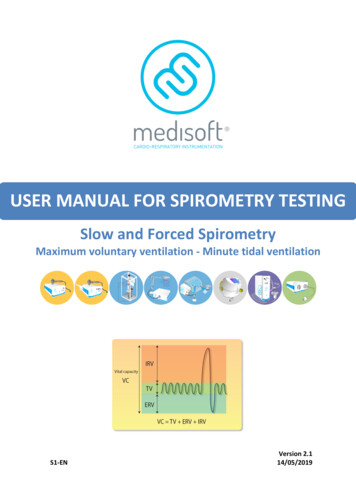
11 ForewordThis document provides instructions required to perform a spirometry test (slow and forcedexpiratory capacity measurements) on Expair.Spirometry option in Expair is a module to record and analyze the vital capacity and forcedexpiratory flow rates. The interface is friendly to use. It provides a sensible spirogramrecorder and other functions for editing and printing the result. The spirometry is a basicoption for most the Medisoft instruments (Micro 5000, Micro 6000, HypAir, SpiroAir,BodyBox), it allows to measure all the lung volumes that can be mobilized, including tidalvolume, functional reserve capacity, inspiratory capacity, vital capacity. In addition, the mostwidely used pulmonary function test: the forced vital capacity maneuver is also ensured.The purpose of this document is to help in using and putting your Medisoft equipment intoservice. Please read this manual carefully before using the equipment for the first time. Allthe necessary measurements must be taken in order to ensure safe use of the equipment.This document is based on the last version (1.32) of our Expair software. Medisoft S.A.reserves the right to modify the software or issue updates without prior notice. Therefore,some differences could exist between these directions for use and the last version of thesoftware in use. Beware that some items may be modified slightly in last version of thesoftware.S1-ENForewordPAGE 5/39
22 General information2.1 Description of test and application rangeSpirometry is a physiological measure of breath. This test aims to evaluate inspiratory andexpiratory flowrates, as well as lung volume subcomponents. Through spirometry outcomes,pulmonary function abnormalities could be classified into two mains categories: obstructiveand restrictive patterns. This clinical approach is based on the fact that the test measurestwo basic components – air flow (FEV1, FEF25-75, FEV6, ) and lung volume (SVC, FVC, IC, ). Intermediate flowrates such as FEF25% or FEF50% might also reflect the dysfunction insmall airways.Spirometry also includes two supplementary methods in which the spirometry exam isrepeated on a subject following the administration of a bronchodilator medication(reversibility testing) or stimulating agents (bronchial provocation testing), in order todistinguish COPD from asthma. This technique is totally non-invasive, therefore would notraise any question about patient safety.According to official guidelines, spirometry is the fundamental test for making a confidentdiagnosis of obstructive airways disorders (e.g. COPD, asthma) and the most effective wayfor determining the severity of lung diseases and following up. Spirometry is also a powerfultool for screening of lung diseases in epidemiological studies.2.2 IndicationsThe spirometry testing (including FVC and VC maneuvers) can be indicated:For diagnostic purposes To evaluate symptoms, signs or abnormal laboratory tests To measure the effect of disease on pulmonary function To screen individuals at risk of having pulmonary disease To assess pre-operative risk To assess prognosis To assess health status before beginning strenuous physical activity programsFor monitoring purposes To assess therapeutic intervention To describe the course of diseases that affect lung function To monitor people exposed to injurious agents To monitor for adverse reactions to drugs with known pulmonary toxicityFor disability/impairment evaluations To assess patients as part of a rehabilitation program To assess risks as part of an insurance evaluation To assess individuals for legal reasonsFor public health studies Epidemiological surveys Derivation of reference equations Clinical researchS1-ENGeneral informationPAGE 6/39
Relative contraindications for spirometry include hemoptysis of unknown origin,pneumothorax, unstable angina pectoris, recent myocardial infarction, thoracic aneurysms,abdominal aneurysms, cerebral aneurysms, recent eye surgery (within 2 weeks due toincreased intraocular pressure during forced expiration), recent abdominal or thoracicsurgical procedures, and patients with a history of syncope associated with forcedexhalation.Relative contraindicationsCerebral aneurysmRecent brain surgeryRecent concussionRecent eye surgerySignificant glaucomaMechanismsIncreases inintracranial/intraocularpressure due todecreased venousreturnRecent sinus surgery ormiddle ear surgery orinfectionPneumothoraxSignificant aortic aneurysmRecent thoracic surgeryRecent abdominal surgeryPregnancyIncreases in sinus andmiddle ear pressuresIncreases inintrathoracic and intraabdominal pressureCommentsIncreases in intraocular pressure duringweightlifting suggest spirometry testingmay lead to clinically significant changes inintraocular pressures in most patients.Most experts suggest a three- to six-weekrecovery period following surgery beforespirometry testing.There is a risk that forced maneuvers causeexcessive pain or even ear drum rupture incases of middle ear infection.Increases in intrathoracic or intraabdominal pressures may increase bloodpressure but are not expected to increaseaortic transmural pressure.Postoperative physiotherapy includingcoughing is believed to be beneficial aftercardiothoracic and abdominal surgery.Cough generally increases intrathoracicpressures up to 400 cm H2O, comparedwith 70 cm H2O – 200 cm H2O duringSystemic hypotension orsevere hypertension (e.g., 200/120 mmHg)Significant atrial/ventriculararrhythmiaNo compensated heartfailureRecent myocardial infarctionor pulmonary embolusHistory of syncope related toS1-ENIncreases inmyocardial demand orchanges in bloodpressurespirometry. The risk is likely low in mostpatients.Lung function tests may increase the risk ofearly delivery in case of cervicalincompetence.Exercise testing one week after myocardialinfarction appears to be safe. A shorterperiod could be appropriate followingreperfusion therapy (e.g., angioplasty),whereas caution is necessary in case ofpersistent myocardial ischemia.Prudence is also called in many of theseconditions with the use of ß2sympathomimetics, although the risk of asingle administration is likely to beGeneral informationPAGE 7/3922.3 Contraindications
Active tuberculosisHepatitis BHemoptysis or oral bleedingInability to follow directions(eg, confusion, dementia,young age, language barrier)S1-ENminimal.Infection control issuesGeneral infection control measures shouldbe adopted in accordance to localprocedures.In some cases, successful spirometry canbe obtained with increased coaching andaid of an interpreter.General informationPAGE 8/392forced exhalation/cough
3 Preparation of the testing33.1 Preparing the equipmentThe module should be turned on at least 20 minutes before performing thecalibration and the first test.This allows the warmup of the device.1Verify the connections of the tubing to the module.2Depending on the configuration of your device, verify the gas cylinders:2A2B2C2D3S1-ENOpen fully each gas cylinder by rotating counter clock wise the tap.Check the fill in pressure of each gas cylinder.It should be at least 20 bars (290 psi). If lower pressure, replace thecylinder.Check the output pressure of the reducer of each gas cylinder. It shouldbe set to 3.5 bars (50 psi) or 4.5 bar (65 psi) depending on your device.Check the validity date of each gas cylinder (indicated on the analysecertificate of the cylinder). Replace the cylinders which are no longervalid.Verify the device has been calibrated before in the day.Read the chapter about calibration in the Hardware User Manual.Preparation of the testingPAGE 9/39
1Measure height and weight of the patient.2Install the patient seated upright with feet firmly on the floor in front of thedevice. This is a safety precaution as the subject can become light headed duringthe test and this can promote his falling from the chair, this posture minimisesany possible risk.3Adjust the arm and patient valve to the height of the subject’s mouth in thenormal seated position. The subject’s chest frame should be undistorted and thediaphragm in a normal position.4Put a new single use barrier filter, and optionally a mouthpiece on the front ofthe pneumotachograph. Instruct the patient in the correct use of the mouthpieceand nose clip during the testing.5Instruct the patient in the performance of the test. Use simple words for him tounderstand the required maneuver.S1-ENPreparation of the testingPAGE 10/3933.2 Preparing the patient
3.3 Encoding the patient in the database3.3.1 If the patient already exists in the databaseOn the main screen of Expair, search the patient on the list.2If necessary, use the search tool in order to find the patient. Click on Search.3Encode the search criteria: last name, ID and or date of birth. Click on Find.4Check the patient details to confirm the right patient has been selected.31S1-ENPreparation of the testingPAGE 11/39
1On the main screen of Expair, click on Add.2Encode the patient details: last Name, first name, ID (facultative), gender, date ofbirth. Click on OK.3On the next screen, encode the additional patient details: physician name,predicted set or ethnia. Click on OK.S1-ENPreparation of the testingPAGE 12/3933.3.2 If the patient does not exist yet in the database
1On the main screen of Expair, verify the right patient is selected in the list.2Make sure the patient is not connected to the patient valve. This could lead to awrong zero measurement.3Activate the testing mode by following one of these 2 ways:4S1-EN3ATo create a new consultation, click on PFT button.3BTo complete an existing consultation, click on Continue button.If the patient has already performed a test that day, a window appears to verify ifyou want to complete the current test.4AClick on No to create a new consultation.4BClick on Yes to complete the existing consultation.Preparation of the testingPAGE 13/3933.4 Initializing the spirometry testing mode
The test screen appears. The zero of the pressure and flow transducers ismeasured. Make sure the patient is still not connected to the patient valve.6Complete the patient’s demographic data (at least height and weight).7Verify the ambient conditions. Correct if necessary.8Verify or encode the instrument dead space (volume of the filter in ml) and theinstrument resistance (resistance of the filter in cmH2O/L/s).9Verify all information and then click on Validate.10Select the test you want to perform.35S1-ENASlow Spirometry Select VC tab;BForced Spirometry Select FVC tab;CMaximum Voluntary Ventilation Select MVV tab;DMinute tidal ventilation Select VMIN tab.Preparation of the testingPAGE 14/39
Filter characteristics (resistance and volume) must be encoded carefully.This information is available on the package or the datasheet of the filter. Incase of any doubt, please contact your filters supplier.The resistance and the volume values of the filter have no impact onspirometry calculation, but for other pulmonary function tests such as lungvolumes or diffusion measurements.The ambient conditions are used to calculate BTPS correction factor. It isessential that ambient conditions are measured or encoded correctly foraccurate volume measurement: Temperature: in degrees Celcius Relative humidity: in % Barometric pressure: in mmHgImportant information on barometric pressureThe barometric pressure used by the software is the actual barometricpressure, not barometric pressure corrected at sea level. Be careful whenusing an external weather station because it always indicates barometricpressure corrected at sea level, depending on the altitude of the location.In order to obtain the real barometric pressure, the formula below can beused:BPreal0.0065 h 5.255) BPcorr (1 288.15Where:- BPcorr is the barometric pressure (in mmHg) corrected at sea level, asindicated on all external weather stations- h is the altitude (in meters)Example: a weather station indicates 760 mmHg at an altitude of 250 meters.This will correspond to a real barometric pressure of 738 mmHg.S1-ENPreparation of the testingPAGE 15/393Height, weight and age of the patient are used for predicting the normalvalues. It is essential that height and weight are measured and encodedcorrectly in order to have good predicting values.
4 Slow spirometry testing44.1 Performing the testS1-ENSlow spirometry testingPAGE 16/39
Click on Start to begin the test.2Verify the volume signal is perfectly horizontal.If the signal is horizontal, it means the zero of the flow transducer hasbeen measured correctly. Go to step 3.If the signal is not horizontal, it means the zero of the flow transducer hasnot been correctly measured.3458S1-EN2BVerify the patient is not connected to the valve and then click onZero in order to measure the zero of the flow transducer.2CVerify the volume signal is now perfectly stable.Ask to the patient to perform a vital capacity maneuver. Two ways are possible:5B7Click on Stop button.Ask to the patient to connect his mouth to the antibacterial filter. Verify there isno leak between his mouth and the filter.The patient breathes normally several times until the ventilatory resting level(FRC) is established.5A62AThe patient exhales fully from FRC level to RV, then inhales fully from RVto TLC.The patient inhales fully from FRC level to TLC, then exhales fully from TLCto RV.Ask to the patient to breath normally.Click on Stop to finish the test.The values are displayed in the results table, under “Test 1” column.Repeat the test at least two times in order to have at least two acceptable andreproducible tests (see 4.2 Quality control).Slow spirometry testingPAGE 17/3941
4.2 Quality control End-tidal expiratory level must be perfectly stable for the reliable calculation of thedifferent pulmonary volumes; During deep maneuver, end inspiratory and expiratory phases must reach a plateauon the volume/time curve to ensure a complete vital capacity; At least 3 maneuvers should be performed:o The difference between the two best acceptable VCs is less than 150 mL;o Make sure the patient did the greatest possible collaboration. If previous criteria are not fulfilled, let’s the patient try again with a maximum of 4repetitions.S1-ENSlow spirometry testingPAGE 18/394The quality control is based on the ATS-ERS criteria:
44.3 Reviewing the test1Select a test by clicking on the corresponding test label.2Select to show or hide the cursors (upper and lower limits on the spirogram).You can optimize manually those cursors with the spirogram editor function (seehereafter).3Use the zoom buttons to modify the size of the spirogram.4Verify the numerical values and select the best value to report.5Use these radio buttons to take a test into account for the final report. Bydefault, the software automatically chooses the best effort as the effort with thelargest VC.6Comment/interpretation editing mode.7Click on this button to see the report before printing.NOTE:The review mode is applied to current test as well as old tests. You can review, edit and printan existing test by repeating exactly the steps on above.S1-ENSlow spirometry testingPAGE 19/39
4.4 Editing the test4For editing mode, click right on the number of the test and select Edit.Toggle each of the buttons you would like to adjust (1-4) and place then your cursor onthe best upper or lower limit of volume (TV or VC) you wish to measure:1Tidal Volume upper limit (blue cursor).2Tidal Volume lower limit (red cursor).3Vital Capacity upper limit (green cursor).4Vital Capacity lower limit (black cursor).56S1-ENThe calculator button is an auto-selection of best value (set by default). Aftermanual changes of TV or VC, the calculator button restores default settings too.The “staircase” button is an auto calibration for Tidal breath cycles. It will levelout a sloping trace, when the slope is known to be caused by an instrument driftand not a true physiological shift.Slow spirometry testingPAGE 20/39
5 Forced spirometry testing55.1 Performing the testS1-ENForced spirometry testingPAGE 21/39
1Click on Start to begin the test.2Verify the volume signal is perfectly horizontal.If the signal is horizontal, it means the zero of the flow transducer hasbeen measured correctly. Go to step 3.If the signal is not horizontal, it means the zero of the flow transducer hasnot been correctly measured.Click on Stop button.2BVerify the patient is not connected to the valve and then click onZero in order to measure the zero of the flow transducer.2CVerify the volume signal is now perfectly stable.52A34Ask to the patient to connect his mouth to the antibacterial filter. Verify there isno leak between his mouth and the filter.The patient breathes normally several times until the ventilatory resting level(FRC) is established.5Ask to the patient to inhale fully, then directly after his lungs are filled.6Ask to the patient to exhale as fast as possible during at least 6 minutes(maximum 10 minutes), followed by a deep inhalation. Encourage him in order toachieve the best effort as possible.7Ask to the patient to breath normally.89Click on Stop to finish the test.The values are displayed in the results table, under “Test 1” column.Repeat the test at least two times in order to have at least two acceptable andreproducible tests (see 5.2 Quality control).Note: The vertical red line indicates when the instantaneous expiratory flow is less than0.025 L/s. This in an indication for the operator that the patient has nearly achieved aplateau in volume-time curve.S1-ENForced spirometry testingPAGE 22/39
51During the test, the screen can be refreshed at any moment with the scissors button.2Stopwatch indicating the duration of expiratory time.3Incentive mode: Medisoft has three incentive graphical formats:Flying above the trees indicates that the FEV1 and PEF is complete.Landing the plane corresponds to 6 seconds of expiration.The birthday cake is a direct measure of FEV1: when the child blows all thecandles in one second, FEV1 measurement is completed.For adults, a timer for exhaled time and a bar graph of volume effort canalso be displayed.S1-ENForced spirometry testingPAGE 23/39
5.2 Quality control5The system will check the quality of each maneuver in regard of the ATS-ERS criteria. For adetailed quality check list, click on the ATS button.1The green check means that the test is acceptable.2The red cross indicates that the test doesn’t meet the ATS-ERS criteria and mustbe rejected.3“OK” means that the criterion is fulfilled.4“OP” means that the criteria must be checked and validated by the operator.5“NO” means that the criterion is not fulfilled.S1-ENForced spirometry testingPAGE 24/39
55.3 Reviewing the test1Select manually or automatically the best values. By default the softwareautomatically selects the best effort as a combination of the best FVC, FEV1, PEFeven from different efforts.2Expiratory volume/time curve, with ‘real zero’ and end-expiratory flow criteria.3Reviewing of the ATS-ERS criteria (see 5.2).4Access to the visual interpretation feature.5Comment/interpretation editing mode.6Click on this button to see the report before printing.S1-ENForced spirometry testingPAGE 25/39
5.4 Editing the test5.4.1 Curves edition5For editing mode, click right on the number of the test and select Edit.Toggle each of the buttons you would like to adjust (1-4) and place then your cursor onthe best upper or lower limit of volume (VCE or VCI) you wish to measure:1Expiratory VC upper limit (blue cursor).2Expiratory VC lower limit (red cursor).3Inspiratory VC upper limit (green cursor).4Inspiratory VC lower limit (black cursor).5The calculator button is an auto-selection of best value (set by default). Aftermanual changes of VCE or VCI, the calculator button restores default settings too.S1-ENForced spirometry testingPAGE 26/39
55.4.2 Toolbox1Toolbox button for setting of default selections.2Mid Expiratory Flow calculation formula. The most common method is (FVC/2)divided by the time interval between F75 and F25. However, an alternative exists.3Adjustment of the flow/volume loop on the measured Residual Volume.4Display of the vertical red line when expiratory flow is lower than 25 ml/s.Another end-expiratory threshold can be edited too.5Confirm the changes in the configuration.S1-ENForced spirometry testingPAGE 27/39
6 Maximum voluntary ventilation testing66.1 Performing the testS1-ENMaximum voluntary ventilation testingPAGE 28/39
1Click on Start to begin the test.2Verify the volume signal is perfectly horizontal.2AClick on Stop button.2BVerify the patient is not connected to the valve and then click onZero in order to measure the zero of the flow transducer.2CVerify the volume signal is now perfectly stable.Ask to the patient to connect his mouth to the antibacterial filter. Verify there isno leak between his mouth and the filter.The patient breathes with maximal breathing pattern. Highest tidal volume andfrequency.345After 20 to 30 seconds, ask to the patient to breath normally.6Click on Stop to finish the test.The values are displayed in the results table, under “Test 1” column.6.2 Quality controlThe quality control is based on the ATS-ERS criteria: Acceptability criteria:o Tidal Volume should be about 50% of VC.o Respiratory rate (RR) should be close to 90 breaths per minute.o Ratio MVV/(40 x FEV1) 0,80 indicates a submaximal effort. Repeatability criteria:o At least two acceptable maneuvers.o Difference between two acceptable values lower than 20%.S1-ENMaximum voluntary ventilation testingPAGE 29/396If the signal is horizontal, it means the zero of the flow transducer hasbeen measured correctly. Go to step 3.If the signal is not horizontal, it means the zero of the flow transducer hasnot been correctly measured.
66.3 Reviewing the test1Automatic selection for calculation of the MVV. Edit the analysis time intervaland then click on the calculator for the MVV calculation in 1 minute.2Manual selection of the analysis range.2APut the limits of the analysis area.2BSlide left or right the selected area.3Comment/interpretation editing mode.4Click on this button to see the report before printing.S1-ENMaximum voluntary ventilation testingPAGE 30/39
7 Minute tidal ventilation testing77.1 Performing the testS1-ENMinute tidal ventilation testingPAGE 31/39
1Click on Start to begin the test.2Verify the volume signal is perfectly horizontal.If the signal is horizontal, it means the zero of the flow transducer hasbeen measured correctly. Go to step 3.If the signal is not horizontal, it means the zero of the flow transducer hasnot been correctly measured.Click on Stop button.2BVerify the patient is not connected to the valve and then click onZero in order to measure the zero of the flow transducer.2CVerify the volume signal is now perfectly stable.72A3Ask to the patient to connect his mouth to the antibacterial filter. Verify there isno leak between his mouth and the filter.4The patient breathes normally in a resting pattern.5After the time defined for this test, the test stops automatically. It is also possibleto finish manually the test by clicking on Stop.The values are displayed in the results table, under “Test 1” column.7.2 Quality controlThere is no ATS-ERS recommendations, but make sure the end-expiratory level is stable.S1-ENMinute tidal ventilation testingPAGE 32/39
77.3 Reviewing the test1Define the duration of the test.2Review different displays of the flow/volume curve.3Comment/interpretation editing mode.4Click on this button to see the report before printing.S1-ENMinute tidal ventilation testingPAGE 33/39
8 Studied parameters8.1 Slow spirometry8.1.1 Measured parametersDefaultunitLLLLssDescriptionTidal VolumeVital CapacityInspiratory Reserve VolumeExpiratory Reserve VolumeInspiratory cycle TimeTotal cycle Time8ParameternameTVVCIRVERVTiTtot8.1.2 Calculated atio of the Inspiratory over Total cycle TimeRF#/minRespiratory rateS1-ENDescriptionFormulaInspiratory CapacityExpiratory CapacityTV IRVTV ERVTiTtot60TtotStudied parametersP
option for most the Medisoft instruments (Micro 5000, Micro 6000, HypAir, SpiroAir, BodyBox), it allows to measure all the lung volumes that can be mobilized, including tidal . Clinical research . S1-EN General information PAGE 7/39 2 2.3 Contraindications Relative contraindications for spirometry include hemoptysis of unknown origin, .